There are many different burns unit's throughout the world. In providing this information we hope to educate you that even though there are differences the main outcomes are still the same. This should help to also give conformity in the specialised care needed. The consultants Russell Taylor, Tom Clarnette, Warwick Teague, Sian Fairbank and Jonathon Burge are the experienced surgeons in this field.
Kathy Bicknell is the Burns CNC. She provides clinical care, coordinates inpatient and outpatient care for burns patients and provides education to patients, families, nursing, medical and allied health. She is also involved in developing prevention strategies and providing education in the community.
Kellie Smith and Kate Glassford are the burns unit Care Managers. They co-ordinate the care of burns patients on Platypus ward who have a severe burn injury.
The Clinical Facilitator provides education and support to staff within the hospital.
The multidisciplinary team meet weekly on a Wednesday morning at 0930am to discuss the care of patients.
Thank you for taking the time to read this information.

Clinical information
There are five functions of the skin that make it so important.
These are:
- Protection
- Fluid balance
- Thermo-regulation
- Sensory organ
- Produces vitamins

Information required prior to admission
The following questions to ask/tell the Ambulance Officer/Admitting Officer/Burns unit staff are important in assisting the Medical and Nursing staff to ascertain the severity of the burn injury.
- Estimated time of arrival
- Name, Age of the child
- What type of burn and location on the body
- Estimated percentage (how have they made this estimate)
- ?Inhalation injury
- How it occurred and time it occurred
- first Aid
- What treatment was given, if any
- Is intravenous access established
- Has analgesia been given
- ?Tetanus status current
- Are the parents/guardians aware. Will they accompany the child
- Is an interpreter required
- Past medical history ie. asthma, diabetes, epilepsy

Classification of burns
Burns are classified into five categories:-
- Epidermal (Not included in TBSA%)
- Superficial Dermal
- Mid Dermal
- Deep Dermal
- Full thickness
Burns dressings
The method of dressings we use at The Royal Children's Hospital involves a "closed" dressing technique, with the exception of burns to the face and perineum. We use this method for a number of reasons. The main reasons are for protection and absorption and for decreasing stress of both the patient and the family, Dressing changes can but may not necessarily be 'painful' however the emotional and psychological distress can be enormous. Because of this the number of dressings required should be kept to as few as possible.
The moistness, size, depth, and area of the burn needs to be taken into consideration for dressing selection. The aim of the burn dressing is to keep the wound clean and dry, and prevent infection.

Epidermal burns - Involves the epidermal layer only and will heal usually within a few days
Superficial burns
A superficial burn involves only the epidermis and the upper part of the dermal papillae. The burn may appear bright pink or red in colour (erythema). Blisters may or may not be present. The texture is normal or firm and the area is very painful and hypersensitive to touch. On pressure the burn area will blanch and capillary return will be brisk. In time the erythema will fade and spontaneous healing will occur with no surgical intervention.
An occlusive non-stick dressing can be used for this sort of burn:
Generally dress with a non stick dressing like Mepite/Jelonet/Bactigras, Melolin and crepe bandage. Secure with Hyperfix if necessary.
Mepitel is a low adherent wound contact dressing made of silicone gel bound to a flexible polyamide net.
It is preferable to leave the dressing intact until the patient is reviewed after 7 days, or earlier if necessary. Spontaneous healing will occur. These sorts of dressings allow the child a certain amount of mobility within a given area, without concern of further injury to the wound or discomfort to the child. It allows for greater ease and comfort for both the patient and the care givers when nursing the child.
Protection is a two way process in the "closed" method. An closed dressing protects the wound, but also protects the "outside", be it patients, staff, family or anyone who comes into contact with the patient.

Partial thickness (Mid - Deep Dermal)
This type of burn injury results in the entire epidermal layer being destroyed along with varying thickness of the dermis. Hence a Partial Thickness injury can be either Superficial, mid or Deep.
The substructures - sweat glands and hair follicles generally remain undamaged, but some can be affected. It is characterised by a creamy coloured base which is mottled in appearance. Usually a Superficial Partial thickness burn will heal itself by regeneration of the epithelial layer but will take longer to heal than a superficial burn. A deep partial burn where the deeper substructures, sweat glands and hair follicles are affected, if left untreated will leave scar tissue.
Unfortunately the depth of a Partial thickness burn may take up to 7 - 10 days to declare it self as superficial or deep.
A closed dressing should be used:
Generally we use Acticoat or Acticoat 7(moisten with sterile water, cover with IntraSite Conformable, cling film, and crepe bandage. Secure with Hyperfix)
The exudate from the wound determines the number of dressing changes required.
Acticoat is a silver impregnated antimicrobial barrier dressing. Acticoat can stay intact for 3 days and Acticoat 7 for up to 7 days. Acticoat needs to be activated by moistening it with Sterile water before applying it on the wound bed. Ensure dressing is moist not wet to avoid maceration of the wound. The moisture releases the silver that protects the wound from bacterial contamination. the Acticoat can be applied either side to the wound.
IntraSite Conformable is a conformable hydrogel dressing that combines the advantage of IntraSite gel with a non woven dressing. It creates a moist wound environment.

Full thickness
In a full thickness burn, injury occurs to the entire thickness of the epidermis, epithelial elements and dermal appendages. Spontaneous healing is not possible. If left, the area will heal by contraction thus reducing function. A full thickness burn is usually characterised by its whitish leather appearance but it can also be brown, cherry red or charred black. It is firm and leathery in texture. Few, if any, blisters are present. Those blisters that are present are thin walled and break easily and should be debrided. Areas will not blanch under pressure. Initially, nerve sensation is greatly diminished or lost completely when the injury is sustained. Later pain associated with the burn area can be severe as the child undergoes grafting.
The eschar of a full thickness burn is extremely inelastic and leads to compression of the underlying tissues as oedema occurs.
A closed dressing could be used:
Generally we use ActicoatTM or Acticoat 7TM(as per consultant choice) moisten with sterile water, covered with IntraSite ConformableTM, cling film (eg Gladwrap), and crepe bandage. Secure with Hyperfix and Tubigrip.
|

1- Apply moisten Acticoat to the burn wound
|
|

2- Cover the Acticoat with a layer of Intrasite Conformable
|

3- Secure the Intrasite Conformable with Hypafix tape to prevent slipping
|
|

4- Cover the Intrasite Conformable with a layer of cling wrap to keep moisture within the dressing
|

5- Secure the entire dressing with Hypafix / Mefix tape
|
|

6- Apply Tubigrip / bandage over the dressing for support
|
Different dressings may be used. The decision to use other dressings is made by the consultant.

Facial/respiratory burns
More people die in a fire from pulmonary insufficiency caused by the inhalation of heat and smoke, than they do from the direct burn injury, thus airway management is a priority. With the advent of new furnishing materials, we are seeing a more complex form of injury.
Inhalation injuries are uncommon in children, but are potentially more dangerous than in an adult because of ;
- the diameter of the child's airway is smaller and more prone to obstruction by a given degree of oedema
- the chest wall is soft and immature
- less respiratory reserve - respiratory failure from fatigue is more likely
- greater metabolic demands, including oxygen consumption are compounded
- the younger the child the greater the risk of respiratory distress, with increased mortality
- greater fluid requirements for fluid resuscitation.
Supraglottic oedema, laryngeal oedema or upper respiratory tract obstruction can develop as a result of a direct thermal injury such as the inhalation of flames, steam and the aspiration of hot liquids, or the inhalation of a chemical agent. Superheated air can transmit sufficient heat throughout the respiratory tract resulting in damage to lung tissue. If a child requires intubation, they will be nursed in the Intensive Care Unit. Occasionally, a tracheostomy may be indicated if prolonged respiratory support is required.
Signs of respiratory burn will be singed nasal hair, facial burns, blood stained sputum, carbonaceous sputum, oedema in the neck and facial area, respiratory distress, uneven noisy respirations, shallow breathing, tachypnoea, stridor, hoarseness, changes in mental state, restlessness, cyanosis and eventually loss of consciousness. Even if there are no signs present, children burned in an enclosed space must be considered to have an inhalation injury until disproved. Upper airway obstruction may result due to inhaled smoke even in the absence of cutaneous burns on the face.
Symptoms of hypoxia and respiratory distress may be delayed, but usually occur within the first 24 hours. Progressive obstruction may occur rapidly and careful observation is necessary for early detection and intervention.
In a facial burn, injury to the eyes, nose, mouth and ears are checked and treated accordingly. Facial burns need frequent cleansing with normal saline as exudate collects below eschar and may lead to infection and a delay in the healing process. Vaseline is applied twice a day after the face is cleaned. It can be reapplied as required if the wound becomes dry.
It must be explained to the child and family that facial oedema will occur. This usually peaks 48 hours post injury. Parents often do not recognise their own children and nursing staff need to explain that this oedema resolves itself in a few days.
Eyelids and ears may be swollen, thus impairing sight and hearing. Frequent eye toilets and the use of Chloromycetin ointment is necessary until swelling subsides sufficiently.
Lip swelling and oral burns can make it difficult for the child to maintain adequate oral intake so a Nasogastric tube may be required and NG feeds commenced and mouth toilets given.
Facial tissue is highly vascular and heals quickly. If grafting is required a specially fitted pressure mask is worn as soon as grafts are stable. The current literature supports that a face should be left no longer than 21 days to heal and that early debridement is needed.
Refer Fact Sheet on
Kids health info for parents web site:
Facial Burns

Fluid resuscitation
Not required for a burn
<10%TBSA.
Burns Resusitation fluid is given for burns >10%. Formula used: TBSA 3ml/kg/TBSA% = 24/hr total. Give 1/2 of this volume in the first 8 hrs from the time of the injury.
Maintenance fluid is administered concurrently.(not included in resuscitation fluids)
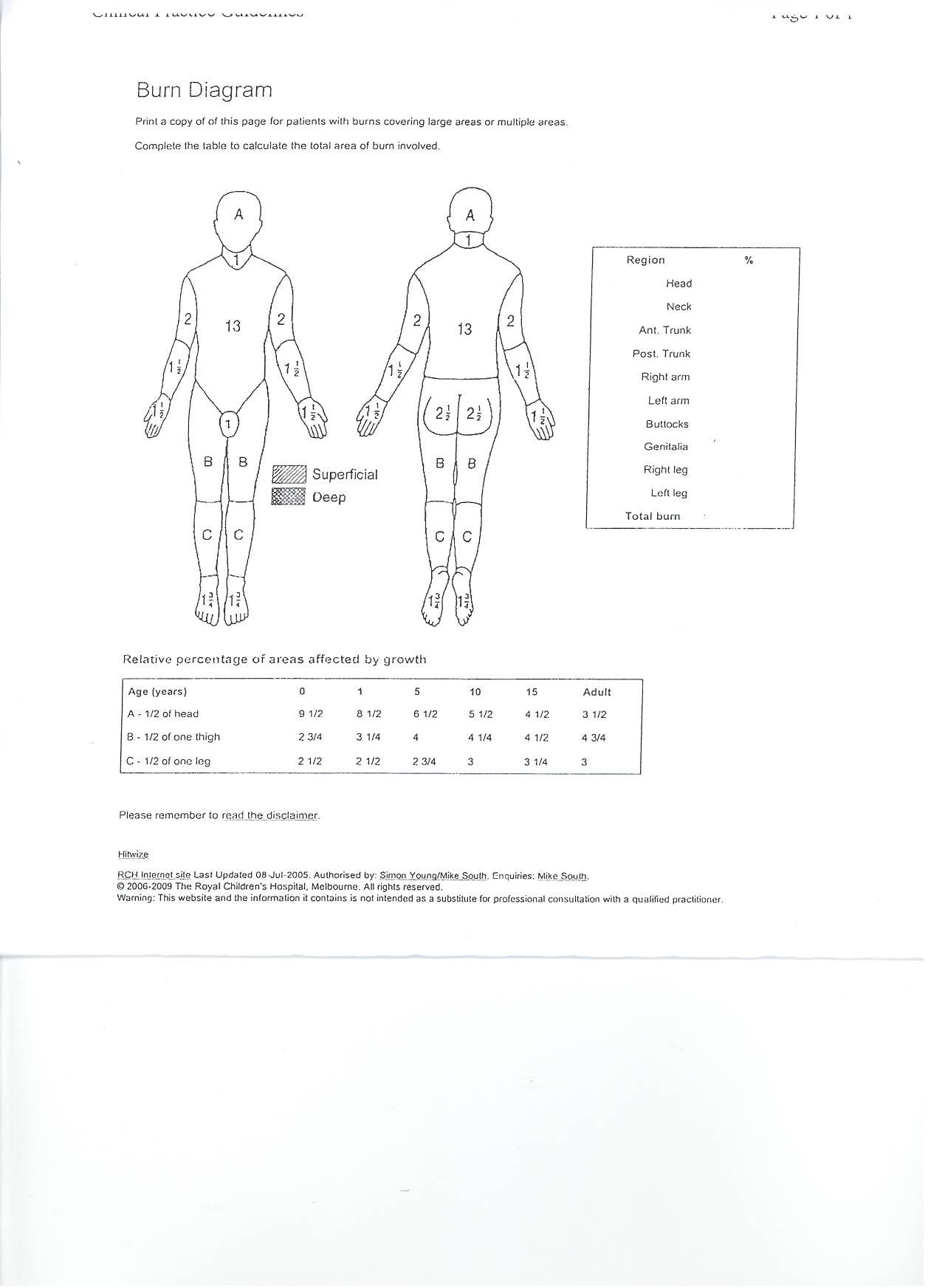
Lund and Browder chart
This assessment chart has been developed to assist health professionals to accurately calculate the percentage of burn surface area. It allows for the varying rates of growth in the head, thigh and lower leg of different age groups.
The "Rule of 9's" is inaccurate for paediatric patients - there is a modified "Rule of 9's" for paediatric use. The palmer method may also be used - the size of the child's palm can be used to estimate 1% Body Surface Area.

Fluids
Please see attached a copy of the fluid resuscitation regime
A modified Parkland Formula is used to calculate Burs Resuscitation fluids at RCH.
3/kg/%TBSA - 24hr total
Half of this volume is given in the first 8 hrs from the time of injury.
The second half is given over the next 16hrs
Fluids used at RCH are :
- N.Saline
- 5% Dextrose & N.Saline (for maintenance fluids)
- Naso-gastric feeding can replace maintenance fluids
Nutrition

Escharotomies
Full thickness circumferential burns can cause a tourniquet effect. Early elevation of the affected area can help prevent the increase of oedema. Increased blood viscosity, localised oedema, eschar formation and reduced circulatory blood volumes results in venous stasis and ischaemia may result. When this occurs an escharotomy is performed by the consultant as a prophylactic measure to reduce the likelihood of further damage to the tissues that lie distally to the circumferential eschar.
The tension within the tissues is relieved by cutting the skin with a scalpel. The wound will gape open exposing fatty tissue and some bleeding will occur. The escharotomy is dressed with Acticoat Absorbent and Acticoat to the area around the escharotomy. Then apply IntraSite conformable, plastic wrap loosely and a loose bandage.
Limb observations are necessary, as is elevation to monitor the effectiveness of the escharotomy. Escharotomies are often performed in the the ward, however, if possible theatre is more appropriate.
Before the patient is transported or if 4 hours has elapsed since the injury and circulation appears compromised, the referring doctor should consider Escharotomies.

Admission to the Burns Unit
Firstly the patients are seen in emergency, wounds debrided and dressed and then transferred to Platypus or Possum Ward.
These guidelines are followed:
Smaller burns can be dressed with a closed dressing and reviewed in outpatients.
Any child >10%TBSA should have the following :
- Fluid Resuscitation
- IDC on 1hrly measures
- NG tube with feeding started within 6 hours
- Strict Fluid Balance
- Flame burns/ burns that are oozing are to be dressed with Acticoat
- Scald burns can be dressed with Mepilex Ag or Acticoat
- Any Circumferential burns to have 1 hourly Colour, Warmth, Movement and Sensation and the limb elevated
As always there are circumstances that warrant a change from these guidelines, this can be discussed with the consultant on call

When to transfer
Types of Burns Requiring Admission at The Royal Children's Hospital
All Burns with a surface area greater than 10%, except very superficial burns.
All full thickness burns except those that are extremely small. (All burns to face, ears, eyes, hands, feet, genitalia, perineum or a major joint. Even if less than 5%.)
- Electrical burns (including lightening injury)
- Chemical Burns
- Burns associated with significant fractures or other major injury, in which the burn injury poses a significant risk of morbidity or mortality
- Inhalation burns of any nature (ICU admission)
- Burns in children under the age of 12 months (emergency transfer may not be required but assessment should be made)
- Small area burns - in patients with social problems, including children at risk
- Any other patient that is deemed appropriate on consultation
Note: For those requiring admission the consultant on call must be notified.

Antibiotics
Systemic antibiotics are not routinely prescribed. They are only given when a known infection is present and they are altered according to their sensitivities. The prophylaxis use of antibiotics does not reduce the risk of infection.
In the early post burn phase, febrile episodes are common, they do not necessarily indicate infection, but they do warrant close monitoring. These episodes are usually related to large amounts of pyrogens that are released as a result of the burn injury.
A wound swab is used for diagnosing infection in burnt areas.
In theatre, when grafting, Prophylactic antibiotics are given if the patient is not already on antibiotics.
Common antibiotics used are :
- Flucloxacillin
- Gentamycin

Blisters
The care of blisters depends on their size and location.
If the blisters are not large and will not obstruct the dressing, they can be left alone. The fluid within the blisters is sterile and therefore offers protection of the underlying skin.
If large bulbous blisters are present that are obstructing a dressing or restricting circulation to a limb/digit it is necessary to puncture the blister, release the serous fluid and debride the skin so that the dressing is compact and in contact with the skin.
When left intact, after a few days, if the fluid within the blister is opaque and infection is suspected, the blistered epidermis should be removed completely. Loose epidermis from broken blisters should be trimmed off if floating free. It should be noted that bleeding can occur if removal is attempted while it is still adherent.
If purulent fluid is present within a blister, it should be deroofed, and swabbed for infection. On the hand or sole, white keratin can be associated with blistering and such loose keratin (which has no sensation) can be excised if floating free.

Non accidental injuries
ERC are on call to have photos taken, please page them through switch (anytime)
Where to get more information