What is pain?
Pain is an
unpleasant sensory and emotional experience that arises from actual or potential tissue damage. Pain assessment
and treatment in the acutely injured child is challenging in the context of
multiple factors impacting patient presentation and competing treatment
priorities. Nevertheless, untreated or under-treated pain following trauma
leads to complications, such as hypoventilation, reduced oxygenation, increased
stress response, increased cardiovascular output and muscle tension and
rigidity. Pain also interferes with sleep, rest and healing.
Assessing pain in injured children
Pain assessment
in the injured child is difficult. In younger patients, pain and distress might
be indistinguishable. Acutely injured and traumatised children may not
cooperate with pain assessment, especially in the absence of a parent or
guardian. Intoxication, collar immobilisation, head injury and need for
ventilation can further complicate pain assessment.
Pain self-report should be sought but
may not always be attainable for the above reasons or simply due to
developmental stage. Regardless of the chosen approach, it is important to:
- Be systematic;
- Choose a developmentally appropriate pain
assessment tool;
- Document findings, act and reassess.
Regular
pain assessment is associated with improved pain management and increased
satisfaction from patients, families and healthcare professionals. Consistent use
and staff familiarity with a chosen assessment tool within individual centers is key to successful pain
management, along with reassessment following analgesic intervention.
Pain assessment tools
- Many
different types of pain-assessment tools exist, and they are discussed
separately below.
- Ideally
the pain tools used should have a common numeric for consistency and clarity
(e.g. all out of 10).
- To
get the best results from pain assessment tools, they should be explained to
the child rather than just being shown, and a response should be expected, eg
“This is a way for you to tell me about how much pain you have. It shows from
no pain to a lot of pain. Can you show me how much pain you have at the
moment?” will produce better results than, “What’s your pain score?”
Self report or Numeric rating scale
- For children over 7 years,
who are verbal and numerate
- Ask the child if he/she has
any pain.
- Explain the scale and ask the
child to rate the severity of their pain.
- Using numeric rating scales
or self report is more difficult during severe acute pain episodes. Instead try
asking, “Do you have no pain, a little pain or a lot of pain?” or use a Faces
or Behavioural Pain Scale.
*Used with permission of the U.S. Agency for Healthcare
Research and Quality (AHRQ), successor to the Agency for Health Care Policy and
Research (AHCPR).
Practical point: Showing the
child a numeric rating scale (0-10, where 0 is no pain and 10 is the worst
pain) will make this easier than if the child has to imagine a scale.
Faces pain scale
- For verbal children aged 4 to
12 years
- Ask the child if he/she has
any pain.
- Explain the scale and ask the
child to rate the severity of their pain.
- The Faces Pain Scale can be found at www.iasp-pain.org/FPSR
Practical point: Older children who are less numerate may prefer to use a Faces
Pain Scale over a Numeric Scale. Children under 3 years can rarely use faces
scales, but many young children can still give a basic report of “a little
sore” or “hurts a lot”.
Behavioural pain scale
- For children who cannot self-report
- The FLACC Scale is recommended for pain assessment in young children with acute pain
FLACC scale
Each category (face,
legs, activity, cry, consolability) is scored separately on a 0-2 scale, for a
total score between 0 and 10.
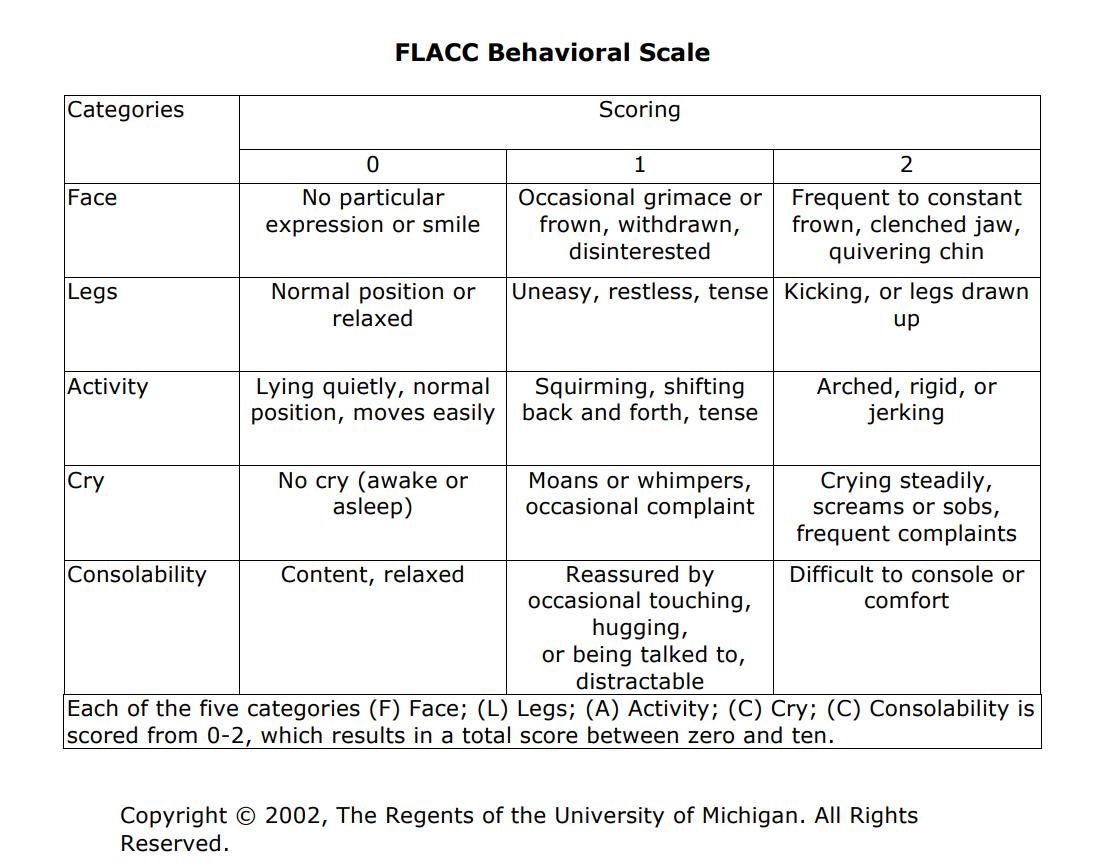
Practical
point: The FLACC scale is also a useful tool
for older children who cannot self-report, such as children with cognitive
impairment or intellectual disability. Caregivers may also provide valuable
insight in the assessment of these patients.
Children’s pain assessment tools (FPS-R,
Numeric Rating Scale and FLACC) are available from RCH on small pink laminated
cards that fit onto staff IDs. These cards cost $3 and can be purchased from
the Child Health Information Centre, ph 03 9345 6429 or at www.rch.org.au/chas/
Behavioural signs of pain
Behavioural
signs of pain may be seen only briefly after the onset or worsening of pain and
can quickly return to normal. These include:
- Facial expressions such as frowning,
grimacing, clenched teeth or jaw.
- Body position or postures such as guarding,
cradling or protecting a limb, muscle rigidity, restlessness,
clenching of hands, foetal position.
- Vocalisations
such as crying, moaning, whimpering or screaming.
Practical
Point: Disabled children may already have
altered body position and posture. Often, these are exaggerated in the presence
of pain. Some children will display none of these expected behaviours for fear
of painful intervention. The following table details the developmental
characteristics of children’s responses to pain.
Developmental characteristics of children's responses to pain [1],[2]
|
Young Infants
|
- Generalised
body response of rigidity or thrashing, possibly with local reflex withdrawal
of stimulated area.
- Loud
crying
- Facial expression of pain
(brows lowered and drawn together, eyes tightly closed, mouth open and
squarish)
|
|
Older Infants
|
- Localised body response
with deliberate withdrawal of stimulated area
- Loud crying
- Facial expression of pain and/or anger
(same facial characteristics as pain but eyes may be open)
- Physical resistance, especially pushing the
stimulus away after it is applied
- Localised body response
with deliberate withdrawal of stimulated area
- Loud crying
- Facial expression of pain and/or anger
(same facial characteristics as pain but eyes may be open)
- Physical resistance, especially pushing the
stimulus away after it is applied
|
Young Children
|
- Loud crying, screaming
- Verbal expressions of “Ow” “Ouch” or “It
hurts”
- Thrashing of arms and legs
- Attempts to push the stimulus away before
it is applied
- Uncooperative, needs physical restraint
- Requests termination of procedure
- Clings to parent, nurse or other
significant person
- Requests emotional support, such as hugs or
other forms of physical comfort
- May become restless or irritable with
continuing pain
- All these behaviours may be seen in
anticipation of actual painful procedure
|
|
School-Age Children
|
- May see all behaviours of
young child, especially during painful procedure but less in anticipatory period.
- Stalling behaviour, such as “Wait a minute”
or “I’m not ready”
- Muscular rigidity, such as clenched fists,
white knuckles, gritted teeth, contracted limbs, body stiffness, closed
eyes, wrinkled forehead
|
|
Adolescents
|
- Less vocal protest
- Less motor activity
- More verbal expression, such as “It hurts”
or “You’re hurting me”
- Increased muscle tension and body control
|
Absence of these signs does NOT mean the
child has no pain.
Physiological
signs of pain
Physiological signs of pain may be seen
only briefly after the onset or worsening of pain and can quickly return to
normal. Some of these signs include: tachycardia, hypertension, tachypnoea, sweating, dilated pupils,
sweating and skin colour changes. In the trauma setting, these physiological
signs can be due to many causes other than pain such as shock, hypovolaemia,
anxiety, fear or anger.
Practical Point: Physiological signs[G1] are most useful to assess procedural pain, where there is a obvious
relationship in time between the painful stimulus and observed changes.
Absence
of these signs does NOT mean the child has no pain.
Parents’
input
Ask the parent or caregiver about their child’s responses
and
behaviour. You may ask:
- How does your child normally behave?
- What sort of temperament does your child
have?
- How does your child usually respond to pain
or stressful situations?
- Do you think your child is in pain? How much?
It is important to acknowledge that some
parents or caregivers may have never seen their child experiencing severe pain
before, so may not recognise the signs. Caregivers and medical staff have been
scientifically shown to underscore pain when compared to the individual child’s
score. Parents may also underestimate their child’s pain due to other factors:
fear of opioids, not wanting their child to have any drugs, their own feelings,
past experiences with pain and pain management, wanting their child to be
brave, or relief that you are caring for their child.
Managing pain in injured children
Pain management in the trauma setting
should be integrated to the systematic approach outlined in this manual. In the
case of moderate to severe trauma, where the findings of the primary survey mandate
IV access, IV opioids will be the analgesic method of choice. The intraosseous
route may also be used in these patients. Non-opioid analgesics should be used
for their opioid-sparing effect. Paracetamol should be administered orally to patients
that are conscious and stable; the IV formulation can be used in severely
injured patients. NSAIDs are contraindicated in acute moderate to severe trauma
as their use can lead to platelet dysfunction and renal impairment if renal
blood flow is compromised. However, oral ibuprofen can be administered if there
is no concern for bleeding or potential for renal injury.
Principles of pain management
The general
principles of pain management in children, as per WHO guidelines (2012)[3], are the following:
-
Use analgesic treatments in two steps
according to the child’s level of pain severity:
- for mild pain, use paracetamol and
ibuprofen as first options
- for moderate to severe pain, an
opioid should be considered
- Treat
pain at regular intervals:
- children should receive regular
analgesia for persistent pain, as opposed to administration on “as needed” basis
- “rescue doses” should be available for intermittent and breakthrough pain
- Treat pain by the appropriate route:
- analgesics should be administered
to children by the simplest, most effective, and least painful
route
- when IV access is not required
but the patient experiences severe pain, such as with isolated limb
injury, intranasal fentanyl is a good alternative to IV morphine
- IM injections are NOT recommended for analgesia following trauma (painful administration and
variable absorption in haemodynamic
compromise)
- Tailor
pain treatment to the individual child:
- opioid analgesics should be titrated on an individual basis as there is
no predictable or maximal correct dose
- use
other pain reduction methods tailored to specific injury (see Analgesia for specific situations section below)
- use non-pharmacological methods such as distraction (see Helping children with pain)
Analgesics table
|
Analgesic
|
Route
|
Loading or dose titration
|
Continued dosing
|
Maximum acute dosing
|
|
Paracetamol
|
PO/IV
|
20 mg/kg (max 1g)
|
15 mg/kg (max 1g) 4 - 6hourly |
60 mg/kg/day (max 1g) 6 hourly
|
|
Ibuprofen
Age > 6 months
|
PO
|
10 mg/kg (max 400mg)
|
10 mg/kg (max 400mg) 6-8 hourly with meals
|
400mg 8 hourly - higher doses (up too 800mg) may be used in the
post-operative setting
|
Oxycodone
|
PO
|
0.1 – 0.2 mg/kg (max 5–10mg)
|
0.1 - 0.2 mg/kg (max 5-10mg) 4 hourly
|
Usual max 5-10mg 4
hourly; higher and/or more frequent doses may be used
|
Morphine
|
IV
|
0.1 – 0.2 mg/kg (titrate to max 5-10mg)
|
Titratable increments eg
of 0.025-0.05mg/kg
|
10mg max dose, in severe
pain / in larger children higher dosing is used
|
|
Fentanyl
|
IN
|
1.5 mcg/kg
(max 75 mcg)
|
0.5 - 1.5 mcg/kg
(max 75 mcg) 10 minutely
|
3 mcg/kg
|
|
IV
|
0.5-1mcg/kg (titrate to max 50-100mcg)
|
0.25 - 0.5 mcg/kg
|
2 mcg/kg
|
|
Drug
|
Route
|
Dose
|
Comment
|
|
Amethocaine
|
Topical |
Ametop - max 1g in children over 1 month |
Leave for 30-60 minutes
Superior to EMLA®
for IV insertion
|
|
EMLA®
|
Topical
|
Max 2g/16cm2 for infants over 3
months
(risk of methaemoglobinaemia)
|
Leave for 60 minutes
|
|
Lignocaine
|
Infiltration
|
Max dose
4mg/kg (without
adrenaline)
7mg/kg (with adrenaline)
1ml of 1% = 10mg
|
Onset of effect 5-10 minutes
|
|
Bupivacaine
|
Infiltration
|
Max 2mg/kg
1ml of 0.5% = 5mg
|
Femoral nerve block lasts
4-6 hours
|
Giving
Opioids Safely
Parenteral opioids are the gold standard for pain management in moderate to severe trauma.
Morphine is the most common first line choice as it is readily available. Patients
may have received opioids during pre-hospital care and further doses may be
titrated.
Giving
opioids by intravenous bolus:
- Ensures rapid onset of effect, within 5-10
minutes
- Is
the best route for rapid relief of pain, particularly following trauma.
- To
administer, divide the dose and give in increments, titrating to effect.
- Adjust
the dose if sedatives already given as may precipitate respiratory depression
- Give
with caution if low BP, hypovolaemia or shocked, but do NOT withhold.
Giving
opioids by intranasal route
- Has
similar onset of effect to intravenous route
- Is
the best route if no IV cannula is present, but requires more patient
cooperation
- Is
less readily titratable than via IV route
Monitoring after administering opioids:
Includes the following observations:
- Sedation
level (an early sign of central nervous system depression)
- Respiratory
rate: rate, depth and effort +/- O2 saturations,
keeping in mind that respiratory depression is a late sign
- Heart
rate
- Pain
score
Practical point: If the patient is still in pain after receiving a
loading dose, assuming there is no airway compromise or reduced level of
consciousness, further IV opioids may be titrated. Further doses of morphine
should be given at no less than 10-minute intervals, using 10-20% of the
loading dose. Repeat loading may be indicated if pain is severe.
Management of opioid-induced
respiratory depression (OIRD) or ventilatory impairment (OIVI)
If respirations are depressed:
- Stop
administering opioid
- Stimulate
the patient (shake gently, call by name, ask to breathe)
- Administer
oxygen
- If
required, administer low dose naloxone (Narcan) : 2mcg/kg, (maximum 100mcg)
If patient cannot be roused or is
apnoeic following opioids:
- Administer
resuscitation dose of naloxone (Narcan): 10mcg/kg IV (max 400mcg)
- Can
be repeated once after 2 minutes (max 800mcg)
- Monitor
patient closely
- May need to be repeated every 20–60 minutes due to naloxone’s short duration of action
Other agents
Ketamine
- Used
as second-
or third-line analgesic agent in the major trauma ED setting, usually in children aged 2 years and
above (avoid in children <12 months)
- Analgesic loading dose
= max 0.5mg/kg IV; continued dosing 0.1-0.2 mg/kg IV every 10 min (ie. 10%
of an anaesthetic dose)
Benzodiazepines
- Used for their
muscle relaxant, anxiolytic, and sedative properties (eg.escalating distress not
responding to opioid titration)
- Midazolam has a rapid
onset and provides antegrade amnesia
- Midazolam dose = 0.05-0.1mg/kg
IV (max 5mg); 0.5mg/kg PO (max 20mg)
Analgesia for specific situations
IV insertion/venipuncture
- EMLA or amethocaine gel prior to
procedure (see table above), if time allows
- Coolsense device (where available) cools the
skin and is effective within minutes of application
Eye examination
- Amethocaine 0.5% drops (+/-
cycloplegic to reduce iris spasm)
Nasopharynx
- Co-phenylcaine spray or lignocaine spray
Indwelling
urinary catheters
- Lignocaine
gel (male AND female)
Wounds
- Lignocaine infiltration to site
Practical point: Reduce pain of
injection of local anaesthesia by using the smallest possible needle, warming
the solution and injecting slowly.
Drain
insertion
- EMLA or amethocaine gel prior to procedure, if time allows
- Lignocaine infiltration to site
- Consider
procedural sedation (see procedural section below)
Limb
fractures
- Immobilise with splint or
traction
- Elevate limb when possible or find most comfortable positioning
- IN fentanyl provides rapid relief for severe pain prior/without IV access
- Consider performing a femoral nerve block for fractured femur, ideally using bupivacaine (eg 1.5 - 2mg/kg) for longer duration.
Burns
- First aid instruction is to cool the burnt area for 20minutes
in cool running water. Then apply plastic (cling) wrap to burn
wound to aid analgesia
- IN fentanyl or IV morphine are good options to provide rapid analgesia
- Consider procedural sedation (see
procedural section below) to apply or change dressing
- See also Clinical practice guideline: Burns management
Practical point: In
the setting of fractures and circumferential burns, compartment syndrome must be considered if pain and opioid
requirements increase rapidly.
Head injury
- Assess whether presentation
is due to pain vs. confusion
- Consider IV paracetamol as
a first line intervention where available and then titrate small increments of
IV morphine to effect
- Take particular care with the use of morphine if hypotensive, hypovolaemic,
shocked and deteriorating conscious state
Ventilated
patients
- Patients may require sedation to tolerate ETT
- Consider the following infusions, especially if paralysed:
- Morphine 10-40mcg/kg/h or Fentanyl 0.3-1.2mcg/kg/h, and
- Midazolam 1-4mcg/kg/min
For details on preparation, see: www.monashchildrenshospital.org/for-health-professionals/resources/resuscitation/ or www.rch.org.au/anaes/pain_management/Opioid_Infusion/
Non pharmacological management of pain
The following list outlines what can be done to help children manage their pain.[4]
- Having a parent or other special person
present. Children feel
more secure
with their parents there.
- Simple, accurate information about
what is going on. Explain things slowly, in very small bits and repeat as
often as needed.
- Children should be helped to ask questions
and express feelings.
- Giving a child some control over
treatment. For example, a child who decides whether to sit in a lap or a chair
for an injection will probably feel less pain than a child that has no
choice.
- Deep and steady breathing can help
reduce pain and allow the child some control.
- Distracting the child from the pain.
Talking, video games, breathing exercises, blowing bubbles, television,
music, pop-up books, reading and being read to, are all distractions.
- Use the child’s imagination to change
from being anxious and frightened to being relaxed and calm.
Focusing the child’s attention on a familiar past activity, or telling or
reading a favourite story, can help.
- Use suggestions for pain relief, such
as, “Let the pain just drain away down and out of your body into the bed and
away…good…that‘s it, let it go.” Use the child’s own language and the
child’s favourite activities or experiences.
- Playing/being silly. Children relax
and forget about their worries when they play.
- Relaxation is useful for adolescents.
Special teaching can be given by a psychologist, nurse or other health
professional. Relaxation can reduce anxiety, nausea and vomiting and pain.
- Comforting touch. This includes
stroking, swaddling, holding, rocking, caressing, cuddling and massaging. Cuddling
is nature’s own pain remedy.
- Heat, cold and vibration can relieve
pain. Ice wrapped in a cloth eases some disease and procedural pain. Heat is
useful for muscle pain. Vibration, either by gentle tapping or some
other mechanical method, can block pain.
- Positive feedback. Remind the child
“you are doing great” or “we’re nearly finished”.
Things that don’t help with
the pain and can make it worse[4]:
- Lying to
children about
painful procedures.
- Ridiculing or making fun of the child
by saying things like “Only babies cry”.
- Using needles as a threat. Lies and
threats teach children to distrust and be fearful.
- False reassurance. Saying it wont hurt
when you know it will.
- Having very high expectations of the
child. It’s not useful to make expectations so high that children feel
stressed by them.
- Talking about the feelings too much.
Saying “I know you’re worried/scared” may lessen the child’s
coping ability.
- Focusing too much on the pain or
potential pain. Saying “it will really hurt a lot” is a bad idea. Firstly it might
not; secondly it encourages children to expect the worst.
PROCEDURAL SEDATION
Once stabilised,
trauma patients may require sedation for procedures to be performed in the
acute setting. Procedures suitable for procedural sedation include vascular
access, laceration repair, burn dressing, chest drain insertion, fracture
reduction and foreign body removal.
Nitrous oxide
- Can be used as
sole agent for procedures associated with pain and anxiety
- Has the advantage
of rapid onset and offset of effect along with amnestic properties
- Increased risk of airway
complications in children less than 2 years
- Should be combined
with an analgesic to perform very painful procedures
- Use of nitrous
oxide at 50-70% concentration is safe
- Can lead to expansion of trapped air:
avoid in chest trauma (where there is a possibility of a pneumothorax) and in head injury if there is a risk of intracranial air (pneumocephaly).
For details, see: www.rch.org.au/clinicalguide/guideline_index/Nitrous_Oxide_Oxygen_Mix/
Ketamine
- Potent sedative,
amnestic, analgesic and anaesthetic agent
- Does not reduce respiratory drive at standard doses
- Increased risk of airway complications in children less than 12 months
- Requires the presence of a an airway-competent physician
- Loading dose of 1-1.5 mg/kg IV over 1-2 min, further incremental
doses of 0.5mg/kg IV if sedation is inadequate or
longer sedation is necessary
For details, see: www.rch.org.au/clinicalguide/guideline_index/Ketamine_use_in_the_emergency_department/
OTHER CONSIDERATIONS
The need for pain management in paediatric
trauma extends beyond the acute presentation. Subacute to long-term issues
related to pain include some of the following:
Opioid tapering and wean
- Once able to
tolerate oral intake, patients can transition from parenteral to oral opioids
- For transition to
oral opioid, calculate total IV morphine dose equivalent given in last 24h
- If greater than 0.5 mg/kg/day of IV morphine equivalent was given, 50-80% the total dose is given as long-acting
with an immediate-release opioid prescribed as a rescue.
The ratio to covert to oral morphine from IV is 3 times and to convert to oral
oxycodone is 2 times.
- Targin is a long acting formulation with less
constipating side effects (CR Oxycodone in combination with CR
naloxone) and is used in preference to CR Oxycodone =Oxycontin (where
available).
- MS Contin granules are used preferentially when nasogastric or
nasojejenal tube is the route for administration.
- Major trauma
victims may have received parenteral opioids over a prolonged period and are at risk of
withdrawal. These patients should be weaned from oral opioids by 10-20% per day over
5-10 days.
Neuropathic pain
- Trauma victims can
experience neuropathic pain secondary to thermal or mechanical nerve injuries.
- Antineuropathic
medications can reduce opioid requirements in nociceptive pain and are more
effective than opioids in neuropathic pain management, such as amitriptyline
0.5-2mg/kg and gabapentinoids eg gabapentin 5-10mg/kg bd to tds.
- Dose reduction
in renal impairment is a consideration.
Neurogenic pruritus
- Neurogenic
pruritus occurs in 80-100% of burns
- Pharmacological strategies used to
treat pruritus in burns include: antihistamines, amitriptyline, topical
treatments such as local anaesthetics, colloidal oatmeal, aloe vera and
moisturizer, ondansetron and gabapentinoids
Sleep disturbance, anxiety and depression
Trauma patients
are at high risk of sleep disturbance for multiple reasons:
- physiological stress response, psychological
distress and sleep disruption from care requirements
- Consider non-pharmacological
and pharmacological measures to regulate the sleep-wake cycle (eg. good sleep
hygiene, light therapy, benzodiazepine [short term use] and melatonin
0.1mg/kg nocte, where available)
- Anxiety and
depression is common following major trauma and affects the experience of pain
- Antidepressant drugs can be prescribed and are used for their psychotropic
as well as antineuropathic effects
References
- Craig KD et al: Developmental changes in infant pain expressions during immunization injections. Soc Sci Med 1984, 19(2): 1331-1337;
- Katz E, Kellerman J, Siegal S: Behavioural distress in children with cancer undergoing medical procedures: developmental considerations. J Consult Clin Psychol 1980, 48(3): 356365.
- WHO Guidelines
on the Pharmacological Treatment of Persisting Pain in Children with Medical Illnesses. Geneva: World Health Organization;
2012. Available
from: https://www.ncbi.nlm.nih.gov/books/NBK138354
- Pain, Pain Go Away: Helping Children with Pain. McGrath, Finley, Ritchie & Dowden, 2nded., 2003.
Further reading
Websites
- www.rch.org.au/anaes/pain_management/Childrens_Pain_Management_Service_CPMS -
Children’s Pain Management Service, RCH, Melbourne.
- pediatric-pain.ca/ -
The Center for Pediatric Pain Research
- www.iasp-pain.org/ - International Association for the Study of
Pain
Books/Journal Articles
-
McGrath PJ, Stevens BJ, Walker SM and
Zempsky WT. Oxford Textbook of Paediatric
Pain. Oxford
University Press, First edition, 2013.
Contains chapter 18 which is
dedicated to pain management in paediatric trauma and burns with
review of the literature and details on pharmaceutical management.
- Twycross A, Dowden and Stinson J. Managing Pain in Children: A Clinical Guide for Nurses
and healthcare Professionals. John Wiley &
Sons Ltd., Second edition, 2014.
User-friendly manual with
practical approach to paediatric pain; includes chapters on
pain assessment, acute and procedural pain management.
- Schug SA, Palmer GM, Scott DA,
Halliwell R and Trinca J. Acute Pain Management: Scientific Evidence. Australian and New Zealand
College of Anaesthetists and Faculty of Pain Medicine, Fourth edition,
2015.
Comprehensive and up-to-date
review of body of evidence in acute pain management,
entire section (Chapter 9) dedicated to the paediatric patient including
assessment tools, analgesics, blocks and non-pharmacological interventions.
- WHO Guidelines on the Pharmacological
Treatment of Persisting Pain in Children with Medical Illnesses. Geneva: World Health Organization; 2012. Available
from: www.ncbi.nlm.nih.gov/books/NBK138354 International
guidelines on pain management in children, good overview and easy
read.
- Roback MG, Carlson DW, Babl FE, et al. Update on pharmacological management of procedural
sedation for children. Curr Opin Anaesthesiol 2016;29 Suppl
1:S21-35.
Recent review of various
procedural sedation agents and regimens to use in the acute
setting.