* Approved by CPG Committee; PIC endorsement pending
See also
Diabetic ketoacidosis
Diabetes mellitus and surgery
Diabetes mellitus: management of unwell children with established diabetes at home
Diabetes mellitus: new presentation not in diabetic ketoacidosis
Glucagon for severe hypoglycaemia
Hypoglycaemia
Key points
- Test for blood ketones in all unwell children with established diabetes, as ketone levels may be raised even in normoglycaemia eg starvation ketosis in gastroenteritis
- Long-acting (basal) insulin should never be omitted in children with diabetes, even when unwell, fasting or hypoglycaemic
- Vomiting should be considered a sign of insulin deficiency/hyperglycaemia in a child with known diabetes
BGL and ketone interpretation in type 1 diabetes
|
BGL |
Ketones |
| Hypoglycaemia |
≤3.9 mmol/L |
|
| Normal pre-meals |
4-7 mmol/L |
<0.6 mmol/L |
| Normal post-meals |
4-10 mmol/L |
<0.6 mmol/L |
| High |
>11 mmol/L |
≥0.6 mmol/L |
| Very High |
>15 mmol/L
(check ketones) |
>1 mmol/L
(insulin required) |
Background
- Children with type 1 diabetes mellitus (T1DM) may present unwell due to an intercurrent illness, or in the setting of hyperglycaemia, hypoglycaemia and/or ketosis
- Insulin requirements may increase, leading to hyperglycaemia if doses are not adjusted
- in acute illnesses
- following surgical procedures
- during treatment with corticosteroids
- Insulin requirements may decrease, leading to hypoglycaemia, if there is
- limited oral intake
- increased fluid losses eg gastroenteritis
- Hyperglycaemia, fever, excessive glycosuria and ketonuria all contribute to increased fluid losses, leading to risk of dehydration
Assessment
History
- Nature of intercurrent illness and symptoms
- Duration of diabetes (how long since diagnosis)
- Current insulin type, dosage and insulin regimen
- Typical total daily dose (TDD) of insulin (see table in Additional notes below)
- Glucose levels and blood ketone levels over the previous 1-2 days
- Ability to tolerate oral fluids/food
- Consider other precipitants for
- Hypoglycaemia: excessive insulin dosing, missed meals, exercise, alcohol ingestion
- Hyperglycaemia: insulin omission, poor insulin adherence, dietary factors, problems with injection method, problems with injection site (lipoatrophy/lipohypertrophy)
- Usual sick day management plan
Examination
Management
Goals of treatment
- Exclude Diabetic ketoacidosis (DKA)
- Fluid management
- Treat hypoglycaemia, ketonaemia or hyperglycaemia and adjust insulin if required
- Monitor blood glucose level (BGL) and ketones
Investigations
- Blood glucose level
- Point of care blood ketones, urine ketones where blood ketones unavailable
- Venous blood gas if BGL or ketones are elevated
- Other investigations as required as part of the workup of intercurrent illness
Treatment
If hyperglycaemic (BGL >11) and pH <7.3 or bicarbonate <18 mmol/L treat as per Diabetic ketoacidosis
Note that some centres use different management guidelines, see local protocols
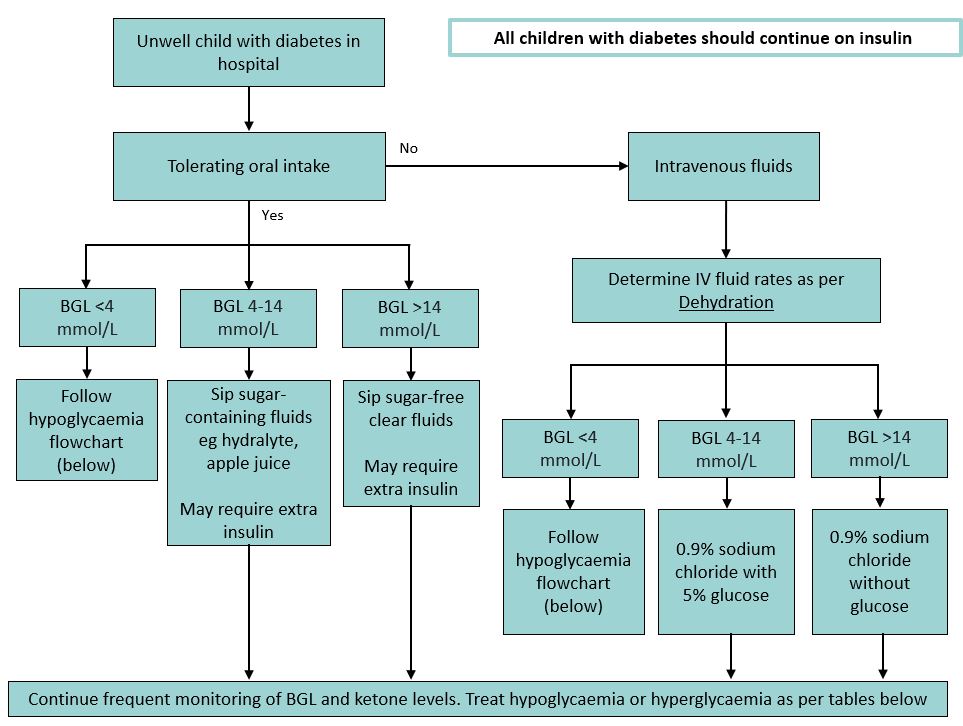
Fluid management for unwell children with diabetes
Hospital management of hypoglycaemia in unwell children with diabetes
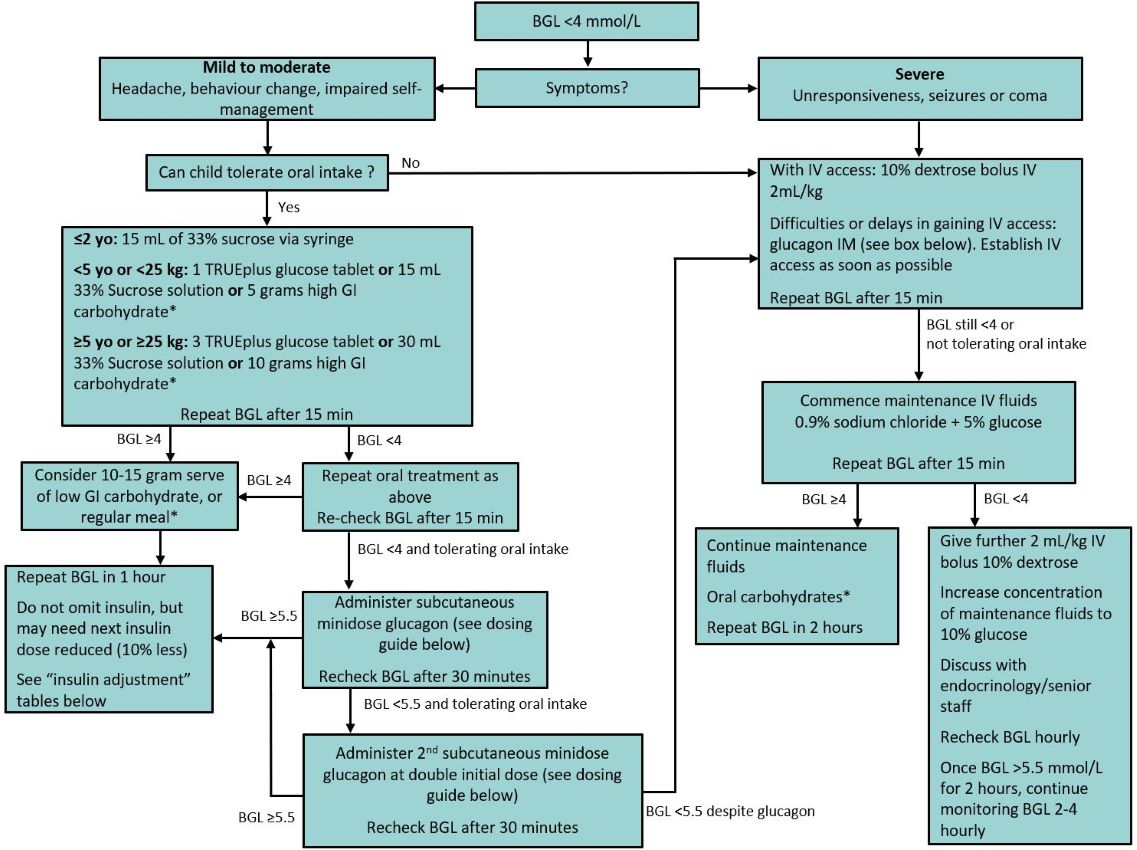
*see Carbohydrate serves box in "Additional notes" for detail. Follow up low GI carbohydrate only required if hypoglycaemic correction occurs outside of a meal-time. If having meal, give usual insulin with meal (additional low GI serve not required)
Intramuscular glucagon dosing for severe hypoglycaemia
If child confused, unconscious or having a seizure
- Inject 1 mL of H2O into the vial containing glucagon 1 mg, gently agitate to dissolve
- Use a syringe to draw up the entire solution (1 mL) from the vial and administer dose depending on weight:
-
<25 kg: give 0.5 mg (half of vial=0 .5 mL)
- >25 kg: give 1 mg (full vial = 1 mL)
- See Glucagon for severe hypoglycaemia
|
Subcutaneous minidose glucagon for rescue hypoglycaemia
- Minidose glucagon is used to manage hypoglycaemia (BGL
<4 mmol/L) in a child with diabetes, when usual oral treatments have been unsuccessful or cannot be tolerated, but the child does not have CNS impairment
- Minidose glucagon avoids the side effects of larger doses of glucagon such as nausea and vomiting
- This can allow the child time to recover sufficiently to tolerate sips of sugar-containing fluid
Minidose glucagon administration:
- Make up glucagon as directed
- Re-constitute the full 1 mg vial in 1 mL of water and then use an insulin syringe to draw up to the 1 'unit' mark on the insulin syringe.
- 1 unit = 10 microg of reconstituted glucagon solution
Minidose glucagon - initial doses for subcutaneous administration
| Age (years) |
Dose of glucagon |
Mark on insulin syringe |
|
<2 |
20 microg (0.02 mg) |
2 unit mark |
| 2-15 |
10 microg per year of age |
1 unit per year of age |
| >15 |
150 microg (0.15 mg) |
15 unit mark |
Insulin adjustments
Where possible, consult the child's usual diabetes care team for advice regarding ongoing insulin adjustments
A suggested approach to insulin adjustments in unwell child with T1DM and normoglycaemia/hypoglycaemia
- Unwell children with diabetes with low/normal blood glucose may need their insulin doses decreased, however insulin should not be omitted
- Children with elevated ketones and low blood glucose are in 'starvation ketosis' and require additional carbohydrate/glucose to normalise their BGL and ketones
| Blood ketone (mmol/L) |
Urine ketone |
Blood glucose levels (mmol/L) |
Frequency of BGL/ketone monitoring |
|
|
<5
If BGL
<4 see Hypoglycaemia flowchart (above)
|
5-10 |
|
|
<0.6 |
Negative/trace |
Reduce TDD* insulin by 20% |
Give usual bolus insulin |
2 hourly |
| 0.6-0.9 |
Trace/small |
Reduce TDD insulin by 15% |
Give usual bolus insulin |
2 hourly |
| 1-1.4 |
Small/moderate |
Reduce TDD insulin by 10% |
Give usual bolus insulin |
2 hourly |
| 1.5-2.9 |
Moderate/large |
Give IV glucose-containing fluids and continue insulin |
Add additional 5% of TDD to ordinary bolus |
1-2 hourly |
| ≥3 |
Large |
Give IV glucose-containing fluids & continue insulin. Insulin may need to be reduced |
Add additional 5% of TDD to ordinary bolus |
1-2 hourly |
| *TDD = total daily dose, based on typical daily dosing schedule. If child uses flexible dosing strategies or family unaware/unsure of usual doses, estimate TDD using 1 unit/kg based on most recent weight. See Additional notes below |
Suggested additional insulin corrections for unwell children with T1DM and hyperglycaemia
- Children with established diabetes who present to hospital with hyperglycaemia and ketosis, but normal pH, need additional subcutaneous insulin to clear their ketones.
- If pH
<7.3 See DKA
Blood ketone
(mmol/L) |
Urine ketone |
Blood glucose levels (mmol/L) |
Frequency of BGL/ketone monitoring |
|
|
10-14 |
15-22 |
>22 |
|
|
<0.6 |
Negative/trace |
Usual treatment dose insulin |
Bolus 5% of TDD* |
Bolus 10% TDD |
2 hourly |
| 0.6-0.9 |
Trace/small |
Bolus 5% TDD
and ensure tolerating oral intake |
Bolus 5% of TDD |
Bolus 10% TDD |
2 hourly |
| 1-1.4 |
Small/moderate |
Bolus 5% TDD
and give extra oral carbs |
Bolus 10% TDD |
Bolus 10% TDD |
2 hourly |
| 1.5-2.9 |
Moderate/large |
Bolus 5% TDD
and give extra oral carbs |
Bolus 10% TDD |
Bolus 20% TDD |
2 hourly |
| ≥3 |
Large |
Bolus 10% TDD
and give extra oral carbs |
Bolus 20% TDD |
Bolus 20% TDD |
1-2 hourly |
| *TDD = total daily dose, based on typical daily dosing schedule. If child uses flexible dosing strategies or family unaware/unsure of usual doses, estimate TDD using 1 unit/kg based on most recent weight. See Additional notes below |
- Repeat additional insulin correction doses as needed every 2-4 hours
- If eating/drinking, give usual rapid-acting insulin for carbohydrate portions as well as the additional correction dose
- Continue usual long-acting/background insulin
Insulin pumps
- If BGL >15 and ketones
<0.6
- Continue basal/background insulin
- Give correction bolus (as above) through child's pump. If eating/drinking, give usual bolus for carbohydrate and additional correction together
- If BGL >15 and ketones ≥0.6
- Assume pump line failure, disconnect
- Give correction bolus (as above) via subcutaneous injection. If eating/drinking, give subcutaneous injection of bolus for carbohydrate and additional correction together
- Change pump cannula and resume basal/background insulin
- If there are any concerns about insulin delivery via the pump, change to subcutaneous injections (in discussion with usual diabetes care team)
Additional notes
Carbohydrate serves
| High GI carbohydrate serves |
Low GI carbohydrate serves |
|
5 grams
If
<5 yo or <25 kg
|
10 grams
If >5 yo or >25 kg
|
10-15 grams
|
Glucose tablets (1 TRUEplus or 3 Glucodin)
50 mL lemonade
100 mL cordial
1 teaspoon honey
2 jellybeans
60 mL juice |
Glucose tablets (3 TRUEplus or 6 Glucodin)
100 mL lemonade
200 mL cordial
2 teaspoon honey
3 jellybeans
120 mL juice |
4-6 savoy biscuits
7-10 rice crackers
1 slice of bread
200-250 mL plain milk
½ cup fruit yoghurt
1 apple
1 small banana |
Calculating total daily dose (TDD) Insulin
This is all the insulin (rapid and long-acting) that a child has in a day.
For example: Background glargine 20 units at night, bolus breakfast typically 8 units, lunch 12 units, dinner 18 units, snack 2 units.
Therefore, daily total = TDD = 20+8+12+18+2 = 60 units
If the child uses flexible dosing strategies or family unaware/unsure of usual doses, estimate TDD using 1 unit/kg based on most recent weight
| Total daily dose (TDD) |
Sick day dose
(rapid-acting insulin in addition to usual doses) |
|
10% |
20% |
| 1-10 units |
1 unit |
2 units |
| 10-15 units |
1.5 units |
3 units |
| 15-20 units |
2 units |
4 units |
| 20-25 units |
2.5 units |
5 units |
| 25-30 units |
3 units |
6 units |
| 30-35 units |
3.5 units |
7 units |
| 35-40 units |
4 units |
8 units |
| 40-45 units |
4.5 units |
9 units |
| 45-50 units |
5 units |
10 units |
| 50-55 units |
5.5 units |
11 units |
| 55-60 units |
6 units |
12 units |
| 60-65 units |
6.5 units |
13 units |
| 65-70 units |
7 units |
14 units |
| 70-75 units |
7.5 units |
15 units |
| 75-80 units |
8 units |
16 units |
Last updated July 2025
Reference List
- Beckles ZL, Edge JA, Mugglestone MA, Murphy MS, & Wales JK (2016). Diagnosis and management of diabetes in children and young people: summary of updated NICE guidance. Bmj, 352.
- Cengiz E, Danne T, Ahmad T, et al. ISPAD Clinical Practice Consensus Guidelines 2022: Insulin treatment in children and adolescents with diabetes. Pediatr Diabetes. 2022;23(8):1277‐1296. doi:10.1111/pedi.13442
- Craig ME, Codner E, Mahmud FH, et al. ISPAD Clinical Practice Consensus Guidelines 2022: Editorial. Pediatr Diabetes. 2022;23(8):1157‐1159. doi:10. 1111/pedi.13441
- Craig ME, Twigg SM, Donaghue KA, Cheung N, Cameron F, Conn J, & Silink M. (2011). National evidence-based clinical care guidelines for type 1 diabetes in children, adolescents and adults. Canberra: Australian Government Department of Health and Ageing,
346
- de Bock M, Codner E, Craig ME, et al. ISPAD Clinical Practice Consensus Guidelines 2022: Glycemic targets and glucose monitoring for children, adolescents, and young people with diabetes. Pediatr Diabetes. 2022;23(8): 1270‐1276. doi:10.1111/pedi.13455
- Phelan, H, Hanas, R, Hofer, SE, et al. Sick day management in children and adolescents with diabetes. Pediatr Diabetes. 2022; 23(7): 912-925. doi:10.1111/pedi.13415
- RCH, Diabetes at the RCH: How to treat low blood glucose levels, https://www.rch.org.au/diabetes/type-1-diabetes-toolkit/How_to_treat_low_blood_glucose_levels/,
accessed 25 November 2024