See also
Meningitis and encephalitis
CSF interpretation
Key points
- The decision to perform a lumbar puncture (LP) should be discussed with a senior clinician
- In a seriously unwell child, prioritise urgent antibiotic administration over performing LP
- LP should only be performed after a thorough neurological examination and once contraindications have been considered
- Careful preparation, adequate analgesia/anaesthetic/sedation and an experienced assistant are key to success
Background
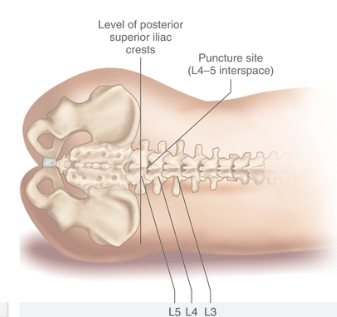
- LP is performed at or below the L4 level (the conus medullaris finishes near L3 at birth, but at L1-2 by adulthood)
- It is preferable to obtain a CSF specimen prior to antibiotic administration. However, antibiotics must not be delayed more than 30 minutes in a child with signs of meningitis or sepsis
- In a child with fever and purpura in whom meningococcal infection is suspected, LP may not change the management and may cause deterioration
- In term infants, the seated position has been shown to be the best tolerated and to also have the best chance of obtaining CSF
- If LP is unsuccessful on two occasions, refer to a senior colleague, reassess the need for LP and consider image guidance to assist
- CT scans are not helpful in most children with meningitis. A normal CT scan does not exclude raised intracranial pressure (ICP) and brain herniation may occur even in the presence of a normal CT scan
Assessment
Informed consent from carers should include discussion of benefits and potential complications. The parent LP information sheet is useful when talking to parents about the procedure
Indications
Contraindications
Absolute
- GCS <8 or deteriorating/fluctuating level of consciousness
- Signs of raised intracranial pressure: diplopia, abnormal pupillary responses, decerebrate or decorticate posture, low HR + elevated BP + irregular respirations, papilloedema
Note: a bulging fontanelle in the absence of other signs of raised ICP is not a contraindication to LP
Relative
- Septic shock or haemodynamic compromise
- Significant respiratory compromise eg apnoeic episodes
- New focal neurological signs or seizures
- Seizure within previous 30 min and/or ongoing decreased conscious state following a seizure
- INR >1.5 or platelets <50 x 109/L for child on anticoagulant medication
Note: abnormal vital signs eg tachycardia or tachypnoea are not contraindications to LP
Complications
- Failure to obtain CSF, or traumatic bloody tap (common)
- Pain/discomfort during procedure (consider sedation, local anaesthetic and analgesia)
- Post-dural puncture headache (uncommon, 5-15%)
- Transient or persistent paraesthesia/numbness (very uncommon)
- Respiratory arrest from positioning (rare)
- Infection introduced by needle causing meningitis, epidural abscess or osteomyelitis (very rare)
- Spinal haematoma (very rare)
- Spinal epidermoid tumour (extremely rare, significantly reduced risk using needle with stylet)
- Brain herniation (extremely rare in the absence of contraindications above)
Procedure
Staff
- Proceduralist
- At least one assistant to hold the child
Equipment
- Sterile gloves
- Sterile drapes and procedure tray
- Skin preparation: 2% chlorhexidine + 70% isopropyl alcohol or povidone iodine solution (Betadine®). In neonates and extremely premature babies, use specialised solutions to avoid burning the skin eg 0.1% chlorhexidine
- Local anaesthetic 1% lidocaine, 2 mL syringe and 25-30G needle if local infiltration indicated
- Spinal needle of appropriate length
- Sterile CSF tubes
- Certain neurological or metabolic conditions may require special tubes eg for neurotransmitters, discuss with local pathology service
- Spinal manometer and three-way tap if opening pressures are required

Figure 1. Set up equipment using aseptic technique
Spinal needles
- Use a 22 or 25G bevelled spinal needle with stylet (the use of needles without a stylet has an associated rare risk of spinal epidermoid tumours)
- Consider using 25G pencil point needles for older children/adolescents to reduce the risk of headache, evidence is not convincing in younger children
Age of child |
Weight of child (kg) |
Median spinal cord depth (cm) |
Length of needle (cm) |
Neonates and infants |
1-5 |
0.9-1.7 |
2 |
12-18 months |
10 |
2.4 |
3 |
4 years |
15 |
2.6 |
3 or 4 |
6 years |
20 |
2.8 |
4 |
9 years |
30 |
3.2 |
4 |
12 years |
40 |
3.6 |
5 |
14 years |
50 |
4 |
5-6 |
Median spinal cord depth has been correlated with weight
Neonates and infants (mm) = 2 x weight (kg) + 7, children (mm) = 0.4 x weight (kg) + 20
Analgesia
- Ensure acute pain management including non-pharmacological techniques
- Child Life Therapy services where appropriate and available
- Local anaesthetic if possible
- Ideally topical anaesthetic cream (EMLA®,AnGel®or LMX4®) for 45-60 minutes prior to LP, except where specimens are required urgently
- Consider subcutaneous 1% lidocaine (max 4 mg/kg) for children >12 months
- Use oral sucrose for infants
- Consider nitrous oxide for children >12 months (or younger with senior clinician involvement) note this may affect opening pressures if manometry required
- Other sedation should be discussed with a senior clinician
Monitoring
- Cardiorespiratory and oxygen saturation monitoring
Position
- Keep neonate or infant under warmer, ideally on Resuscitaire® or similar
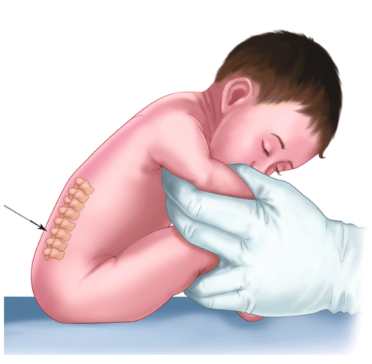
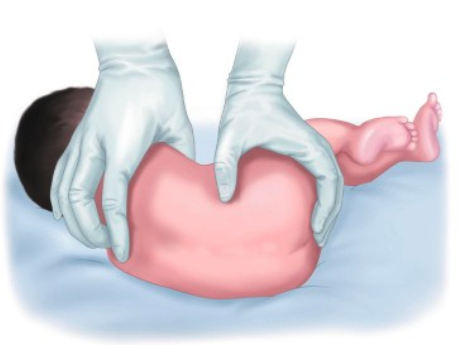
- LP may be performed with the child sitting up or lying on their side (with proceduralist’s dominant hand at caudal end)
- Position back and bottom close to edge of bed
- Aim for maximum flexion of spine (curl into fetal position), but avoid over-flexing neck, especially in infants, as this may cause airway obstruction and respiratory compromise
 |  |
|
| Figure 2. Sitting position | Figure 3. Lateral decubitus |
- Position plane of the back at 900 to the bed and make sure hips and shoulders are in line with each other
- Draw an imaginary line between the top of the iliac crests. This intersects the spine at approximately the L3-4 interspace (mark this if necessary)
- Aim for the L3-4 or L4-5 interspace
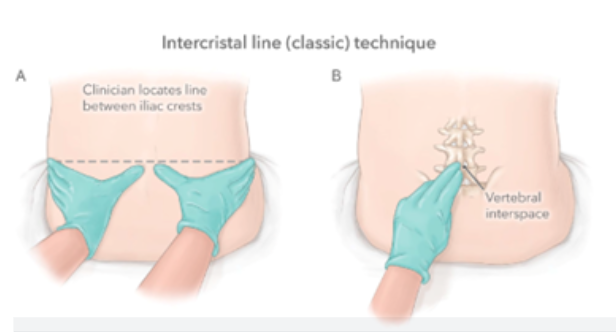 |  |
| Figure 4 and 5. Identifying landmarks | |
Preparation
- Obtain and document parental consent. This should include a discussion of the benefits of the procedure in terms of possible diagnoses, and potential complications (see above)
- Remove topical anaesthetic cream
- Proper interpretation of CSF glucose requires paired blood glucose level to be collected. Ideally, collect the blood glucose prior to LP
- Put on mask
- Wash hands and aseptically put on sterile gloves ± gown
- Prepare skin and set up sterile drapes
- Allow adequate time for skin preparation to dry
- Take tops off tubes, ensuring that they remain sterile
- Infiltrate skin with 1% lidocaine using a 25-30G needle (smaller needle is less painful, but increases difficulty of infiltration) if local anaesthetic appropriate
Lumbar puncture
- Position needle in midline, with bevel pointing to the side if child sitting, or towards ceiling if child lying
- Pierce skin with needle and pause to ensure child is still
- Check child's position and adjust if necessary
- Angle needle aiming for umbilicus
- Advance needle into spinous ligament, where there will be increased resistance
- Firm resistance and inability to advance needle is likely due to bony obstruction and requires withdrawal and repositioning of needle
- Continue to advance needle slowly within ligament until there is a fall in resistance (this may not be obvious in neonates)
- Remove stylet
- If CSF is flowing:
- collect 2-4 numbered sterile tubes
- 5-10 drops in each is usually adequate, but more may be required depending on investigations ordered. 10 drops = 0.5 mL
- If CSF is flowing very slowly, rotate needle 90 degrees
- If blood-stained fluid is flowing:
- collect some for culture. If fluid "clears", it can be used for a cell count, which is best performed on final tube collected
- consider whether blood may be due to sub-arachnoid haemorrhage
- if it does not "clear", another attempt at a different level may be required
- If CSF is not flowing:
- replace the stylet and advance (or withdraw and reposition) the needle slightly, then re-check for CSF
- it is possible to reposition and reangle needle multiple times, each time reviewing position of child and needle position
- multiple attempts may lead to local swelling and bruising
- After CSF collection or failed attempt:
- replace stylet (to reduce risk of headache), and remove needle and stylet together
- apply brief pressure to puncture site
- Send specimens urgently to lab
Post procedure care
- Cover puncture site with occlusive dressing
- Bed-rest following LP is of no benefit in preventing headache in children
- Perform further vital signs and neurological observations as indicated by sedation used and child's clinical state
- Document in patient record
- analgesia and anaesthetic use
- needle length and gauge
- number of attempts required
- description of CSF appearance
Consider consultation with local paediatric team when
Unsure whether LP should be performed
Consider transfer when
Child is unwell above the comfort level of the hospital
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services.
Consider discharge when
Appropriate investigation/treatment has been completed and any necessary follow-up plan is in place
Parent information
Lumbar puncture (NSW)
Lumbar puncture (SA)
Lumbar puncture (Vic)
Lumbar puncture (WA)
Additional notes
Holding for a lumbar puncture - infant
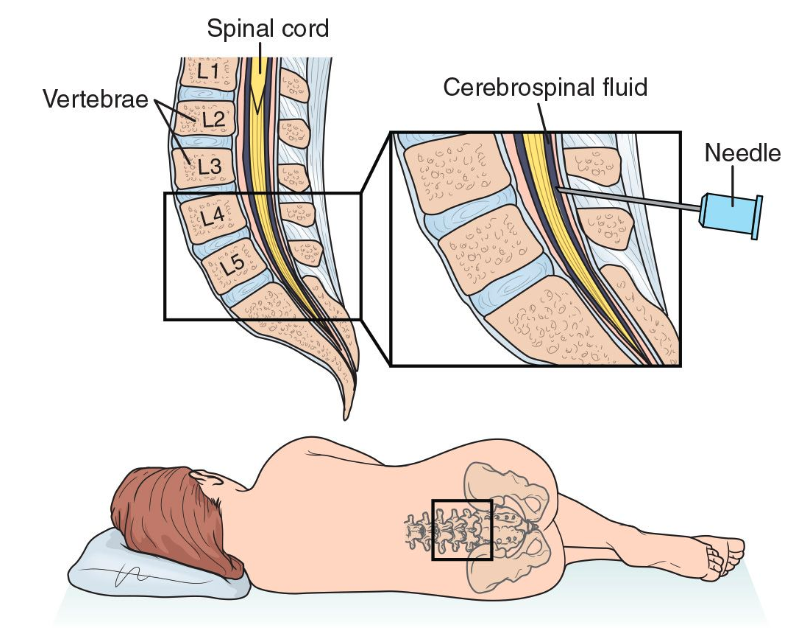
Figure 6. Spinal insertion point
Last updated December 2024