1.
Summary
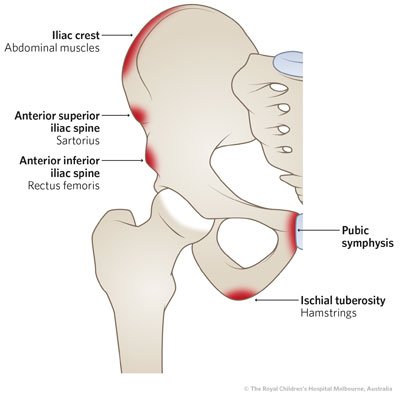
The apophysis is the location of a growth plate with a muscle attachment - there are several in the pelvis where the various thigh muscles attach.
Apophysitis involves inflammation of one of these with associated dull pain, and is typically associated with muscle overuse.
It is usually of gradual onset, and should be differentiated from Avulsion injuries of the Pelvis which present as an abrupt injury.
2. How are they classified
ASIS - Anterior Superior Iliac Spine
AIIS - Anterior Inferior Iliac Spine
Iliac crest
Ischial spine
Pubis
3. How common are they and how do they occur
Apophysitis is usually associated with strenuous muscle overuse such as might occur in athletes, running sports (e.g. soccer, AFL etc), gymnasts or dancers.
4. What do they look like - clinically?
They will usually present with gradual onset pain in the area of concern (e.g iliac crest, AIIS, Ischial spine etc) that worsen with activity. Pain worsens with activity and settles with rest. There is almost always local tenderness at the site of the apophysis.
In the case of ischial spine apophysitis, passive hamstrings stretching will elicit tenderness at the ischial spine. Direct palpation of the ischial spine is best done with the patient on their back with the affected leg bent at 90 degs at hip and knee and direct palpation of the ischial spine can be done easily.
5. What radiological investigations should be ordered?
An AP pelvis X-Ray can be ordered if there is a need to differentiate it either from an acute avulsion, or the possibility of a missed avulsion injury that has developed chronic non-union .
6. What do they look like on X-Ray?
X-ray may be normal or show a fluffy appearance to the muscle attachment area.
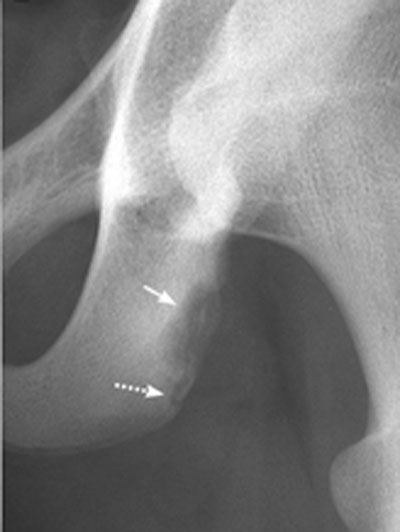
ischial apophysitis
7. When is operative treatment required?
Surgical treatment is of no benefit in apophysitis.
8. Do I need to refer to orthopaedics now?
Orthopaedic referral is not required where the diagnosis is clear. Follow up is usually with a physiotherapist and/or a sports physician, as discussed below.
9. What is the usual ED management for this condition?
- The main emphasis is on advising patients to have “relative rest” . This entails doing things that are not painful. If painful to walk then crutches may be needed, otherwise rest from any activity that causes pain for 1-2 weeks. Avoid stretches that cause pain at the tendon insertion site.
- Intermittent ice applied to the area initially may be of benefit.
- Non-steroidal anti-inflammatories may be of benefit for a short course (1 week).
- At the initial consult it is important to emphasise that return to sport will need to be gradual; overly ambitious return to full activity can lead to worsening injury and chronic pain. The longer the symptoms have been present, the longer it is likely to be before it improves.
10. What follow-up is required?
Follow up should be with a physiotherapist and/or a sports physician. These professionals will be able to provide a graded return to exercise program over several weeks, and advice regarding stretching exercises to minimise chance of re-injury.
11. What advice should I give to parents?
Early rest, avoid rushing back to sports and adherence to physiotherapy / exercise program should be the focus.
Premature return to sports will result in a longer period of recovery.
In the process of returning to activity, any pain should be interpreted as a sign to ‘back off’, not something to ‘push through’. Patience is required.
12. What are the potential complications associated with this injury?
Ongoing pain and limitation of activity.
Avulsion fractures from inappropriate early return to strenuous activities.
13. References
- Clancy, W and Foltz, A.Iliac apophysitis and stress fractures in adolescent runners, Am J Sports Med 1976;4(5):214-218
- Frush, T & Lindenfeld, T. Peri-epiphyseal and Overuse injuries in the Adolescent Athlete Sports Health 2009;1(3):201-211
- Pointinger, H. Avulsion fracture of the anterior superior iliac spine following apophysitis Br J Sports Med 2003;37:361-362
- Read, J. Sports Medicine Imaging, accessed 12 August 2020, http://sportsmedicineimaging.com/topics/pubic-apophysitis/ - Images reproduced with permission.
- Sailly, M et al. Pubic apophysitis: a previously undescribed clinical entity of groin pain in athletes British Journal of Sports Medicine 2015;49:828-834.
Last updated November 2020