Introduction
Transpyloric tubes (also known as Nasojejunal Tubes or NJT) are used to provide nutritional support to patients who are not able to tolerate oral or gastric feeding. Insertion of a transpyloric tube involves placing a feeding tube through the nose (or
mouth), past the pylorus (opening between the stomach and small intestine) into the small intestine, where the tip of the tube is either positioned in the duodenum or jejunum.
Aim
This guideline supports nurses with appropriate training and experience to insert bedside transpyloric feeding tubes and is intended to be used in conjunction with clinical judgement and based on the needs of individual patients.
Definition of Terms
- Bedside Insertion (Bedside) – tube placement performed at the bedside without real-time imaging guidance such as fluoroscopy or endoscopy and is confirmed by abdominal x-ray
- Fluoroscopy guided Insertion – tube placement with the aid of real time imaging guidance
- Nasojejunal Tube (NJT) – thin, soft tube passed through child’s nose, down the back of throat, through the oesophagus, through the stomach and past the pylorus
- Nasogastric Tube (NGT) – thin, soft tube passed through the children’s nose or mouth, down the back of throat, through the oesophagus and through to the stomach
- Transpyloric Placement – placement of a feeding tube beyond the pylorus, including the duodenum and jejunum.
Assessment
Decisions regarding the method of transpyloric tube placement in paediatric patients should be made in collaboration with the multidisciplinary team and in partnership with the family.
Risk Assessment for Insertion
For some paediatric patients, transpyloric tube placement may not be appropriately completed without imaging (see below). In these situations, a referral to Medical Imaging for tube placement should be considered and discussed with the treating team.
Contraindications for Transpyloric Tube Insertion
Absolute Contraindications
Bedside Transpyloric tube insertion is contraindicated in certain patients; alternative options must be considered for the following:
- Bowel Obstruction
- Ileus
- Perforation or significant GI Bleeding
- Necrotising Enterocolitis
- Ischaemic Bowel
- Post-Operative Bowel Resection or gastric surgery
- Inability to gain safe enteral access including significant mid face trauma, nasal fractures, basal skull fracture
Relative Contraindications
In the presence of relative contraindications, the advantages and disadvantages of tube placement, including method of placement (bedside or medical imagining) will need to be considered and discussed with the treating team and senior nursing staff in
clinical area.
- A history of gastric surgery or gastric perforation
- History of gastrointestinal bleeding, intestinal obstruction, ischemic bowel disease and epistaxis
- Gastroduodenal ulcers and oesophageal varices
- Severe sinusitis
- Oesophageal trauma, strictures, obstruction or history of oesophageal surgery
- Recent nasal surgery
- Implantable cardiac defibrillator, implantable cardiac or diaphragm pacemaker
- Low platelet count
Transpyloric Tube Insertion
The treating team is responsible for placing an EMR order for insertion of the Nasojejunal Tube including imaging required to confirm tube placement.
Selecting the correct tube and size
At RCH, the recommended tube to be inserted for jejunal feeding is the yellow CORFLO silastic enteral feeding tube with ENfit® connector.
The smallest size possible should be used to accommodate feed consistency and patient comfort. In general, a
tube size of between 8 to 10French (Fr) should be used. Larger sizes (over 10Fr) may be used on children over 12 years based on clinical judgement. Generally, 6Fr are not recommended as they block easily. There is no official guidance for Trans-pyloric
Tube sizing, however Table 1 can be used as a practical guide for tube selection.
Table 1. Tube size selection
|
Patient Weight
|
Tube size
|
Tube Length
|
|
< 10 kg
|
6Fr - 8Fr
|
91 - 109cm
|
|
≥ 10 kg up to
< 30 kg
|
8Fr - 10Fr
|
|
> 30 kg
|
10Fr - 12Fr
|
109 - 140cm
|
Choose a length that will allow approximately an extra 20cm external to nostril.
Preparation of patient
- Provide the patient and family with an age-appropriate explanation of the procedure and the rationale for tube insertion or removal. Consider and plan for age-appropriate procedural positioning and non-pharmacological distraction techniques.
- For further information refer to the RCH Nursing Guideline: Procedural Management.
- If a NGT is already in place, aspirate gastric contents before attempting insertion. Removal of the NGT is not required prior to trans-pyloric tube insertion.
Equipment
- Suction and oxygen should be available
- Appropriate size and type of tube (Pre-freezing tubes before insertion can improve rigidity making them easier to guide).
- Lubrication - water or use of patient’s own saliva (neonates)
- x2 10mL Enteral Syringe
- pH Test indicators
- Stethoscope
- x2 Vial sterile water for injection
- Pen marker
- Securement tapes (Comfeel®, Tegaderm™, Scissors, Cavilon Barrier Wipe™)
- Gloves, eye protection if vomiting expected
Procedure
- Assessment of Nasal Passage
Assess the nostrils and oral cavity for any possible abnormalities or obstruction prior to insertion of the tube. If reinserting a tube, consider alternating nostrils if possible.
- Determine the length of the tube insertion
Measure and mark the tube at the following measurements:
(a) Tip of the Nose to Tragus
(b) Tragus to the xiphisternum
(c) Xiphisternum to Right lateral costal margin (the
lower edge of the right side of the ribs). This aligns the tube for entry into the pylorus.
(d) Plus, an additional 10cm
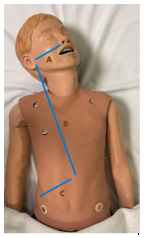
Image taken by RCH staff member.
Administering a promotility agent, such as Metoclopramide 5-10 minutes prior to insertion, will enhance the likelihood of successful trans-pyloric tube advancement.
Refer to AMH paediatric dose recommendations under Metoclopramide “Aid in Intestinal Intubation”.
- Insertion of Tube into Stomach
(a) Position patient in a supported manner that prevents hyperextension of the neck.
(b) Lubricate the tube, water is recommended, or in neonates use their own saliva.
(c) Insert the tube
into patient nostril, gently aiming posterior and parallel to the nasal septum, then aiming downward. If practical, ask the child to swallow or wait for a swallow to occur. This will assist the passage of the tube into the stomach. Consider the
use of a pacifier for neonates. Insert the tube to the pre-measured length of xiphisternum.
(d) During insertion of the tube monitor for respiratory distress, excessive coughing or choking. If this occurs, stop advancement, remove and adjust
direction slightly before reattempting.
(e) Obtain a gastric aspirate pH 1- 5.0, to confirm correct position (in the stomach).
- Advancement towards Jejunum
(a) Position patient in the right lateral decubitus position (lying on right side) to assist advancement of tube into the jejunum.
Patient remains in Right Lateral Decubitus position until TPT is
confirmed on Abdominal X-ray.
(b) Simultaneously insert 1-2 mL of air and advance the tube in increments of 1-2cm until pyloric mark (right lower costal margin measurement) is reached at the nostril.
(c) Listen on inserting air and notice
the change in sound from low pitch gurgles to high pitch as it enters the duodenum. A subtle ‘give’ may be felt as it crosses the pylorus.
(d) Listen for air in the upper right quadrant.
(e) Advance the tube further by passing the extra
measured 10cm.
(f) When 10 mL of sterile water is inserted and less than 2 mL returns on aspiration, it is in the small bowel.
a. If the aspiration is 2mL or less, confirm transpyloric placement with an abdominal X-ray (Note: ongoing
aspiration of the tube is not recommended).
b. If aspirated volume exceeds 2mL, the tube is likely in the stomach, maintain the patient in the right lateral decubitus position until tube placement is confirmed.
If resistance is felt
during insertion, stop advancement and adjust direction slightly before reattempting.
If placement is unsuccessful after 2 attempts, discussion with Medical Imaging is required for fluoroscopy guided placement.
- Securing tube for use
a. Confirm centimeter marking on the tube at the nostril.
b. Remove the stylet by flushing the tube via the side port with water (Do not reinsert stylet when tube is in the patient).
c. Secure the
tube with Comfeel™ secured to the cheek, followed by Tegaderm™ positioned over the tube. Ensure the tube is secure to minimise the risk of pressure injury in and around the nostrils
- Confirm placement prior to administering medication or feeds into tube
Obtain Abdominal X-ray within 60–90 minutes to confirm transpyloric tube position.
Please note: tube position must be confirmed with the treating medical team prior to commencement of feeds or medication administration via transpyloric tube/NJT.
For information regarding feeding and management of Transpyloric/NJ Tubes refer to the RCH Nursing Guideline: Jejunal Feeding.
Post procedure
Continue to monitor for signs of respiratory distress including persistent coughing or gagging. Any patient who is clinically unstable following transpyloric tube insertion requires an urgent medical review to exclude bowel perforation.
Changing a Transpyloric feeding tube/NJT
Frequency of tube change will vary depending on the manufacturer’s guideline.
Removal of Transpyloric feeding tube/NJT
Equipment
- Suction and Oxygen should be available
- PPE (non-sterile gloves and eye wear)
- Adhesive remover
Transpyloric Tube Removal Procedure
(a) Perform Hand Hygiene
(b) Turn off continuous feeding, if applicable
(c) Ensure that the patient and family is aware of and understand the reasons for removal.
(d) Position the patient in a supine position. Elevate the head of the bed for
comfort. Prepare the child as per RCH Nursing Guideline: Procedural Management.
(e)
Gentle use of adhesive remover to remove securement tapes from the face.
(f) Occlude the tube by pinching it closed.
(g) Pull the tube out using a swift, consistent motion with the thumb and index finger.
(h) Clean face and nose, support
patient to recover.
Troubleshooting
|
Troubleshooting Potential Problem (related to insertion)
|
Risk factor /Common cause
|
Presentation
|
Considerations
|
|
Unable to obtain gastric aspirate/aspirate pH >5 during insertion
|
Uncommon, Minor Influenced by:
- Acid suppression medications
- Tube not positioned adequately
|
|
|
|
Unsuccessful placement
|
Uncommon, Minor
Influenced by:
- Underlying anatomy
- Insertion technique
- Proceduralist
|
- Respiratory distress
- May be no signs
- Circling in the stomach on X-ray
|
-
Consider alternative insertion technique and / or proceduralist
- Freezing the tube for 30 minutes before insertion may facilitate placement
|
|
Clinically unstable following transpyloric tube insertion
|
Uncommon: Major
Influenced by:
- Age
- Anatomy
- Medical comorbidities
|
- Abdominal distention
- Vomiting
|
|
Complications
|
Complication (related to insertion)
|
Signs and symptoms
|
Risk factors
|
Management
|
|
Bowel perforation
|
- Acutely unwell/changes in observations
- Sudden, severe abdominal pain which may continue to increase.
- Nausea and vomiting
|
This is considered an uncommon but significant complication. Patients who are most at risk include:
-
Infants and Children less than 2 years of age or less than 10kgs
-
Medical co-morbidities
-
Significant neurological impairment or an inability to communicate pain
|
|
|
Dislodgement, Tube migration
|
- Vomiting
- Feed Intolerance
- Aspiration Pneumonia
|
- Common, Minor
- Influenced by:
- Age
- Unsecured securement tapes
|
- Stop continuous feeds
- Remove tube
- Medical review
|
Companion Documents
RCH Clinical Practice Guidelines
RCH Nursing Clinical Guidelines
RCH Policies and Procedures
Please remember to read the disclaimer.
The development of this nursing guideline was coordinated by Ash Doherty, CNC, Emergency Department, and approved by the Nursing Guideline Committee. First published September 2025.
Evidence Table
| Reference |
Source of Evidence
|
Key
findings and considerations |
| Joffe, A; Grant, M; Wong, B; Gresiuk, C. (2000) Validation of a blind transpyloric feeding tube placement technique in paediatric intensive care: Rapid, simple, and highly successful. Paediatric Critical Care Medicine 1(2)151-155 |
Observational
|
High Success rate of transpyloric feeding tube placement when using combination of metoclopramide administration, right lateral positioning and incremental air insufflation.
|
| Ketsuwan, S., Tanpowpong, P., Ruangwattanapaisarn, N., Phaopant, S., Suppalarkbunlue, N., Kooanantkul, C., Anantasit, N., & Vaewpanich, J. (2021). Intravenous metoclopramide to improve the success rate of blind bedside post-pyloric placement of feeding tube in critically ill children: A randomized, double-blind, placebo-controlled study. Frontiers in Pediatrics, V9, Article 739247 |
RCT
|
Metoclopramide improves success rate of trans pyloric feeding tubes.
|
McGrath KH, Collins T, Comerford A, McCallum Z, Comito M, Herbison K, Cochrane OR, Burgess DM, Kane S, Coster K, Cooper M, Jesson K. (2024).A clinical consensus paper on jejunal tube feeding in children. JPEN. Apr;48(3):337-344. doi: 10.1002/jpen.2615.
|
Clinical consensus paper
|
Consensus statements developed by expert working group of the Australasian Society of Parenteral and Enteral Nutrition (ASPEN) including patient selection, type and selection of feeding tube and complications.
|
| Quinteiro, N, Fioravanti Dos Santos, J, de Siqueira Caldas, J &
Carmona, E. (2024). Procedures for a Transpyloric Feeding Tube Inserted Into
Newborns and Infants: A Systematic Review. Advances in Neonatal Care, 24,
374-381. |
Systematic Review
|
Bedside insertion of transpyloric tubes is successful with glabella-calcaneal measurements, gastric air insufflation and right lateral decubitus position.
|
| Tiancha H, Jiyong J, Min Y. How to Promote Bedside Placement of the Postpyloric Feeding Tube: A Network Meta-Analysis of Randomized Controlled Trials. JPEN J Parenter Enteral Nutr. 2015 Jul;39(5):521-30. |
Meta-Analysis |
Air Insufflation promotes bedside placement of transplyoric feeding tubes in adults. Prokinetic agents not required in paediatric patients without impaired motility.
|
| Phipps LM, Weber MD, Ginder BR, Hulse MA, Thomas NJ. (2005).A randomized controlled trial comparing three different techniques of nasojejunal feeding tube placement in critically ill children. JPEN 29(6):420-4. |
RCT |
No significant difference in success rates among three methods of blind bedside insertion (standard, standard with air insufflation, standard with IV Erythromycin).
|
| Spalding HK, Sullivan KJ, Soremi O, Gonzalez F, Goodwin SR. (2000). Bedside
placement of transpyloric feeding tubes in the pediatric intensive care unit
using gastric insufflation. Crit Care Med. 28(6):2041-4. |
Prospective, RCT |
Gastric insufflation (10ml/kg) air significantly improved first-attempt success and reduced time to enteral feeding in critically ill children undergoing bedside transpyloric tube insertion.
|
Starship Child Health Nursing
Guidelines
Nasogastric
& nasojejunal tube care for an infant, child, or young person (June 2023)
|
Guideline |
Describes specific technique for insertion of NJ tube
Child remains positioned right side down for 60 to 90 minutes post insertion
|
| Sydney Children’s Hospitals Network: 2024 *Enteral Feeding Tubes and the Administration of Enteral Nutrition |
Guideline |
Guideline for Enteral Feeding Tubes and the Administration of Enteral Nutrition. Appendix 3 Placement of transpyloric tube.
|
Turner AD,
Hamilton SM, Callif C, et al. (2020) Bedside Postpyloric Tube Placement and
Enteral Nutrition Delivery in the Pediatric Intensive Care Unit. Nutrition in
Clinical Practice : Official Publication of the American Society for Parenteral
and Enteral Nutrition. Apr;35(2):299-305. DOI: 10.1002/ncp.10452. PMID: 31990093.
|
Single centre
retrospective study |
Retrospective chart review of nurse led bedside (gastric
insufflation) postpyloric feeding tube placements in 100 PICU patients.
Bedside placement used for 93 patients (success rate 84.9%).
Successful confirmation by Xray showed most common location
for the tip was the proximal duodenum (37%) followed by distal duodenum (33%)
duodenal jejunal junction (24%) and jejunum (6%).
RN Competency training program in place.
|