See also
Acute poisoning
Head injury
Metabolic disorders
Stroke
Key points
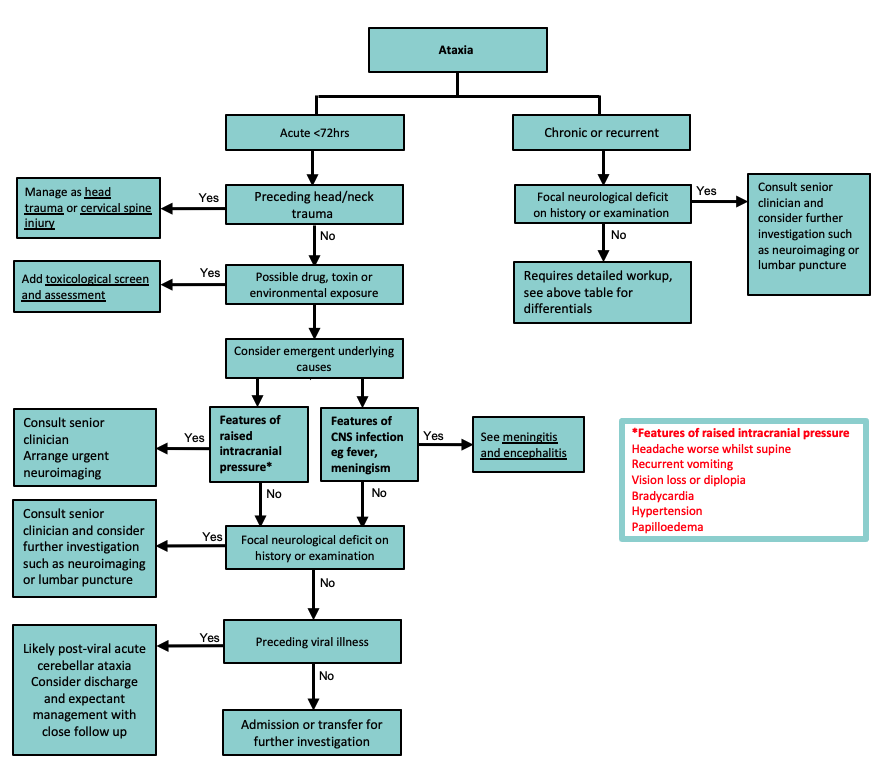
- Assessment focuses on a thorough evaluation for serious and treatable causes including CNS infection or inflammation, trauma, stroke, toxin ingestion and mass lesions
- Post-infectious acute cerebellar ataxia is the most common cause, it is self-limiting and is a diagnosis of exclusion
- Some conditions present with an unsteady gait due to weakness or pain. A frightened or very unwell child may also appear ataxic
Background
Ataxia is defined as unsteadiness, imbalance or clumsiness due to uncoordinated muscle movements, and presents as abnormal gait, speech or motor skills
Classification & causes
| Acute (<72 hours duration, previously well child) |
Chronic |
Recurrent |
Post-infectious*
Toxins*
Tumours*
Trauma*
Metabolic
Infections
Vascular, may require urgent lysis see Stroke
Immune (eg ADEM, Guillain Barre Syndrome)
Functional neurological disorder |
Brain tumours
Hydrocephalus
Metabolic
Nutritional
Congenital malformations
Hereditary ataxia
Trauma
Functional neurological disorder |
Episodic ataxia
Basilar artery migraine
Seizure disorder
Metabolic
Demyelinating pathology
Functional neurological disorder |
*Most common causes
Common causes of acute ataxia
|
Cause |
Timing |
Clinical features |
Post- infectious acute cerebellar ataxia |
Viral (eg varicella, EBV, HHV6,
Enteroviruses)
Mycoplasma |
Most commonly occurs 5-10 days after a prodromal illness |
Commonly affects children 2-7 years of age
Features of cerebellar ataxia which are maximal at onset and usually improve within 48-72 hours.
Full recovery usually occurs within 10-21 days (>90% resolve by 2 months) |
Toxins |
Antihistamines
Antiepileptics
Ethanol, ethylene glycol or isopropyl
Sedative-hypnotics |
Variable and dose related |
History of potential access to medications, environmental exposure or a recent change to medications
Altered GCS or toxidrome |
Tumours |
Oedema
Obstructive hydrocephalus
Haemorrhage |
Acute or acute on chronic |
Usually present with normal conscious level
Features of raised ICP
Constitutional symptoms
Focal neurological deficits |
Trauma |
Haemorrhage
Contusion
Diffuse axonal injury
Concussion |
Both acute and chronic |
History or clinical findings of head injury
Risk factors for NAI
|
ADEM |
Autoimmune condition leading to demyelination of the CNS |
Typically occurs 1-4 weeks after a febrile illness |
Lethargy or irritability associated with multiple neurological deficits including pyramidal signs, optic neuritis, hemiplegia, ataxia |
Assessment
History
- Time course (acute <72 hours)
- Antecedents include
- recent viral illness
- rash
- head trauma
- earache
- Symptoms of ataxia
- clumsiness, falls, broad based or staggering gait
- difficulty sitting upright
- slurred speech
- swallowing difficulties
- Other neurological symptoms, including:
- behavioural change
- photophobia
- vertigo
- Family history, including:
- metabolic disease
- hereditary ataxia
- migraine
- seizure disorder
- Drugs/toxins or environmental exposures
Examination
- Conscious state, orientation
- Thorough neurological examination is essential
- Exclude signs of meningoencephalitis (fever, meningism)
- Features suggestive ofcerebellar ataxia
- Cerebellar signs (dysdiadochokinesis, dysmetria, dysarthria, tremor, nystagmus)
- Gait abnormalities (staggering and/or wide-based)
- Features suggestive of sensory ataxia
- Positive Romberg test
- Loss of light touch, vibration and proprioception
- Hyporeflexia
- Features suggestive of vestibular ataxia
- Nystagmus without other cerebellar signs
Red flag features
- Signs of raised intracranial pressure
- Altered conscious state
- Focal neurology
- Meningism
- Loss of proprioception, vibration sense or tactile discrimination
- Weakness
- Abnormal deep tendon reflexes
Management
Investigations
If features are consistent with post-infectious acute cerebellar ataxia, then no investigations may be necessary
If ataxia does not resolve within 72 hours, worsens any time after onset or another cause is suspected, consider:
Bloods |
Imaging |
Other |
Blood glucose
Venous Blood gas
Electrolytes
Liver function tests
Anticonvulsant level, ethanol
|
Neuroimaging (CT or MRI depending on likely cause and availability) |
Toxicology
Metabolic screening
Viral studies
Vitamin B12 levels
Lumbar puncture (after neuroimaging)
EEG |
Treatment
Treatment will depend on cause, children with a presentation consistent with post-infectious acute cerebellar ataxia generally require no treatment
Consider consultation with local paediatric team when
- A child with an acute ataxia of unclear aetiology
- A child with chronic or recurrent ataxia
Consider transfer when
- Other focal neurological signs
- Raised ICP present
- History not typical of post-infectious acute cerebellar ataxia or aetiology is unclear
- Child requiring care beyond the comfort level of the hospital
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
The cause of ataxia is clear, the child is clinically well and there is a follow up arranged
Last updated August 2024