1. Summary
Pelvic avulsion injuries are usually seen in the active adolescent patient. Whilst they are technically a fracture of the pelvis, they differ from the other types in that they are not usually caused by a high degree of extrinsic force, instead being caused by a sudden muscle contraction such as may occur during a sporting activity.
The vast majority of these injuries have a good outcome with conservative management once diagnosed, though delay to diagnosis has some association with longer term issues. Only a small minority require consideration of surgical management.
The main challenge in managing the enthusiastic adolescent athlete lies in convincing them for the need for rest during the convalescent phase.
2. How are they classified?
- Main classification is by location
- Can also be classified by degree of displacement
- Pelvic avulsion fractures are pelvic fractures graded under the Zieg/Torode system as type I. (for other pelvic fractures, see pelvic fracture guideline
3. How common are they and how do they occur?
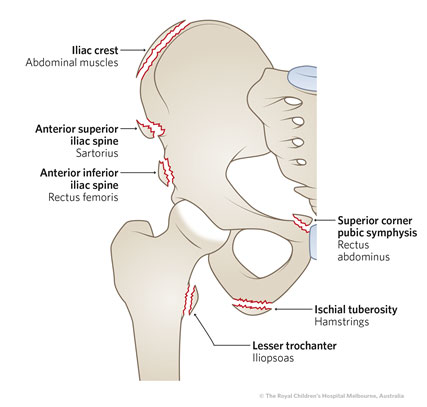
These fractures are relatively common in the adolescent athlete, due to the relative weakness of the apophysis compared with the tendon. They can occur when an explosive muscular contraction, such as sprinting, kicking or jumping causes the tendon to pull at the apophysis and cause a separation of the apophysis from the bone. Males are affected more often than females.
The most frequently affected sites are the Anterior Superior Iliac Spine, Anterior Inferior Iliac Spine, and Ischial Tuberosity.
4. What do they look like – clinically?
The adolescent patient will present with a history of a sudden pain during forceful muscle contraction, for example whilst kicking a ball, sprinting, or doing gymnastics. It may be associated with a ‘cracking’ sound or sensation. The acuity of this history helps make the diagnosis
On examination the patient will have local tenderness and pain at the site exacerbated by passive stretching (or active contraction) of the associated muscle groups,
Some patients may have a history of intermittent pain in the same area prior to the acute injury suggestive of an apophysitis - this is more common in the ischial avulsion. Apophysitis is covered in a separate guideli ne: in this condition, there is generally a history of pain with exercise and relieved by rest. X-rays can look abnormal with the area appearing fuzzy, suggesting a chronic issue rather than acute fracture, although the treatment is similar - a graded return to sport under supervision. |
5. What radiological investigations should be ordered?
An AP Pelvis X-ray should be obtained. In patients where ASIS or AIIS fracture is suspected, an oblique pelvis view is best.
MRI is NOT required where the diagnosis is clear on a simple AP pelvis X-ray. Very occasionally, this test may be useful to detect subtle apophyseal avulsion fractures and ongoing pain with apparent normal x-rays in skeletally immature patients.
6. What do they look like on x-ray?
 |
 |
| Ischial Tuberosity Fracture - Left |
Anterior superior iliac spine (ASIS) - Left |
 |
 |
| Avulsion of right anterior inferior iliac spine (AIIS): sudden onset pain during running in a 14yo boy. |
 |
|
| Avulsion of left iliac crest apophysis: sudden onset pain during sprinting in a 15 yo boy |
 |
|
| Left lesser trochanter avulsion |
|
7. When is reduction (non-operative and operative) required?
The vast majority of pelvic avulsion injuries will heal without surgical treatment, but the patient will need to follow a gradual recovery program overseen by a physiotherapist or Sports Medicine Physician as outlined below.
Pelvic apophyseal avulsion fractures that are displaced more 30mm are at a higher risk of non-union and warrant a consideration of operative fixation, however this is rarely performed.
8. Do I need to refer to orthopaedics now?
Orthopaedic consultation need not occur out of hours or emergently unless it is indicated for a coexisting injury. Where an orthopaedic opinion is required (see below), it can occur in an outpatient setting.
9. What is the usual ED management for this injury?
A period of non-weight bearing, rest, ice therapy and simple pain relief is recommended.
The injury should be explained to the adolescent and their family, along with the importance of initial rest without weight bearing, followed by protected weight bearing after a week. Return to sport will usually take about 8-10 weeks. Ice packs can be applied to the site of injury intermittently during the first few days. The patient should mobilise with crutches - see Kids Health Information - Fact Sheets - Crutches, with follow up as below.
10. What follow up is required?
The majority of cases are best handled by a Physiotherapist and/or a Sports Medicine Physician. Either of these professionals will oversee a program of progressive weight bearing, stretching, movement against resistance, muscle strengthening and return to full sport participation
Where there is significant displacement of the fragment beyond 3 cm, local orthopaedic outpatient consultation can be arranged, although surgery is rare..
11. What advice should I give parents?
The majority of these injuries heal completely without the need for surgical correction, but compliance with an initial period of rest and then protected weight bearing is key to preventing delays to full recovery, repeat injury or development of chronic symptoms.
12. What are the potential complications associated with this injury?
- Non-union, particularly where displacement is more than 3cm
- Ongoing pain with functional limitations
- Chronic pain
- Femoroacetabular impingement (AIIS only: inferior displacement &/or hypertrophy of the avulsed fragment can mechanically conflict with the femoral neck, leading to anterior groin pain with hip flexion and limitation of range of flexion).
13. References
Ghanem I & Rizkallah M, Paediatric Avulsion Fractures of the Pelvis: Current Concepts Curr Opin Pediatr 2018;30(1);78
Eberbach H et al, Operative Versus Conservative Treatment of Apophyseal Avulsion Fractures of the Pelvis in the Adolescents: A Systematical Review With Meta-Analysis of Clinical Outcome and Return to Sports, BMC Musculoskelet Disord 2017:18(1);162
Schuett DJ, Bomar JD, Pennock AT. Pelvic apophyseal avulsion fractures: a retrospective review of 228 cases. J Pediatr Orthop. 2015;35:617–23
Cheng CW, Young Athletes Beware BMJ Case Reports 2014;bcr2014204738. Reproduction of image with permission.
Gidwani BMJ 2004;329:99
Sutter, R and Pfirrman C. Atypical Hip Impingement, AJR 2013;201:W437-442
Last updated November 2020