Introduction
Aim
Definition of terms
Pressure injury development
Prevention
Management
Referral
Documentation/communication
Discharge
Evidence Table
Introduction
International data indicates that hospitalised children and neonates experience pressure injuries at a high incidence rate, up to 27% (EPUAP/NPIAP/PPPIA, 2019). Children and neonates are at higher risk due to their relatively larger skin surface area, increased nutritional requirements and risk of nutritional deficiencies, immature skin and the use of medical devices. Pressure injuries are associated with increased morbidity and hospital stay, as well hospital costs. Most pressure injuries are preventable if appropriate evidence-based measures are implemented, including comprehensive risk assessment, skin care and targeted prevention strategies.
Aim
The aim of this guideline is to increase awareness of pressure injuries amongst health care professionals at the Royal Children’s Hospital (RCH). The primary objectives are to provide evidence-based guidance for the prevention, assessment and management of pressure injuries.
Definition of terms
Blanching Erythema - Reddened skin that becomes white or pale in appearance when light pressure is applied.
Extrinsic Factors - Originating external to the body.
Intrinsic Factors - Originating internal to the body.
Pressure Injury (PI) - Is a localised area of tissue destruction that develops when soft tissue is compressed between a bony prominence, as a result of pressure, shearing forces and/or friction, or a combination of these.
Risk Assessment Scale- A formal grade used to help ascertain the degree of pressure injury risk. At the Royal Children’s Hospital a modified Glamorgan Risk Assessment Scale is currently used.
Re-perfusion Injury- A re-perfusion injury is a response that the tissues have that results in damage to the cells when blood supply returns back to the tissue after a period of ischemia or lack of oxygen.
Induration – A hardened mass or formation of the skin tissue due to increase in fibrous elements commonly associated with inflammation and marked loss of elasticity and pliability of the skin.
Pressure injury development
A pressure injury is defined as localised damage to the skin and/or underlying tissue as a result of pressure.
PIs commonly occur over bony prominences, however in the paediatric population, PIs are more commonly associated with a medical device or object. In addition to pressure, poor blood flow, friction, shear, and tissue ischaemia can all contribute to the develop of a PI. The deep fascia, subcutaneous fat, skin, bone, and muscle can all be damaged by unrelieved pressure.
The tissues’ ability to tolerate the pressure including the intensity and duration, are factors affecting PI development. Prolonged pressure on a localised area of tissue causes the occlusion of blood flow, preventing the supply of nutrients and oxygen to the tissue, resulting in ischaemia and re-perfusion injury. This leads to cell obliteration and eventually tissue death.
Factors associated with increased risk
Several factors may influence an individual’s risk of developing pressure injuries. In the prevention of PIs, it is essential that patients at risk are identified so an individualised prevention plan can be implemented to mitigate the risks. A risk factor is any element that either diminishes the skins tolerance to pressure or contributes to increased exposure of the skin to excess pressure.
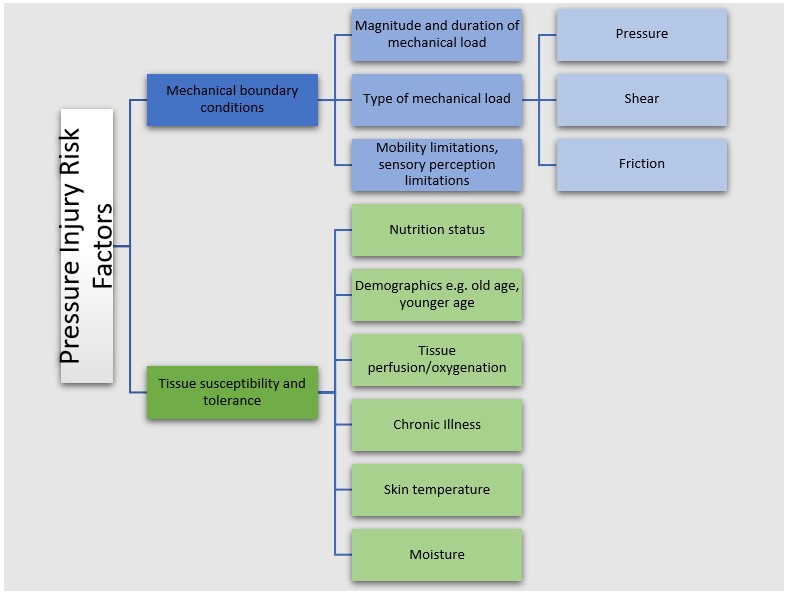
(Adapted
from the Prevention and Treatment of Pressure Ulcers/Injuries International
Guideline 2019)
Prevention
Prevention requires an on-going risk assessment, consideration of casual factors, implementation of prevention strategies and the selection of an appropriate use of support surfaces. When an assessment identifies a patient at risk of pressure injury, interventions should be implemented immediately.
Pressure injury risk assessment
PI risk assessment tools are the key to determining if a patient is susceptible to PIs. Validated risk assessment tools for children are effective for identifying those at risk and increasing awareness of potential pressure related injuries, however they cannot embody every possible circumstance. Therefore, clinicians need to use their experience, clinical judgment and knowledge to prevent tissue damage and protect the skin in conjunction with the risk screening tool.
The pressure injury risk assessment tool used at RCH is a modified Glamorgan Pressure Injury Risk Assessment Tool.
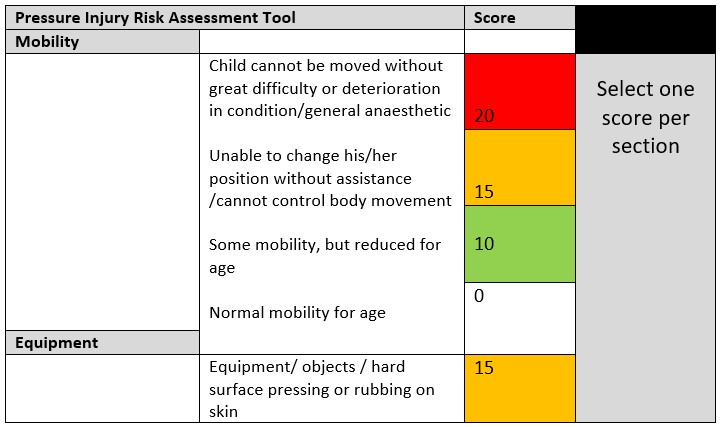

(Adapted from the Glamorgan Risk Assessment Scale from the United Kingdom)
Nursing responsibilities
Every inpatient at RCH should have a Glamorgan Pressure Injury Risk Assessment Tool completed:
- On admission or as soon as practical after the admission (within six hours).
- At the commencement of every shift as required nursing documentation.
- When a patient’s condition changes.
- When the patient is transferred from one ward/department to another.
Once completed, the risk assessment should be documented on the Primary Assessment flowsheet within the EMR.
Any patient deemed “At Risk” (risk score of +10) of pressure injury should have an individualised prevention plan developed and documented in the Primary Assessment flowsheet in the EMR. This plan should be reviewed for appropriateness following every pressure injury risk assessment completion.
If a patient’s pressure injury risk assessment score changes, a new pressure injury prevention plan needs to be completed and implemented to address the new level of risk.
Skin assessment
Skin assessment is key to pressure injury prevention, classification/diagnosis, and treatment. All inpatients should have a skin assessment to determine its’ general condition and identify factors that increase the risk for PI development. The status of the patient’s skin is the most important
early indicator of the skin’s reaction to pressure exposure and the continuing risk of pressure injury.
Conducting the assessment
Complete a general visual check of the skin including analysis of the entire skin surface to assess its integrity and identify any characteristics indicative of pressure damage.
Monitor and check the skin beneath dressings, prosthesis and devices when clinically appropriate.
Check for areas of localised heat, skin breakdown, oedema, areas of redness that do not blanch and induration of the wound.
Particular attention should be paid to areas of bony prominence, which are at an increased risk for pressure injury due to pressure, friction and shearing forces. High risk areas include; sacrum, heels, elbows, wrists, temporal region of skill, ears, shoulders, back of head (especially in
children less than 36 months of age), knees, and toes.
Frequency of
assessment
As with the pressure injury risk assessment tool, a patient’s skin should be assessed;
- On admission or as soon as practical after the admission (within six hours).
- At the commencement of every shift as required nursing documentation.
- When a patient’s condition changes.
- When the patient is transferred from one ward/department to another.
- As well as, upon discharge (to ensure discharge planning is complete)
Document skin assessment findings in the Focused Assessment Flowsheet within the EMR.
Patient and family education
Parents and carers play a vital role in the care of their child; and therefore, their engagement is vital in helping to prevent the formation of pressure injuries. Carers and parents should be educated around the risk of their child developing pressure injuries whilst in hospital and be provided
with effective and age-appropriate strategies to mitigate these risks.
The
PI prevention factsheet should be provided to all carers and parents of patients that have been identified to be at risk of developing a pressure injury.
Nutrition and hydration
Malnourished children are at increased risk of pressure injury development due to their compromised ability to maintain healthy skin and mucosa. Hydration and nutritional support should be aimed at preventing and correcting these deficits.
Maintenance of a positive nitrogen balance and serum albumin levels are vital in maintaining adequate skin integrity and hydration. Monitoring patient weight loss as well as protein and micronutrient intake have been identified as key factors in nutrition to support immunity and
skin integrity.
- Patients at risk should be offered frequent fluids and diet to maintain adequate nutrition and hydration.
- Patients considered high risk or very high risk should follow the advice of the
Paediatric Nutritional Screening Tool and be referred to a dietician for assessment.
Moisture control and skin care
Increased moisture on the skin or excessive dryness can exacerbate pressure injury development due to the risk of skin breakdown and altered skin integrity.
Keep the skin clean and dry
- Clean skin daily to remove unwanted substances and allow to dry
- Do not vigorously rub or massage the patient’s skin
- Use a pH neutral or slightly acidic skin cleanser (pH 4-7) ~ Alkaline products (pH >7) should be avoided.
- Utilise a fragrance-free moisturiser to avoid dryness (e.g. SorboleneTM)
Investigate and manage incontinence
- Clean skin promptly after episodes of incontinence
- Use appropriately sized incontinence products for maximum absorption
- Consider referral to occupational therapy if the child was previously continent and support with return to toileting is required
Apply barrier creams
- Barrier creams place a physical barrier between the skin and contaminants that may irritate skin and cause breakdown.
| Area |
Treatment aim |
Treatment/product |
| Low-risk areas/normal skin hygiene |
Support skin health and maintain hydration |
Mild pH,
fragrance-free moisturiser e.g. SorboleneTM |
| High-risk areas (e.g. nappy region) |
Create a protective physical barrier from moisture and irritants that promotes skin health and healing |
Barrier wipes e.g. 3MTM CavilonTM No Sting Barrier
Wipes.
These wipes create a transparent barrier preventing incontinence associated skin irritation and nappy rash without impacting the absorbency of incontinence products. When used in nappy cares, barrier wipes have been shown to decrease redness and pain by preventing breakdown and can be used in a similar way to
traditional barrier creams. Barrier wipes also allow for ongoing integumentary assessments and do not require removal.
Zinc-oxide based creams e.g. Sudocrem® |
| Broken down skin |
Promote skin healing and prevent further breakdown in areas that are red or excoriated |
Zinc-oxide based creams e.g. Sudocrem®
Consultation with medical team/Stomal Therapy Clinical Nurse Consultant if required. |
Mobility and positioning
- Consider the patient’s baseline level of mobility and their current level of mobility
- For patients who can move independently or assist in moving themselves, it is recommended that they be encouraged and/or assisted (as required) to change their position regularly, either in bed or out of bed (if able).
- For patients who are unable to assist with moving themselves, it is recommended that they be repositioned every two hours. Employ appropriate manual handling techniques in line with Occupational Health and Safety guidelines when transferring and repositioning patients. Please refer to the
Smart Move Smart Lift Training Program.
- Positions will vary based on age, developmental stage, physical ability and medical stability; however, they may include lying in bed in a prone, supine, left side lying, or right side lying position, seated in bed, seated in a chair or on a parents’ lap, or playing on a floor
mat. Pillows or rolled towels can be used to help maintain a change in position.
- For high-risk patients, limit time spent sitting in bed with head elevated > thirty degrees to no more than two hours due to the increased pressure on the sacrum.
- Always check the positioning of the bony prominences (e.g. shoulders, elbows, ankles, ears) and heels when repositioning the patient into any position. Heels should be suspended off the bed using pillows or gel pads for patients spending prolonged periods in bed
- Consider smaller more frequent (e.g. hourly to two hourly) shifts in position of patients who cannot tolerate major changes in body position to redistribute pressure (e.g. Patients with Pulmonary hypertension, on ECMO Support)
- Patients in pain are at an increased risk of pressure injury. If pain is managed appropriately, they are more likely to move or be moved at frequent intervals. Monitor the patient's level of pain and ensure appropriate
pain relief is provided to support and encourage mobility. Refer to
Pain Management
Clinical Practice Guidelines. Ensure the analgesia has adequate time to take effect prior to attending to pressure area care to reduce the patient’s pain on moving - this will be dependent on the medication itself and the route of administration (i.e. IV vs oral).
- For patients at higher risk of pressure injuries or with existing pressure injuries requiring additional support to manage their mobility and positioning, consider referral to:
- Physiotherapy referral for assistance/advice on positioning and repositioning, transferring and supporting mobility
- Occupational therapy referral for assistance/advice on positioning and repositioning and selection of the most appropriate support surface
Friction and shear
- For patients who are unable to assist in moving themselves, use appropriate transfer assistance devices (e.g. hoist, slide sheets) to reduce friction and shear forces. Always lower the bed head before repositioning patients.
- Do not use incontinence bed pads to move/slide patient up the bed
- To reduce shear forces on the sacrum, the head of the bed should be raised in conjunction with the knee bend and/or pillows under the knee
Medical devices
Any object that comes into direct contact with the patient’s skin has the potential to cause a pressure injury. This is exacerbated in the paediatric inpatient population with device related pressure injuries causing the majority of all paediatric pressure injuries due to the immature skin
barrier and decreased tissue tolerance. With increasing complexity of care and advances in technology, incorporating more devices into patient care, nurses must correctly assess and protect a patient’s skin from the formation of device related pressure injuries.
Key points
- Regular repositioning and inspection of the patient to ensure that they are not unintentionally lying on devices
- Conduct more frequent assessments at the skin-device interface in patients vulnerable to fluid shifts and exhibiting localised or generalised oedema
- Use the correct size equipment suitable to the patient’s anatomical size
- When equipment is secured to the patient using tapes, ensure that they are not applied too tightly and that where possible they have some elasticity and stretch (e.g. Hypafix®, TegadermTM)
- Use the minimal amount of strapping or tape to safely secure the device to allow for maximal visualization of the patient’s skin
- Devices that are unable to be easily repositioned should be managed with appropriate dressing and skin care
General advice
Prior to the application of medical devices and associated preventative dressings, barrier products (e.g. 3MTM CavilonTM No Sting Barrier Wipes) should be used as a transparent barrier to protect the patients skin. These products repel moisture and provide protection from fluids and friction,
which can prevent skin breakdown in areas with frequent dressing changes or repositioning.
Dressings should be changed as appropriate or when soiled, however removal within the first 24 hours of application should be avoided due to the increased risk of sheering force that can cause trauma to patient skin.
Where appropriate adhesive removal products (e.g. Convacare® removal wipes) should be used to promote comfort and reduce skin trauma when dressings are difficult to remove.
High risk patient populations
Patients in the operating room
Pressure injuries that originate in the operating room may not appear until one to four days post-operatively, highlighting the importance of thorough skin assessment and prevention interventions as the child continues their journey through the pre-operative,
surgery and post-operative phase at the RCH.
Pre-operative –
Before going to theatre, the perioperative nurse performs a pre-operative assessment to assess for factors that may increase an individual child’s risk for pressure injury during surgery. Assessment taken should be documented on the pre-operative assessment through EMR. Factors that should be assessed include:
- Medical devices (catheter, tubes, drains)
- Jewellery or body piercings
- Braided hair, hair accessories, hair extensions
- Implants
- Prosthetics
- Comorbidities
- Skin condition
- Nutritional status
Intra-operative -
Research suggests surgery that lasts longer than two hours has been associated with an increased risk of PIs. Anaesthetised patients that are positioned on specialised frames in the prone position, may be at an even higher risk of developing PIs in uncommon areas such as the: chest, iliac crest, face (tip of
the nose, chin and forehead) and heels.
There are many factors that contribute to the incidence of PI’s in the operating theatre such as:
- Intense or prolonged pressure during lengthy surgical procedures.
- Increased pressure on bony prominences from positioning.
- Exposure to friction or shear during transfer to the operating table and positioning.
Risks for patients undergoing surgery should be determined by:
- Length of the operation
- Increased hypotensive episodes intra-operatively
- Low core temperature during surgery
- Reduced mobility on day one post-operatively
- Prolonged placement of equipment and medical devices e.g. neurosurgical head frame, arm boards, monitoring equipment.
The RCH operating tables are all fitted with high density pressure-redistributing foam to reduce the risk of pressure injury development. Other methods of managing a patient to reduce the risk of pressure injuries include:
- The use of Gel Pads and Perspex boxes for complex theatre cases.
- Patients should be positioned to reduce the risk of pressure injury development during surgery.
- Heels should be completely elevated in such a way as to distribute the weight of the leg along the calf without putting all the pressure on the Achilles tendon. The knee should be in slight flexion.
- Hyperextension of the knee may cause obstruction of the popliteal vein, and this could predispose the individual to deep vein thrombosis.
- Pay attention to pressure redistribution prior to and after surgery. Position the individual in a different posture pre-operatively and post-operatively than the posture adopted during surgery where possible.
- Patient supports and patient positioning aids, including the most appropriate support surface
- Actions/interventions taken should be documented on the EMR intra-operative nursing record including patient positioning and assessment of the integumentary system.
Post-operative -
In the postoperative phase, a full integumentary assessment is required. Any altered skin integrity must be documented on the EMR flowsheet and communicated to the multidisciplinary team.
Neonatal patients
Pressure injury prevention in this specialised population should be managed carefully, considering the effect of various dressing and barrier products on underdeveloped skin. Consultation with neonatal specialists is suggested before application of new products.
Please refer to the
Neonatal and infant skin care Clinical guideline for further information on the management of neonatal skin and prevention of pressure injuries.
Paediatric intensive care patients
Patients admitted to the Paediatric Intensive Care Unit (PICU) have a higher incidence of PI’s and are usually more severe due to patient complexities and prolonged length of stay.
The ICU environment has several main contributing factors:
- Multiple invasive devices
- Low cardiac output state
- Inotrope, vasopressor and muscle relaxant use
- Impaired level of consciousness
- Immobility
- Poor peripheral and central blood flow
- Suboptimal nutrition
Patients should have existing PIs assessed every second hour and be repositioned based on their mobility status identified daily on medical ward from the ‘Early Mobilisation Traffic Light Guideline’. If the patient is identified as too clinically unstable to attend to major pressure area care and repositioning, an alternative pressure injury prevention plan needs to be discussed with the multidisciplinary team.
Orthopaedic patients
Orthopaedic patients are considered to be at high risk of pressure injuries due to the prolonged presence of fixed devices such as external fixation, traction, plasters casts and braces. These devices can cause sheering force and friction, so should be regularly monitored and
assessed. These patients are also at higher risk of immobilisation due to painful procedures and extended periods of bed rest or reduced weight bearing capacity.
- Elevation of limbs on pillows and towels where possible to reduce pressure, particularly on the heels
- Monitoring of neurovascular compromise or increased pain levels as this can decrease skin integrity and indicate the formation of pressure injuries
Neurovascular Observations Guideline
- Orthopaedic patients with developmental delays are at increased risk of pressure injuries due to their compromised ability to communicate changes in sensation. Therefore, pain cues should be monitored closely in this population.
- Patients with epidural analgesia should adhere to strict pressure area cares and frequent repositioning as they have extremely compromised movement and sensation
Epidural Analgesia Nursing Management
- Referral to Prosthetics + Orthotics for review of braces/splints/collars where required
Support surfaces
Support surfaces are devices (e.g. air mattresses, cushions) that are used to assist with pressure redistribution to manage the pressure load on the integumentary system. Support surfaces typically support pressure redistribution through either immersion to increase the body surface area in contact with the surface,
or by alternating and offloading the area of the body in contact with the support surface.
Decisions about an appropriate support surface to use for pressure injury prevention should be based on an overall assessment of the patient, including their weight, and their Glamorgan screening tool score. Selection of an appropriate support surface should also take into consideration factors such as the
individual’s level of mobility within the bed, his/her comfort, and the need for microclimate control. The LINK Bariatric Procedure should be referred to for guidance regarding suitable support surfaces for patients above 100kg.
For support surfaces to be effective, there must be minimal layering in between the device and the person. The use of additional sheets, kylie pads, dry-flows and towels can alter the pressure relieving qualities of pressure redistribution equipment and should be avoided where possible. A single
sheet that can be kept dry and crease free is optimal.
Please note: support surfaces facilitate the redistribution of body weight but do not negate the need for regular repositioning of patients or pressure area care. For patients that are very high risk, these surfaces may allow a decrease in turning frequency overnight to 3-4
hourly to encourage rest patterns, however, this should be considered carefully on a case-by-case basis. If the patient is spending time sitting with the bed head raised, the mattress should be checked to ensure it is not ‘bottoming out’ underneath the patient.
Please consider the sudden infant death syndrome (SIDS) risk reduction recommendations when using support surfaces for infants. Monitoring is required for infants nursed outside of these recommendations.
Consider Occupational Therapy referral for assistance with assessment of causal factors and advice on pressure injury prevention or management plans, including selection of most appropriate support surfaces.
The following should NOT be used as a support surface:
- Sheepskins
- Doughnut shaped gels – this type of device may impair lymphatic drainage and circulation*.
- Water filled gloves under heels – these are not effective as the water filled glove is unable to redistribute pressure and it only supports a small surface of the heel.
*Note: doughnut shaped gel rings are still currently used in special
circumstances in operating theatres only with careful consideration and
application. Assessment of the occiput and surrounding tissue should take place
before and after doughnut shaped gel ring use.
Characteristics of support surfaces
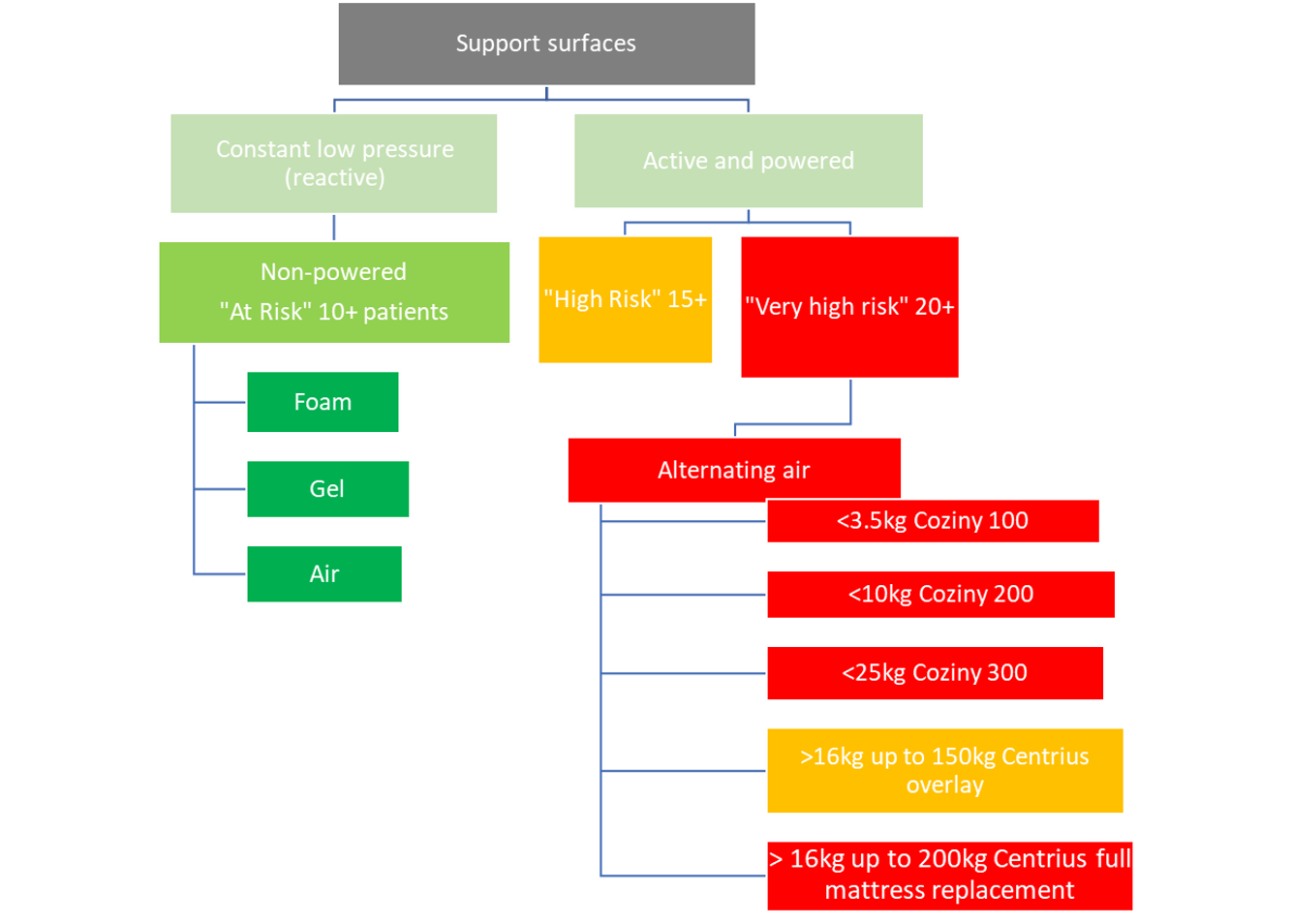
Please see the table below for further information regarding the pressure mattresses available for use at RCH.
Alternating air mattresses
At RCH, all pressure mattresses available for patient use are on consignment (externally managed Keystone Healthcare Supplies) and are available through bed pool.
| Patient Weight Range |
Bed Utilised |
Pressure Mattress |
Notes |
|
<3.5kg |
Radiant warmer |
Coziny 100 |
Not compatible with x-ray due to artefact. Patient must be lifted and x-ray board placed directly under patient not mattress. |
|
<10kg |
Radiant warmer |
Coziny 200 |
Replace foam mattress with the pressure mattress |
| Cot |
Coziny 200 |
Place pressure mattress on top of the foam mattress |
|
<25kg |
Cot |
Coziny 300 |
Replace foam mattress with the pressure mattress |
| Bed AND nursed 1:1 e.g. in PICU |
Coziny 300 |
Place pressure mattress on top of the foam mattress |
| 16kg-150kg |
Bed |
Centrius Overlay |
Place pressure mattress on top of the foam mattress |
| 16kg-200kg |
Bed |
Centrius full mattress replacement |
Replace foam mattress with pressure mattress |
Pressure mattress ordering process
For ordering information please see the below document:
Link to 2022 Keystone pressure mattress ordering workflow
Management
Pressure injury stages
Pressure injury staging or classification describes the extent of skin and tissue damage. Staging of a pressure injury is essential for the development and implementation of a management plan.
Quick reference table:
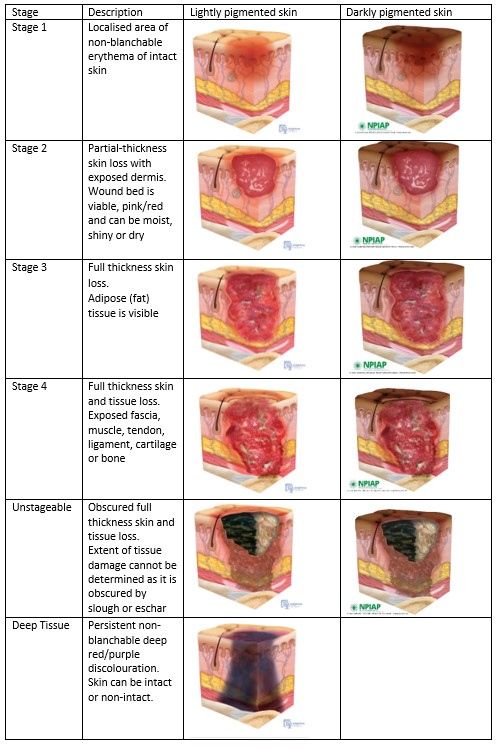
Adapted from the National Pressure Injury
Advisory Panel (NPIAP) Pressure Injury and Stages Poster September 2016
For further information regarding pressure injury staging please refer to the
NPIAP Pressure Injury Staging Poster.
Pressure injury/wound management
Basic
principles
- Avoid positioning patients directly on an existing pressure injury or body surface that remains damaged or erythematous, where possible
- Ensure the patient is on the most suitable support surface. Consider referral to Occupational Therapy for further advice/support if required.
- Always consider patient nutrition and hygiene and refer for support if required
Wound management
- Utilise appropriate pain management (see comfort kids procedural support LINK)
- Clean the pressure injury with sterile water or 0.9% sodium chloride solution
- If required, debride dead or devitalised tissue. This can be done using autolytic debridement through dressing selection or surgical debridement
- Assess and document the size and appearance of the pressure injury in the LDA (see below)
- Select a wound dressing that promotes a warm, moist environment for wound healing (see table below)
- If the wound appears infected antibiotics can be used. Topical antiseptics are not routinely used on pressure injuries, but topical antimicrobials should be considered if clinically indicated
- Remove dressings with adhesive remover wipe or spray to gently remove tapes
- Do not use gauze to treat pressure injuries
- Wound management plan should be documented in the EMR progress notes
| Stage |
Management Goals |
Dressing
Selection |
|
Stage 1
Non-blanchable
erythema |
Protect skin to prevent further injury |
Silicone
adhesive, non-adherent foam or transparent hydrocolloid adhesive dressing
- Silicone e.g. Mepilex® Border, Mepilex® Lite or AllevynTM helps to reduce effects of friction and can be left in-situ for 7 days (must be changed if soiled)
- Hydrocolloid e.g. Comfeel® has very little a sorbency so should only be used on wounds with no or low exudate. It should only be used if it can be left on for 7 days
- Apply 3MTMCavilonTM No Sting Barrier wipe underneath to prevent adhesive trauma upon removing the Comfeel®
|
| Stage 2 Partial thickness
skin loss |
Relieve pressure and protect wound from further trauma/ contamination |
Silicone adhesive
or non-adherent foam
- Silicone e.g. Mepilex® Border, Mepilex® Lite or AllevynTM has an absorption layer that draws moisture and exudate from the wound while protecting the surrounding healthy skin from maceration. It mounds well to the skin without
sticking to the wound
- Silicone dressings can be left on for up to 7 days but should be changed PRN depending on exudate/ as guided by stomal therapy
- Silicone properties prevent trauma upon removal
REFERRAL TO STOMAL THERAPY CLINICAL NURSE CONSULTANT |
|
Stage 3
Full thickness
skin loss |
Relieve pressure and protect wound from further trauma/ contamination |
Hydrogel,
Adhesive foam, Hydrofiber or Silicone dressing
- Hydrogel e.g. IntrasiteTM Gel absorbs slough/exudate while creating a moist healing environment
- Hydrofibre e.g. Aquacel® is 100% sodium carboxylmethyl-cellulose which converts to a soft gel when in contact with wound exudate to absorb exudate and maintain a moist wound environment for healing
REFERAL TO STOMAL THERAPY CLINICAL NURSE CONSULTANT |
|
Stage 4
Full thickness
tissue loss |
Relieve pressure and protect wound from further trauma/ contamination |
Alginate,
Hydrogel, Adhesive foam, Hydrofiber or Silicone dressing
- Alginate dressings e.g. Kaltostat® are used when there is active bleeding. It is made from brown seaweed and forms a gel when in contact with a wound surface to absorb the exudate and promote haemostasis
CONDSIDER REFERRING TO PLASTIC SURGERY TEAM |
| Unstageable Depth unknown |
Unable to determine prior to debridement |
Surgical
debridement required as determined by surgical team |
For further information regarding dressing types/ordering and wound management please refer to the RCH dressing selection resources:
Wound Dressing Product Reference Guide
Dressing and Wound Management Poster
Dressing Supplies Ordering
Referral
Stomal Therapy
Clinical Nurse Consultant/Plastic Surgery Team
Every pressure injury that is Stage 2 or above, should be referred to the Stomal Therapy Clinical Nurse Consultant for opinion and management.
For a Stage 4 pressure injury and above, a referral to Plastic Surgery Team should be considered.
Physiotherapy/Occupational therapy
For patients at high risk of pressure injuries or with an existing pressure injury consider referral to:
- Occupational Therapy if additional support with assessment of causal factors and advice on pressure injury prevention or management plans, including selection of most appropriate support surface is required
- Physiotherapy if assistance/advice on positioning and repositioning, transferring and supporting mobility is required
Documentation/Communication
All pressure injuries need to be carefully documented. If a pressure injury is identified the following process should be followed;
EMR
documentation
- Create an EMR progress note and document the following;
- Likely causal factors e.g. medical device related, moisture, immobility etc.
- PI staging, appearance, measurement (wound size and depth), exudate and odour
- Add the pressure injury as a “non-surgical wound” LDA on the Avatar, selecting “pressure ulcer” as the primary wound type
- Capture clinical image of the PI with patient/family consent) and upload to patient’s file
- Complete LDA assessment of pressure injury every shift
Communication
- Notify medical staff and nurse in charge of shift about the pressure injury
- Inform the patient, family and/or carers about the pressure injury and management plan
- Ensure a detailed description of what is observed, and the action taken is included in clinical handover
VHIMS
Report the pressure injury on the hospital reporting system
Victorian Health Incident Management System (VHIMS) and confirm the stage of the pressure injury is included.
Patients with identified pressure injuries should be managed as high or very high risk regardless of their identified Glamorgan Risk Assessment Score. This assessment should be documented in EMR under the pressure prevention plan.
Discharge
If the patient is being discharged with a change in their function and associated higher level of pressure care risk than pre-admission, an appropriate management plan must be in place. This may include:
Goals of care: Patients who are returning home with considerable changes to their mobility should have goals of care established by the multidisciplinary team in collaboration with the patient and their caregivers. Particularly those patients
receiving palliative care, appropriate goals should be established and included in the patient’s management plan. Multiple risk factors and general poor health significantly increases the risk of pressure injuries. Palliative care may have a stronger focus on managing
symptoms, comfort and quality of life.
Education: Education of patients, parents and carers is essential in the prevention and management of pressure injuries. Patients and their families should have a clear understanding of the potential impact of a pressure injury and the importance of its prevention, contributing risk factors
and strategies that assist in reducing the risk. This is particularly important when patients are in a home care environment or being discharged from an inpatient area. Families and carers of patients discharged with risk factors should receive a
pressure injury prevention factsheet and discuss suitable prevention strategies relevant to their child prior to discharge.
Equipment: If the patient is currently on a support surface and requires this for use on discharge, refer to Occupational Therapy.
Evidence table
Pressure Injury Prevention Evidence Table
Please remember to
read the disclaimer
The development of this nursing guideline was coordinated by Lexie Miller, Improvement Manager, Jade Grillo, Platypus, and Ashlee Cruz, Occupational Therapy, and approved by the Nursing Clinical Effectiveness Committee. Updated April 2022.