See also
Sepsis – assessment and management
Acute meningococcal disease
Child abuse
Key points
- The majority of children with petechiae do not have a serious bacterial infection or meningococcal disease, and often will not have a specific cause identified
- Seriously unwell children with petechiae/purpura require urgent management
Background
- Serious bacterial infections including meningococcal disease can present with a non-blanching rash, with or without fever
- The incidence of pneumococcal and meningococcal bacteraemia has decreased since the introduction of routine vaccination
- There are many other infective and non-infective
causes of petechiae and purpura (see table below)
Definitions
- Both petechiae and purpura do not blanch when pressure is applied - this is in contrast to other common rashes in children such as viral exanthems and urticaria
- The 'glass test' can be used to assist with assessing whether a rash is blanching - a drinking glass can be applied firmly against a rash - if the rash does not disappear it is non-blanching

Image: glass test
- Petechiae are pinpoint non-blanching spots
- Purpura are larger non-blanching spots (>2 mm)

Image: petechiae on the torso and legs of a child

Image: purpura on the torso and back/face of a child
Assessment
All children with fever and petechiae/purpura should be reviewed promptly by a senior clinician
History
- Immunisation status - children
<6 months of age or with incomplete immunisation status
- Rapid onset and/or rapid progression of symptoms and rash
- Medications: prior treatment with antibiotics may mask signs of a bacterial infection
- High risk groups: immunosuppression, previous invasive bacterial infections
- History of trauma/injury
- Association with bleeding, abdominal pain, joint pain, difficulty mobilising
- Travel
- Sick contacts
Examination
Children are considered unwell when they have:
- Abnormal vital signs: tachycardia, tachypnoea and/or desaturation in air
- Cold shock: narrow pulse pressure, cold extremities, prolonged capillary refill
- Warm shock: wide pulse pressure, bounding pulses, flushed skin with rapid capillary refill
- Altered conscious state: irritability (inconsolable crying or screaming), lethargy (including as reported by family or other staff)
- Limb tenderness or difficulty mobilising
For more information on assessment of the unwell child see
Resuscitation: Care of the seriously unwell child
For all children, also consider haematological causes and review for:
- Hepatomegaly or splenomegaly
- Lymphadenopathy
- Swelling or erythema of joints
Differential diagnoses
Causes of petechiae and/or purpura
|
Viral |
Enterovirus
Adenovirus
Influenza |
|
Bacterial |
Neisseria
meningitidis
(meningococcal disease)
Streptococcus pneumoniae
Haemophilus influenzae
Group A streptococcus
Staphylococcus aureus |
|
Mechanical |
Vomiting or coughing - occurs in the distribution of the superior vena cava which is above the level of the nipples
Local physical pressure eg holding child during procedure, tight tourniquet
Non-accidental injury or accidental injury
|
|
Haematological |
Immune thrombocytopenia (ITP)
Malignancy including acute leukaemia
Aplastic anaemia
Disseminated intravascular coagulation (DIC)
Haemolytic uraemic syndrome (HUS) |
|
Other |
Henoch-Schönlein purpura (HSP)
Vasculitis
Drug-induced thrombocytopenia |
Note: There are additional causes of petechiae that should be considered in newborns (eg congenital cytomegalovirus, toxoplasmosis, neonatal lupus). Any newborn with petechiae should be promptly reviewed with a senior clinician
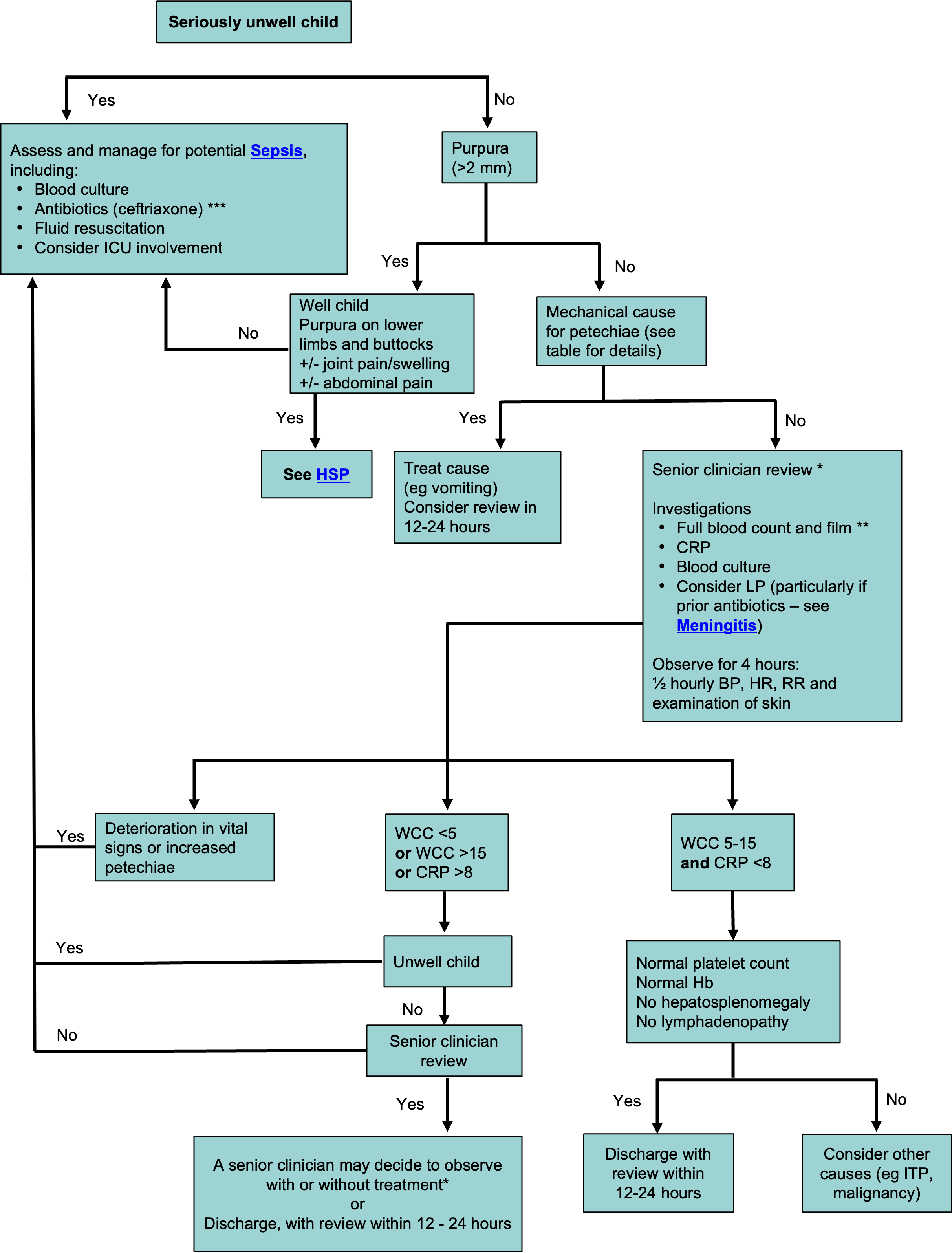
Management
Antimicrobial recommendations may vary according to local antimicrobial susceptibility patterns. Refer to local guidelines
* Senior clinician review may lead to decision making pathways outside of this flowchart, including the role of investigations. If a senior clinician is unavailable, the safest approach is to manage according to the flowchart.
** Film must be reviewed to exclude an alternative diagnosis
***
Antibiotics:
- Ceftriaxone:
100 mg/kg (4 g) IV daily (where possible, ceftriaxone should be avoided in neonates <41 weeks gestation, particularly if jaundiced or receiving calcium containing solutions, including TPN)
- Cefotaxime: 50 mg/kg (2 g) IV 12H (week 1 of life), 6-8H (week 2-4 of life), 6H (>week 4 of life)
Consider consultation with local paediatric team when
- Assessing any unwell child, including any with suspected meningococcal disease
- Uncertainty about diagnosis or to arrange follow-up
- Advice regarding escalation of care
Consider transfer when
Child requiring care beyond the comfort level of the hospital
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services.
Consider discharge when
- Serious cause of petechiae/purpura considered unlikely based on clinical assessment and/or investigations
- Always advise parents to return for review if their child becomes more unwell or there is concern
Parent information
Rashes
Fever in children
Last updated February 2021