Major paediatric trauma – Primary survey
Major paediatric trauma - Secondary survey
Cervical spine assessment
Key points
The priorities when assessing a child with head injury are to identify those with:
- Moderate to severe head injury who need immediate management, urgent investigation and referral
- Mild head injury who can be immediately discharged home
- Head injury who need observation and/or neuroimaging
- Other significant injuries or suspected
child abuse
Background
- Most head injuries are mild
- A head injury may still be significant without loss of consciousness
- Consider non-accidental injury, especially in infants (See
child abuse)
- Infants and non-verbal/non-ambulant children have a higher risk of inflicted head injury
- Non-verbal children, particularly those under 6 months, require a more cautious assessment approach and may require longer observation
- Children with suspected drug or alcohol intoxication may be more difficult to assess – assume conscious level relates to injury and have a lower threshold for referral and neuroimaging
- Concurrent cervical spine assessment is required
Assessment
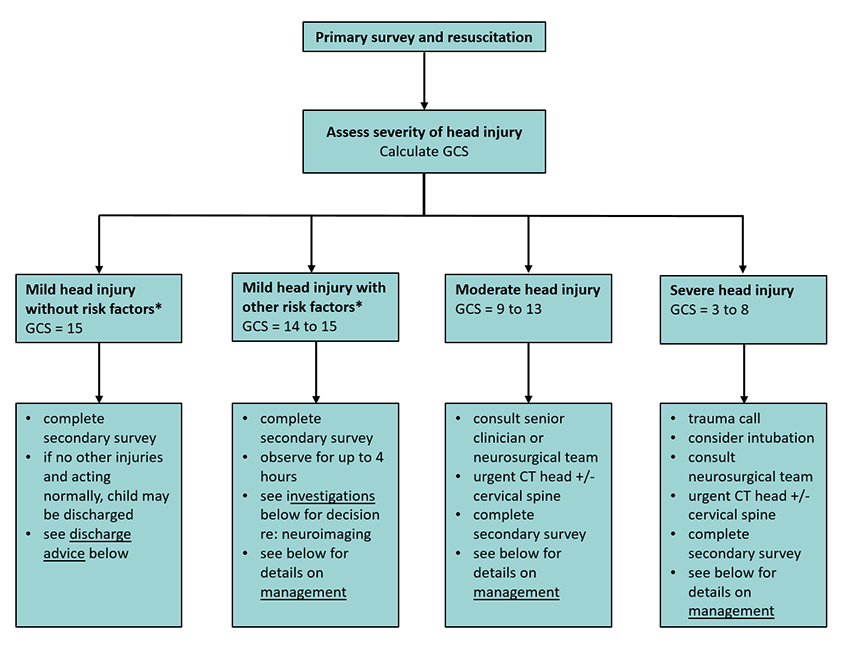
Initial assessment of severity
- Determines those that can be discharged promptly, versus those that need a period of observation or those requiring active management
- Severity may change – all children being observed should be regularly reassessed for signs or symptoms of deterioration
*Risk factors:
- Severe headache
- Persistent altered mental status/acting abnormally
- Abnormal neurology
- Suspected child abuse
- Palpable skull fracture
- Signs of base of skull fracture
- Non-frontal scalp haematoma (occipital, parietal or temporal) in child
<2 years
- Severe mechanism
- Post-traumatic seizure
- Loss of consciousness
- Persistent vomiting
- Known bleeding disorder/anticoagulation
- Ventriculoperitoneal shunt
- Neurodevelopmental disability
Primary survey and resuscitation:
Glasgow Coma Score (GCS)
| ≥4 years |
<4 years |
|
Response |
Score |
Response |
Score |
|
Eye opening |
|
Eye opening |
|
|
Spontaneously |
4 |
Spontaneously |
4 |
|
To verbal stimuli |
3 |
To verbal stimuli |
3 |
|
To painful stimuli |
2 |
To pain |
2 |
|
No response to pain |
1 |
No response to pain |
1 |
|
Best verbal response |
|
Best verbal response |
|
|
Orientated and converses |
5 |
Alert; babbles, coos words to usual ability |
5 |
|
Confused and converses |
4 |
Less than usual words, spontaneous irritable cry |
4 |
|
Inappropriate words |
3 |
Cries only to pain |
3 |
|
Incomprehensible sounds |
2 |
Moans to pain |
2 |
|
No response to pain |
1 |
No response to pain |
1 |
|
Best motor response |
|
Best motor response |
|
|
Obeys verbal commands |
6 |
Spontaneous or obeys verbal commands |
6 |
|
Localises to stimuli |
5 |
Localises to pain or withdraws to touch |
5 |
|
Withdraws to stimuli |
4 |
Withdraws from pain |
4 |
|
Abnormal flexion to pain (decorticate) |
3 |
Abnormal flexion to pain (decorticate) |
3 |
|
Abnormal extension to pain (decerebrate) |
2 |
Abnormal extension to pain (decerebrate) |
2 |
|
No response to pain |
1 |
No response to pain |
1 |
History
Past history
- Bleeding tendency, anticoagulation or antiplatelet therapy
- VP shunt
Injury
- Timing
- Mechanism of injury
Severe mechanism includes:
- motor vehicle accident with patient ejection or rollover, death of another passenger
- pedestrian or cyclist struck by motor vehicle
- falls of ≥1 m (<2 yr)
- fall >1.5 m (>2 yr)
- head struck by high impact object
- Circumstances of injury, eg accident, suspected child abuse, unexplained fall (consider
syncope), intoxication
Clinical course and associated symptoms
- Stable, deteriorating, improving
- Loss or impairment of consciousness and duration
- Abnormal behaviour, including agitation, confusion and drowsiness
- Headache
- Nausea and vomiting
- Other injuries sustained
- Presence of amnesia
- Post injury seizure
Examination
- Neurological examination, including signs of raised intracranial pressure:
- unilateral or bilateral pupillary dilatation
- drop of more than 2 points in GCS
- development of focal neurological signs
- abnormal posturing
- Irregular respirations, hypertension and bradycardia (Cushing reflex – late sign)
- Feel specifically for palpable skull fractures
- Look for signs of fractured base of skull (haemotympanum, cerebrospinal fluid otorrhoea or rhinorrhoea, periorbital bruising (raccoon eyes), bruising over mastoid area (Battle sign))
- Assess for other injuries (see
secondary survey)
Management
Investigations
Neuroimaging
- The need and timing of neuroimaging requires balancing the clinical benefit with the risk of radiation exposure and sedation – discuss with a senior doctor or neurosurgeon
- For children with mild head injury, a decision about whether to image should be based on the presence or absence of risk factors (as described below)
- Indications for neuroimaging may be present on initial assessment, or may evolve during the period of observation
Risk factors as indications for imaging
| Definite indications |
Relative indications (if more than one, observe child and consider neuroimaging) |
- Any moderate or severe head injury (GCS ≤13)
- Focal neurological deficit
- Signs of base of skull fracture
- Palpable skull fracture
- Suspected non-accidental injury
- Persistent signs of altered mental status (agitation, drowsiness, repetitive questioning, slow response to verbal communication)
|
- GCS persistently 14
- Severe mechanism of injury
- History of loss of consciousness
- Post-traumatic seizure
- Severe headache
- Persistent vomiting
- Non-frontal scalp haematoma (<2 years)
- Acting abnormally as per parent (<2 years)
|
Neuroimaging for children with special conditions
Children with any of the following conditions, although not at increased risk of intracranial injury, require greater consideration of neuroimaging:
- Age
<6 months
- Bleeding disorder, or taking either anticoagulation or anti-platelet therapy
- Immune thrombocytopenia
- Ventriculoperitoneal shunt
- Neurodevelopmental disorders
- Drug or alcohol intoxication
If no other risk factors are present, structured observation may be considered over immediate neuroimaging. Seek advice from a senior clinician, haematologist or other relevant subspecialist
Type of neuroimaging
- Plain skull X-ray or head ultrasound should not be performed in lieu of a CT
- MRI may be equivalent in terms of clinical utility, but should only be considered in settings where it can be performed quickly and safely
Consider other investigations
If other injuries are present, investigate as clinically indicated
Consider investigation for causes of falls eg alcohol, other ingestions, arrhythmias, hypoglycaemia
(see Syncope)
Treatment
Mild head injury without other risk factors
- GCS 15 and meets the following criteria:
- no concern about abusive head trauma
- age over 6 months
- no special conditions (bleeding tendency, neurodevelopmental disorder, VP shunt)
- non-severe mechanism
- If on the basis of history and examination there are no other clinical concerns, the child has returned to normal conscious state, and is acting normally, they may be discharged to the care of their parents
- Treat pain with simple analgesia
- Ensure discharge advice given to parents
Mild head injury with other risk factors
- Child should be observed for up to 4 hours post injury, with:
- 30-minutely neurological observations (conscious state, PR, RR, BP, pupils and limb power) for the first 2 hours
- one-hourly neurological observations thereafter
- Treat pain with simple analgesia
- Consider anti-emetics
- A persistent headache, ongoing vomiting, GCS of 14 or persistent altered mental status requires further observation and likely investigation. Discuss with a senior clinician
- The child may be discharged home if there is return to normal conscious state for at least one hour, is acting normally, and they can tolerate oral fluids
Concussion and return to activity
- A concussion is a mild injury which temporarily alters brain function
- Post concussive symptoms are common, and advice should be given regarding rest and gradual return to activity (See parent information)
Moderate head injury
- Consult a senior doctor or neurosurgeon for advice
- Urgent CT of head (and consideration of imaging of c-spine if relevant)
- Ensure early specialist consultation
- Low threshold to escalate care as per severe head injury below
Severe head injury:
- Look for signs of severe head injury which may include presence of focal neurological deficit, signs of increased intracranial pressure or signs of basal skull fracture
- The initial aim of management of a child with a serious head injury is prevention of secondary brain damage
- The key aims are to maintain oxygenation, ventilation, and circulation, and to avoid rises in intracranial pressure (ICP)
- Urgent CT of head (and consideration of c-spine imaging if relevant)
- Ensure early neurosurgical consultation
- Cervical spine movement should be minimised until formal assessment occurs. See Cervical spine assessment
Intubation and ventilation
- Consider intubation if:
- Child unresponsive or not responding purposefully to pain
- GCS persistently
<8
- Loss of protective laryngeal reflexes
- Respiratory irregularity or suspected hypoventilation
- Avoid hypotension, hypoventilation and hypoxia during intubation and minimise cervical spine movement. See Cervical spine assessment
- If possible, a neurological examination should be performed before intubation and any motor deficits or cranial nerve signs documented
- Intubation should be performed by the most skilled clinician available. For children requiring mechanical ventilation:
- Analgesia and sedation with morphine and midazolam should be administered by careful titration. Children with head injury are often more sensitive to opioids
- Consider muscle paralysis (eg pancuronium or vecuronium)
Maintain circulation and cerebral perfusion
- Uncorrected hypotension is a significant factor in secondary brain damage
- Ensure adequate blood pressure with crystalloid infusion (eg 0.9% sodium chloride) or inotropes if necessary
- isotonic fluids (eg 0.9% sodium chloride) recommended (see
Intravenous fluids)
Treat signs of raised intracranial pressure
In consultation with neurosurgical team, consider measures to decrease intracranial pressure:
- Maintain head position: Nurse 30 degrees head up (after correction of shock) with head in midline position to help venous drainage
- Ventilate to PaCO2 35-40 mmHg
- Consider hypertonic saline (sodium chloride 3% 3 mL/kg IV over 10-20 min) or 20% mannitol (0.25-0.5 g/kg IV over 20-30 min)
Control seizures
- Treat with benzodiazepines to immediately control seizures
- Seek neurosurgical advice early
- Give phenytoin or levetiracetam loading dose
- Observe closely for subsequent hypotension or hypoventilation and manage appropriately
- See afebrile seizures
Other measures:
- Maintain normal sodium and glucose levels
- Maintain normothermia
- Check for coagulopathy
Consider consultation with local paediatric or paediatric neurosurgical team when
- Failure to return to normal within 4 hours
- Suspected
child abuse. Consult child protective and forensic medical service
- Uncertainty surrounding when to perform neuroimaging
- Any child with a ventricular shunt
- Any child with a bleeding disorder, or who is taking anticoagulant or anti-platelet therapy (discuss with paediatric haematologist)
Consider transfer to a tertiary centre when
- All severe head injuries
- Suspected inflicted head injury
- Deteriorating conscious level (especially motor response changes)
- Focal neurological signs
- Seizure without full recovery
- Definite or suspected penetrating injury
- Cerebrospinal fluid leak
- Child requiring care beyond the comfort level of the hospital
For emergency advice and paediatric or neonatal ICU transfers, call Retrieval Services
Consider discharge when
- The child is acting normally for at least one hour as per the parent, has a normal neurological examination and can tolerate fluids
- There are no other factors warranting admission or longer observation (eg other injuries or underlying medical concerns, drug and alcohol intoxication, social factors, possible abusive head injury)
Concussion and return to activity
- A concussion is a mild injury which temporarily alters brain function
- Post concussive symptoms are common, and advice should be given regarding rest and gradual return to activity (See parent information)
Parent advice and follow-up
- Ensure the parents have clear instructions regarding the management of their child at home, and when to seek medical attention
- Children discharged following a mild to moderate head injury should consider follow-up with a primary care doctor within 1 to 2 weeks to assess post-concussive symptoms
- Advise parents that children with anything other than a trivial head injury may take up to 4 weeks to recover, and
graded return to activity is recommended
Parent information sheets
Concussion and mild brain injury
Head injury - general advice
Head Injury - Return to school and sport
Raising Children Network Concussion
Concussion in Sport Australia
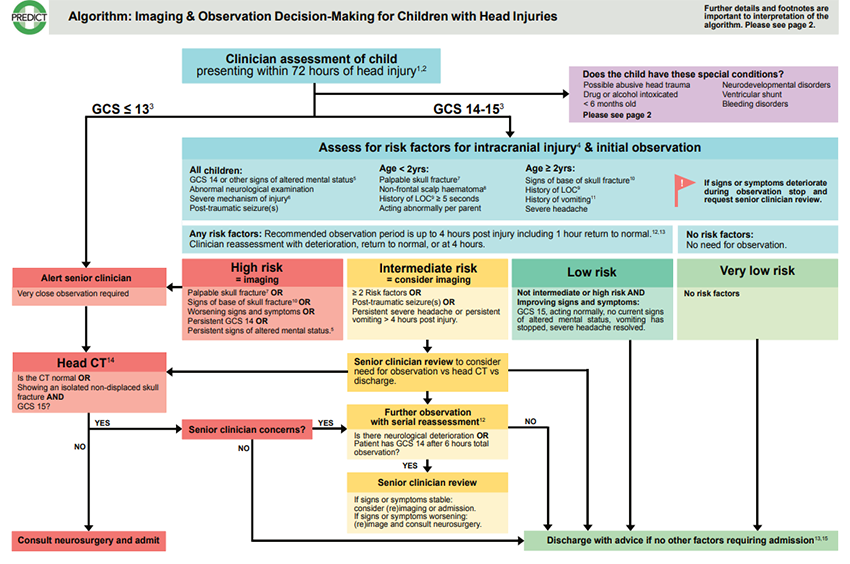
Additional information
For additional guidance regarding management of mild to moderate head injuries, the Paediatric Research in Emergency Departments International Collaborative (PREDICT) has developed the following algorithm (available
here with further details to aid interpretation):
Last Updated November 2021