See also
Head injury
Hypoglycaemia
Trauma - primary survey
Meningitis and encephalitis
Sepsis - assessment and management
Afebrile seizures
Child abuse
Poisoning
Key points
- The aim of immediate management is to minimise ongoing neurological damage while investigation and treatment are initiated
- Parents are the best judge of an altered conscious state, particularly for children with disability
- Consider child abuse in a young child presenting with altered conscious state and signs of injury
Background
- Altered conscious state is a continuum from disorientation and confusion to coma
- Altered conscious state is an uncommon presentation but is associated with significant mortality and morbidity
- Parental and nursing concerns of conscious state should be taken seriously
- Head injury and infection are the most common causes of paediatric coma
- The Glasgow Coma Scale (GCS) or Children’s Glasgow Coma Scale is a semiquantitative measure of conscious state with altered conscious state defined by a GCS of
< 15
- Initial assessment of conscious state may be done using AVPU scale
Causes
Trauma |
Blunt, penetrating head injury, falls, concussion
|
|
Infection
|
Meningitis, encephalitis, sepsis, cerebral and extracerebral abscesses, malaria
|
|
Neurological
|
Epilepsy: Post-ictal phase, status epilepticus
Raised intracranial pressure: Mass lesion, cerebral oedema, blocked ventriculoperitoneal shunt
Cerebral hypoxia, ischaemia: Respiratory failure, shock (cardiogenic, adrenal crisis, sepsis, hypovolaemia), asphyxiation, cerebrovascular event (stroke/intracranial haemorrhage)
|
|
Poisoning/toxin
|
Substance abuse or accidental ingestion (eg alcohol, hallucinogens, opiates, lead)
|
|
Metabolic and endocrine
|
Hypoglycaemia
Diabetic ketoacidosis, renal or hepatic failure, hypo/hypernatremia, hypothermia, inborn error of metabolism
|
|
Other
|
Acute confusional migraine, psychiatric, arrhythmia
|
Assessment
Initial assessment and management
Initial screening of conscious state may be done using AVPU scale, particularly in younger children
- A = Alert
- V = Responds to voice
- P = Responds to pain
- U = Unresponsive
Any impairment on AVPU scale should prompt a formal assessment of GCS
Glasgow Coma Score
| ≥4 years
|
<4 years
|
|
Response
|
Score
|
Response
|
Score
|
|
Eye opening
|
|
Eye opening
|
|
|
Spontaneously
|
4
|
Spontaneously
|
4
|
|
To verbal stimuli
|
3
|
To verbal stimuli
|
3
|
|
To painful stimuli
|
2
|
To pain
|
2
|
|
No response to pain
|
1
|
No response to pain
|
1
|
|
Best verbal response
|
|
Best verbal response
|
|
|
Orientated and converses
|
5
|
Alert; babbles, coos words to usual ability
|
5
|
|
Confused and converses
|
4
|
Less than usual words, spontaneous irritable cry
|
4
|
|
Inappropriate words
|
3
|
Cries only to pain
|
3
|
|
Incomprehensible sounds
|
2
|
Moans to pain
|
2
|
|
No response to pain
|
1
|
No response to pain
|
1
|
|
Best motor response
|
|
Best motor response
|
|
|
Obeys verbal commands
|
6
|
Spontaneous or obeys verbal commands
|
6
|
|
Localises to stimuli
|
5
|
Localises to pain or withdraws to touch
|
5
|
|
Withdraws to stimuli
|
4
|
Withdraws from pain
|
4
|
|
Abnormal flexion to pain (decorticate)
|
3
|
Abnormal flexion to pain (decorticate)
|
3
|
|
Abnormal extension to pain (decerebrate)
|
2
|
Abnormal extension to pain (decerebrate)
|
2
|
|
No response to pain
|
1
|
No response to pain
|
1
|
Regardless of cause of altered conscious state, attend to ABCDE first, see
Resuscitation
If traumatic cause is possible, immobilise cervical spine and consult neurosurgery (
Trauma- Primary survey and
Head Injury)
The aim is then to identify a cause as quickly as possible, to guide investigation and treatment. Where this is not immediately obvious careful history and examination aims to identify coma syndromes, and possible diagnoses
History
- Symptoms: headache, confusion, seizures
- Focal neurology
- Time course of symptoms: abrupt vs gradual deterioration, recurrent episodes
- Injury: mechanism, timing
- Presence of fever
- Past and recent medical history including immunisation, seizures, developmental delay
- Family history including consanguinity
- Drug and toxin exposure: exposure, quantity, timing
- Travel history: personal or that of close family contacts
Examination
| Cardiac |
Pulse rate, volume, blood pressure, perfusion
|
|
Respiratory
|
Saturations, respiratory rate, pattern of breathing, chest injury
|
|
Neurological
|
Signs of raised intracranial pressure:
- unilateral or bilateral pupillary dilatation
- drop of more than 2 points in GCS
- focal neurological signs
- abnormal posturing (decorticate, decerebrate)
- irregular respirations, hypertension and bradycardia (Cushing reflex, a late sign)
Presence of ventricular-peritoneal shunt, encephalopathy
|
|
Gastrointestinal
|
Hepatomegaly, abdominal guarding, rigidity, or tenderness
|
|
Skin
|
Rash, petechiae, bruising, birth marks, sweating, needle marks
|
|
Smell
|
Alcohol, glue, ketones, petrol, phenol
|
|
Head and neck
|
Scalp haematoma, ear/nasal bloody or clear discharge, otitis media, mastoiditis, neck bruising
|
|
Toxins
|
Toxidromes
|
Management
Investigations
Consider the following as guided by your differential diagnoses:
Blood tests
- POCT Glucose
- FBE, renal function, glucose, liver function tests
- Blood gas, ammonia, cortisol
- Coagulation profile
- Urine toxicology
Microbiology
- Blood culture, urine culture
- Lumbar puncture: do not perform in a child with a reduced GCS (see
Lumbar puncture). If required, this can be performed when the child is clinically stable to determine if meningitis, encephalitis, or other neurological condition (such as autoimmune encephalitis etc) are present
Imaging
- CT or MRI (where feasible and only after initial resuscitation and treatment) in suspected trauma, stroke or concerns regarding raised intracranial pressure
Cardiac
- ECG eg broad QRS suggestive of critical tricyclic antidepressant toxicity
Treatment
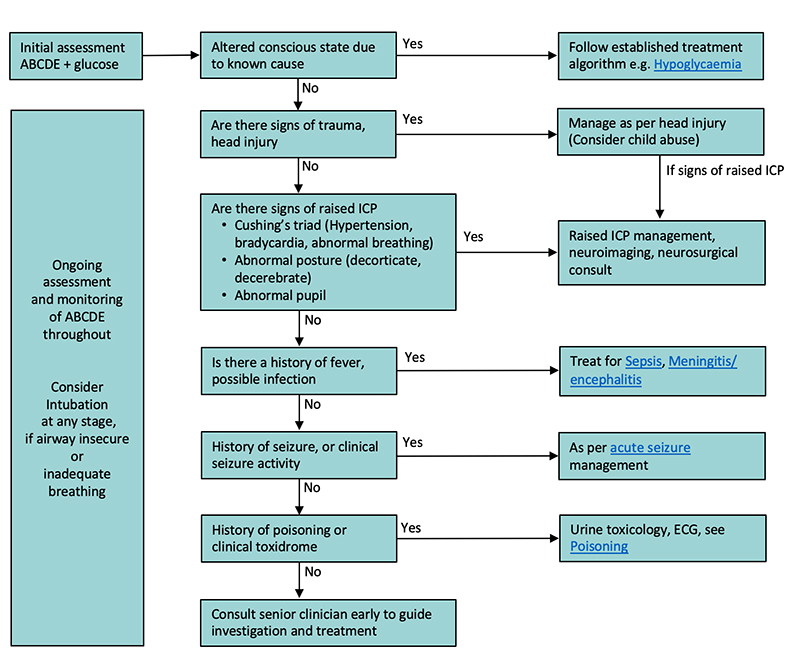
Approach to management of altered conscious state based on suspected cause
Consider consultation with local paediatric team when
- Any child who presents with persistent or unexplained altered conscious state
- When there are concerns for child abuse
Consider transfer when
Child is at risk of deteriorating and requires management beyond the capability of available local services
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Consider discharge when
- The child’s conscious state has returned to normal
- There is clear plan for ongoing follow up if required
Parent information
Head injury
Meningitis
Seizure
Last updated November 2022