See also
ANZCOR Guidelines: Paediatric Advanced Life Support
APLS: Advanced Paediatric Life Support Algorithm
Resuscitation: care of the seriously unwell child
Recognition of the seriously unwell neonate and young infant
These guidelines are point of care guidelines that aligns with ANZCOR and APLS guidelines.
APLS Paediatric Advanced Life Support Algorithm
Key points
- Cardiopulmonary resuscitation (CPR) should be commenced in an infant or child who is unresponsive and not breathing normally, pulse check should not delay commencement of CPR
- Optimal resuscitation relies on good team coordination, communication, and early allocation of roles
- Ongoing management should be directed by the cardiac rhythm identified
- Early consideration of ECPR/ECMO: contact appropriate services as per local procedures
Background
- Most arrests in children are due to hypoxia or hypotension
- Most common initial arrest rhythms in children are non-shockable: severe bradycardia, asystole, and pulseless electrical activity (PEA)
- Shockable rhythms: ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT), are approximately 15% of initial arrest rhythms
- Cardiac arrest following major trauma (traumatic cardiac arrest) is a unique situation which is outside the scope of this guideline ANZCOR Traumatic Cardiac Arrest
Assessment and management
- Assess environment for danger, ensuring staff and observer safety
- Assess for signs of life or response
- Send for help early: activate hospital emergency response team and consider early contact with local paediatric retrieval service
- Resuscitation includes assessment and prompt management in parallel
Early allocation of roles can optimise resuscitation (if personnel available):
- team leader
- airway nurse and doctor
- circulation nurse and doctor
- cardiac compression personnel
- defibrillator operator
- scribe + timekeeper with stopwatch
- staff member dedicated to family support
Assess for signs of life or response; if absent commence CPR
A - Airway
Optimise head position - infant: neutral position, child: sniffing position
Open the airway - head-tilt, chin-lift or jaw thrust
Suction secretions/blood/vomit under direct vision
Consider oro/nasopharyngeal airway for upper airway obstruction
B - Breathing
Look, listen and feel
If the child is not breathing, provide two initial breaths via bag valve mask (BVM) using 100% oxygen, and continue BVM ventilation as needed
Use 2-person technique as standard (if enough personnel)
Intubate if necessary (should be performed by proficient personnel and should not delay other resuscitation efforts, see Emergency airway management)
If intubated, continuous wave-form end-tidal CO2 monitoring should be used to:
- ensure adequacy of ventilation
- identify non-tracheal intubation
- warn of accidental extubation during CPR
- monitor for return of spontaneous circulation
C - Circulation
Check for signs of circulation - normal breathing, movement, coughing
If absent, start chest compressions
- Checking for a central pulse (brachial, femoral, carotid) is difficult and unreliable as a sole marker for commencing compressions
- Do not delay compressions if a central pulse cannot be palpated in less than 10 seconds
- If no pulse, slow pulse (<60 in an infant) or unsure, continue CPR and start chest compressions
Apply defibrillation pads and determine the cardiac rhythm as soon as possible: shockable or non-shockable (see Advanced Life Support flow chart below)
Gain IV access: intraosseous access is recommended if peripheral or central IV access is not already in place
Algorithm
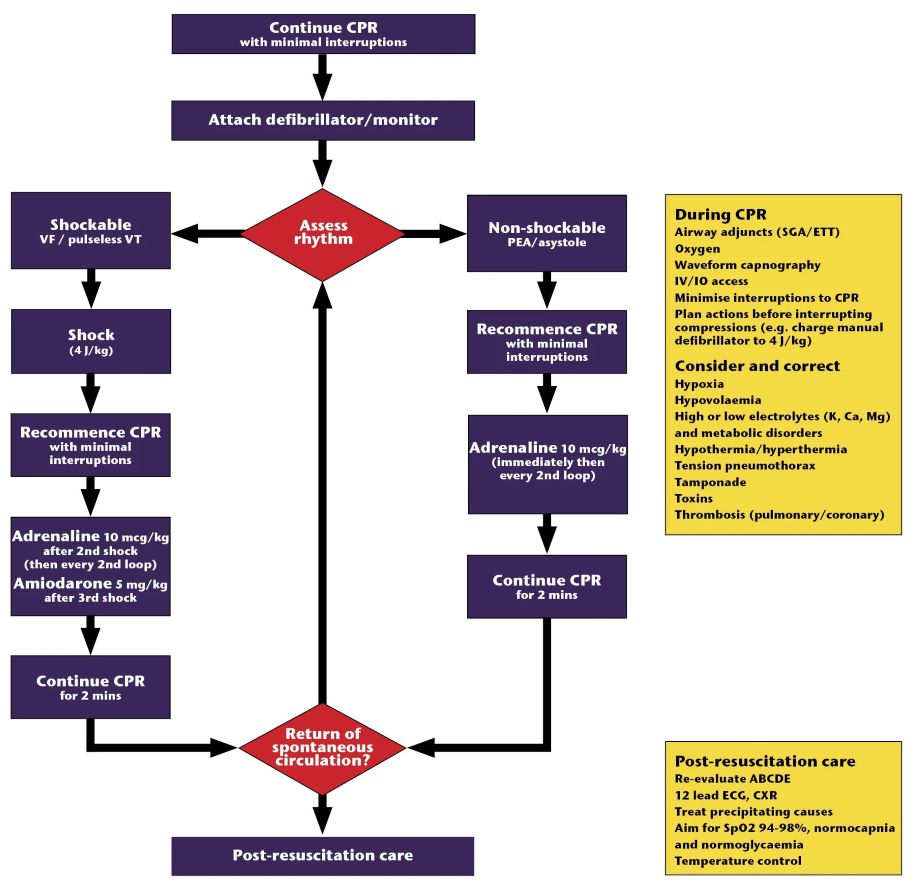
Advanced Paediatric Life Support: The Practical Approach 7th Edition, published 2024
Techniques
All images below courtesy of Children's Health Queensland, licensed under CC BY-NC
Airway opening manoeuvres

Head tilt and chin lift in an infant: neutral position
| 
Head tilt and chin lift in a child: sniffing position
|

Jaw thrust in an infant: neutral position | 
Jaw thrust in a child: sniffing position |
Chest compressions
- Rate for all ages 100-120 bpm
- CPR ratio 15 compressions:2 breaths
- If the child is intubated, compressions continue at rate 100-120 and breaths at rate of 10
- Place child on a firm surface. If on a bed, place cardiac compression board under child
- Perform chest compressions to lower half of sternum, compress by 1/3 of the AP diameter of the chest
- Infants:
- The recommended technique is a two-handed hold in which both thumbs compress the sternum
- The two-finger technique may be preferred by a single rescuer to minimise transition time between breaths and compressions.
- Children:
- Chest compressions can be performed using the heel of one hand
- Two-handed technique can also be used

Two-handed technique in an infant
| 
Two-finger technique in an infant
|

One-handed technique in a child |  Two-handed technique in a child |
DO NOT interrupt CPR except for rhythm check or defibrillation
Frequent changes of cardiac compression personnel (every 2 minutes) is desirable to avoid inadequate compressions due to fatigue
Defibrillator operator instructions
Minimise interruptions to CPR by charging whist chest compressions continue
DC shocks for VF and pulseless VT should be delivered asynchronously at a dose of 4 J/kg (round up)
Manual defibrillators are preferred in infants and children. Standard AEDs can be used for children >8 years. For children <8 years, the order of preference is:
- Manual defibrillator
- AED with paediatric attenuation
- Standard AED
Take care to ensure no one is touching the child at the time of delivering shock
For rhythm checks, consider the "COACHED" mnemonic:
- Compressions continue
- Oxygen away
- All else clear
- Charging
- Hands off (compressor stands clear and responds "I'm safe")
- Evaluating rhythm
- Defibrillate or Disarm
If DC shock delivered, recommence CPR immediately for 2 minutes prior to rhythm check
During resuscitation
Address reversible causes: 4 Hs and 4 Ts
- Hypoxaemia
- Hypovolaemia
- Hypo/hyperthermia
- Hypo/hyperkalaemia
- Tension pneumothorax
- Tamponade
- Toxins
- Thrombosis
Medications and fluids
Emergency drug dose calculator
Monash Children's Hospital Paediatric Emergency Medication Book
NETS Clinical Calculator
Primary resuscitation drugs are:
- Adrenaline (1:10,000) 10 microg/kg = 0.1 mL/kg IV/IM/intraosseous (max 1 mg)
- Amiodarone 5 mg/kg IV/intraosseous (max 300 mg) -- deliver as a rapid bolus with 5% glucose
Correct hypovolaemia:
- IV/IO crystalloid bolus of 10-20 mL/kg
- Additional bolus should be titrated to response
Correct hypoglycaemia:
- Aim for normoglycaemia
- IV/IO 10% glucose 2 mL/kg
Atropine, lidocaine, sodium bicarbonate and calcium are not routinely used and should only be considered in specific situations
Special circumstances
Specific conditions require a specific approach to cardiopulmonary resuscitation, such as
- Trauma (ANZCOR Traumatic cardiac arrest)
- Cardiac surgery
- Drowning
- Sepsis
- Pulmonary hypertension
- Toxins (National Poisons Centre 13 11 26)
Extracorporeal cardiopulmonary resuscitation (ECPR)
ECPR is a procedure offered by specialised paediatric intensive care centres in Australia
This should be considered early, within a short period of cardiopulmonary arrest and urgently discussed with appropriate local retrieval or onsite services, see Retrieval services
Cessation of CPR
The decision to cease CPR in children is difficult and must involve experienced senior clinicians, consider the clinical context, and occur in discussion with the child's family
Post resuscitation care - following return of spontaneous circulation
Children resuscitated from a cardiorespiratory arrest should be admitted to PICU
Ongoing reevaluation of ABCD
Perform 12 lead ECG and monitor for arrhythmias
Clinical targets of post-resuscitation care:
| Oxygenation |
Titrate inspired oxygen to achieve normal saturations: 94-98% or PaO2 60-80 mmHg) |
| Ventilation |
Aim for normal CO2 levels: PaCO2 35-45 mmHg |
| Perfusion |
Maintain systolic blood pressure >10th percentile for age and 50th percentile height with use of inotropes as needed |
| Temperature |
Maintain central temperature ≤37.C (avoid hyperthermia) |
| Glucose |
Maintain normoglycemia: 4-8 mmol/L |
Family Support
Family members of children undergoing CPR should be offered to be present, ideally with an assigned support person. Most hospitals have a family presence policy and staff education strategy in place
Staff Support
Regardless of the outcome, resuscitation is stressful and can be psychologically traumatic for team members providing care. Debriefing and support should be offered to all involved staff who wish to attend both immediately post resuscitation and ongoing as required.
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval services
Reference List
- Advanced Paediatric Life Support, Australia and New Zealand: The Practical Approach. 7th Edition Online Manual. https://www.apls.org.au/manual (viewed 31 March 2025)
- Australian and New Zealand Committee on Resuscitation (ANZCOR) Guidelines. Paediatric Advanced Life Support. https://www.anzcor.org/home/paediatric-advanced-life-support/ (viewed 31 March 2025)
- Craig, S. Paediatric Emergency Medication Book. 3rd Edition. 2023. Monash Children's Hospital. https://monashchildrenshospital.org/for-health-professionals/resources/resuscitation (viewed 31 March 2025)
- Greif, R et al. International Liaison Committee on Resuscitation (ILCOR) Summary Statement. 2024 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Circulation. 2024;150(24):e580-e687.
Last updated December 2025