IV fluids - for children beyond the newborn period
See also
Resuscitation: Care of the seriously unwell child
Dehydration
Maintenance Fluids Calculator
Follow specialised fluid guidance for:
Key points
- Whenever possible, the enteral route should be used
- In most situations, the preferred fluid type is sodium chloride 0.9% (with glucose 5% +/- potassium for maintenance fluid)
- Most sick children will retain water and require less than full maintenance fluids
- Serial weights are the best measure of acute changes in fluid status
Background
- This guideline only applies to children aged 1 month to 18 years who cannot receive enteral fluids. Whenever possible the enteral route should be used
- Fluids with a similar sodium concentration to plasma are most appropriate
- Safe use of IV fluid in children requires careful prescribing and monitoring
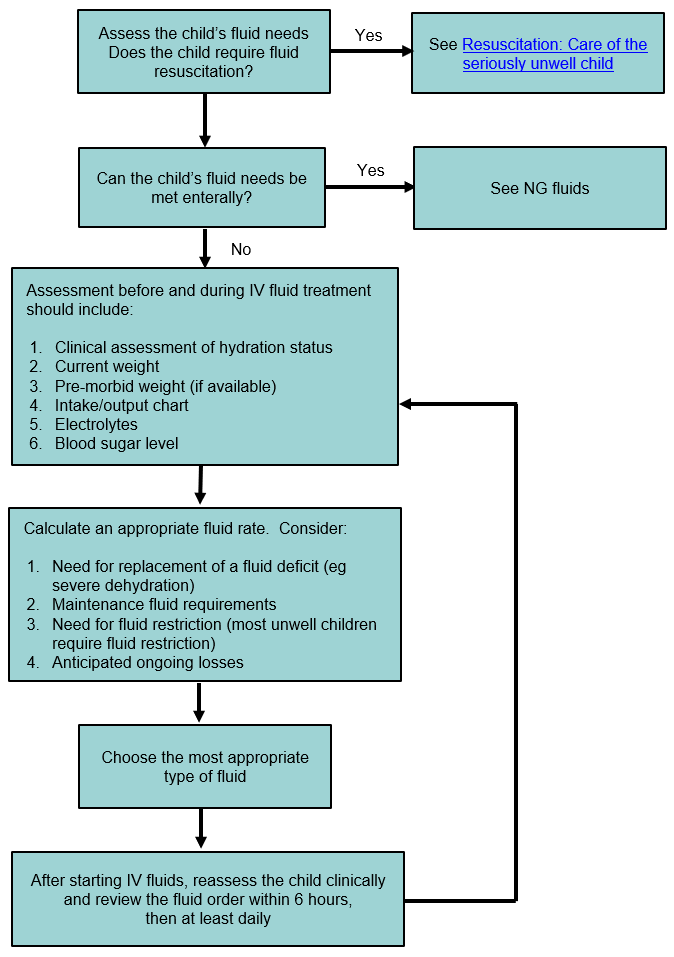
See flowchart outlining approach to safe IV fluid prescription
- Check the compatibility of IV fluid with any IV drugs that are being co-administered
Assessment
Red flags
- Abnormal serum sodium
<135 mmol/L or >145 mmol/L (or significant change of >0.5 mmol/L/hr on a repeat measure) – see
hyponatraemia or
hypernatraemia and notify senior clinician
- Consider increased antidiuretic hormone (ADH) secretion - especially with acute CNS and pulmonary conditions, although any unwell child is at risk
- Short gut or other significant gastrointestinal pathology
- Fluid resuscitation >20 mL/kg required
- Situations where specialised fluid management is required (see list above)
Examination
Hydration Status
- Assess for
dehydration
- Signs of fluid overload including oedema (eg periorbital, genital, sacral, peripheral) should also be evaluated, especially in children already receiving IV fluid treatment
Weight
- All children on IV fluids should be weighed at the start of treatment and then at least daily
- Children with severe dehydration or ongoing losses need to be weighed more often
Management
Investigations
Serum electrolytes and glucose
- All children should have serum electrolytes and glucose checked before starting IV fluid treatment and at least every 24 hours if IV fluids are continued at more than 50% maintenance
- For more unwell children and children with large fluid losses or abnormal electrolytes, check the electrolytes and glucose 4-6 hours after starting fluid therapy, and then according to the clinical situation
Fluid Balance
- Repeated weights are the best measure of fluid status. Also document intake/inputs and ongoing losses (including urine output), with at least 12 hourly subtotals
Treatment
Resuscitation Fluid
For treatment of shocked children, see
Resuscitation: Care of the seriously unwell child
Treat shock with bolus IV fluids to restore circulatory volume:
|
Give a bolus of 10–20 mL/kg of sodium chloride 0.9% as fast as possible, and reassess to determine if additional IV fluid is required
Do not include this fluid volume in subsequent calculations |
Alternative resuscitation fluids such as Plasma-Lyte 148, Hartmann's, packed red blood cells, or albumin may sometimes be used on senior advice
Rehydration
To restore hydration, the
degree of dehydration must first be calculated. For children with mild or moderate dehydration, enteral (oral or NG) rehydration is preferable. IV fluid rehydration may be required for children with severe dehydration or those who cannot tolerate enteral intake
Calculation of Fluid Requirements
|
Total fluid requirement = Maintenance + Replacement of deficit + Replacement of ongoing losses |
Calculating fluid deficit
|
The most accurate way to calculate a child's fluid deficit is:
Deficit (mL) = [Premorbid weight (kg) minus current weight (kg)] x 1000
If a pre-morbid weight is not available, use:
Deficit (mL) = weight (kg) x % dehydration x 10 |
Replace deficit over 24–48 hours
- For children with ≤5% dehydration, replace deficit in the first 24 hours
- For children with >5% dehydration, replace deficit more slowly. Replace the 5% deficit in the first 24 hours and the remainder over the following 24 hours
- Serial clinical assessment of hydration status must be made at regular invervals for all children with dehydration
(See worked example under the flowchart below)
If electrolytes are deranged, consult senior clinician and relevant guideline, and consider slower replacement of deficit
Ongoing Fluid Losses
Ongoing losses should be measured and replaced if clinically indicated, based on each previous hour (if significant) or 4-hour period (eg a 200 mL loss over the previous 4 hours is replaced by giving 50 mL/hr for the next 4 hours)
Gastrointestinal tract losses are commonly replaced with sodium chloride 0.9% + potassium chloride 20 mmol/L
Maintenance
Full maintenance fluid rates may be calculated using the table below as a starting point. This calculation applies for well children only. Fluid rates need to be adjusted for ALL unwell children
Weight (kg) |
Full maintenance mL/day |
mL/hour |
|
3–10 |
100 x weight |
4 x weight |
|
10–20 |
1000 plus 50 x (weight minus 10) |
40 plus 2 x (weight minus 10) |
|
20–60 |
1500 plus 20 x (weight minus 20) |
60 plus 1 x (weight minus 20) |
|
>60 |
2400 mL/day is the normal maximum amount |
100 mL/hour |
This calculation:
- Estimates the volume required per kg to maintain hydration in healthy children
- Accounts for insensible losses (from breathing, through the skin, and in stool)
- Allows for excretion of the daily excess solute load (urea, creatinine, electrolytes, etc) in a volume of urine with similar osmolarity to plasma
Note:
The maintenance fluid requirement calculation in this table applies to all ages including young infants. Babies need a higher volume of enteral milk (150–180 mL/kg/day) to meet nutritional and growth requirements, but this higher volume should not be used as a basis for intravenous fluid prescribing
Intravenous fluid prescribing for an infant should be based on the water requirement (ie 100 mL/kg/day up to 10kg and then adjust as clinically indicated (eg restrict to 2/3 maintenance)
Fluid Restriction
2/3 maintenance rates should be used in most unwell children unless they are dehydrated. Unwell children are likely to secrete excess ADH so will need less fluid to avoid water overload and hyponatraemia
Children with the following conditions are at high risk of excess ADH secretion and may require further fluid restriction – seek senior advice:
- Acute CNS conditions (meningitis, tumours, head injuries)
- Pulmonary conditions (pneumonia, bronchiolitis, mechanical ventilation)
- Post-operatively and in trauma
Hourly fluid rates can be calculated using this
Maintenance fluids calculator or the table below.
|
Weight (kg) |
Full maintenance (mL/hour)
Well child eg fasting for elective surgery |
2/3 maintenance (mL/hour)
Most unwell children unless dehydrated |
|
5 |
20 |
13 |
|
10 |
40 |
27 |
|
15 |
50 |
33 |
|
20 |
60 |
40 |
|
25 |
65 |
43 |
|
30 |
70 |
47 |
|
35 |
75 |
50 |
|
40 |
80 |
53 |
|
45 |
85 |
57 |
|
50 |
90 |
60 |
|
55 |
95 |
63 |
|
≥60 |
100 |
67 |
Choice of Fluid
The preferred fluid type for IV maintenance is sodium chloride 0.9% with glucose 5%
Alternative maintenance fluid options include:
- Plasma-Lyte 148 with glucose 5% (contains 5 mmol/L of potassium) - generally stocked in tertiary paediatric centres and intensive care
- Hartmann's with glucose 5%
Glucose 5% should be given in maintenance fluids for children with no other source of glucose
High glucose containing fluids
- Glucose 10% (+/- additional sodium chloride) is often used in neonates and sometimes used in children with metabolic disorders. See worked calculation (at bottom of page) for how to prepare
IV fluid containing glucose 10%, however wherever possible pre-mixed bags should be used. Always follow local injectable guidelines
- Glucose 15–20% solutions are very occasionally used in neonates and in children with metabolic disorders. These should ideally be given via central venous access
- >20% glucose solutions are rarely required in children; inappropriate use can cause severe adverse events. Only use in an ICU setting in discussion with senior staff
The inclusion of potassium in maintenance fluids
- Should be considered once normal baseline electrolytes and renal function have been confirmed
- Use premixed fluid bags containing potassium
- Avoid the addition of concentrated solutions (sodium chloride, potassium chloride or glucose) to bags of fluid, unless there is a clinical need, as this is a safety risk
- The standard concentration for most circumstances is 20 mmol/L of potassium chloride
Non-standard fluids
- Should only be prescribed with clear clinical indication, in consultation with a senior clinician
- Check the serum sodium and blood glucose regularly
Hypotonic Fluids containing a sodium concentration less than plasma are NOT recommended for routine use in children. These fluids are associated with morbidity/mortality secondary to hyponatraemia
- Do NOT give glucose 4% with sodium chloride 0.18%
- Sodium chloride 0.45% solutions are only rarely indicated. If necessary, they should be prescribed in consultation with a senior clinician
Consider consultation with local paediatric team when
- Unsure of which/how much fluid to use
- Electrolyte abnormalities
- Using a non-standard fluid
- Significant co-morbidities are present
- Fluid resuscitation >20mL/kg required
Consider transfer when
Children with severe electrolyte or glucose abnormalities
Shock requiring ≥40 mL/kg IV fluid boluses
Children requiring care above the level of comfort of the local hospital
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Approach to IV fluid prescription
Worked example for fluid replacement
An infant with severe gastroenteritis requires fluid rehydration and is not tolerating enteral fluids. A decision is made to proceed with IV fluid treatment
The infant weighed 10 kg prior to this illness but her current weight is 9 kg. She has clinical signs consistent with severe dehydration of 10%
|
The most accurate way to calculate a child's fluid deficit is:
Deficit (mL) = [Premorbid weight (kg) minus current weight (kg)] x 1000
If a pre-morbid weight is not available, use:
Deficit (mL) = weight (kg) x % dehydration x 10 |
To calculate the fluid deficit volume for this infant:
| Fluid deficit (mL) |
= [10 kg – 9 kg] x 1000 |
| |
= 1000 mL |
In the first 24 hours replace 5% dehydration. For this infant that is 500 mL (ie 500 mL ÷ 24 = 20.5 mL/hr). Replace the remaining deficit (here another 500 mL ÷ 24 = 20.5 mL/hr) if still indicated after clinical reassessment, over the following 24 hours.
Next you calculate the infant's maintenance fluid requirement and check it using the
calculator:
| Hourly maintenance rate (mL/hr) |
= 4 x pre-morbid weight (kg) |
| |
= 40 mL/hr |
| Total fluid requirement = Maintenance + Replacement of deficit + Replacement of ongoing losses |
| The starting total hourly fluid rate |
= 40 mL/hr + 20.5 mL/hr |
| |
= 60.5 mL/hr |
A re-assessment of the child's fluid status, including any ongoing losses, should be completed within 6 hours
Additional notes/other considerations
Electrolyte content of intravenous fluids
|
Fluid |
Na
mmol/L |
Cl
mmol/L |
K
mmol/L |
Ca
mmol/L |
Lactate
mmol/L |
Mg
mmol/L |
Acetate
mmol/L |
Gluconate
mmol/L |
Glucose
% |
Osmolality
mOsm/L |
|
Normal human plasma |
135 - 145 |
96 - 106 |
3.5 – 5.0 |
2.1 – 2.6 |
0.5 – 1.8 |
0.7 – 1.2 |
0 |
|
3.5 – 8.0 |
275 –
295 |
|
Sodium chloride 0.9% |
154 |
154 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
308 |
|
Sodium chloride 0.9% + glucose 5% |
154 |
154 |
0 |
0 |
0 |
0 |
0 |
0 |
5 |
586 |
|
Sodium chloride 0.9% + glucose 5% + potassium 20 mmol/L |
154 |
174 |
20 |
0 |
0 |
0 |
0 |
0 |
5 |
626 |
|
Plasma-Lyte 148 +
glucose 5% |
140 |
98 |
5 |
0 |
0 |
1.5 |
27 |
23 |
5 |
584 |
|
Compound Sodium Lactate (Hartmann's) |
130 |
110 |
5 |
2 |
30 |
0 |
0 |
0 |
0 |
274 |
|
Sodium chloride 0.45% + glucose 5%
* |
77 |
77 |
0 |
0 |
0 |
0 |
0 |
0 |
5 |
428 |
|
*Note – Fluids with a sodium concentration
<125 mmol/L are not recommended for routine use |
Worked calculation to convert 5% glucose to 10% glucose
IV fluid bags contain a significant overfill volume; a 1 L Baxter brand bag of 5% glucose contains an average volume of 1035 mL (51.75 grams of glucose). To prepare a 10% solution, withdraw 120 mL from the 1 L bag of 5% glucose and discard. Add 110 mL of 50% glucose. The final solution will contain 100 grams in 1025 mL (approximately 10% glucose)
Last updated October 2020