Note: This guideline is currently under review.
Introduction
Aim
Definition of Terms
Assessment
Management
Common newborn rashes
Links
Evidence Table
References
Introduction
Preservation of skin integrity, reduction of risk factors and neonate skin care education for parents are key nursing priorities in the care of the term and preterm neonate.
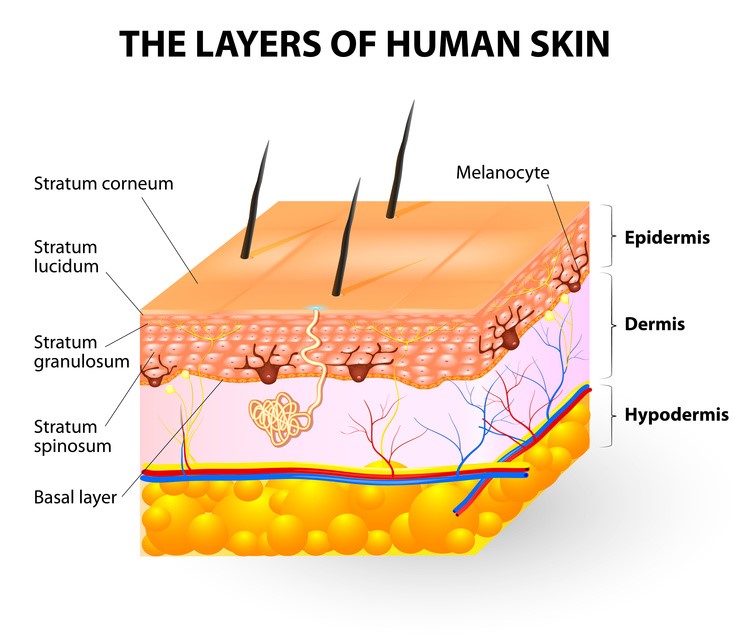
The skin contains three separate layers. The uppermost layer is the stratum corneum. This provides the barrier function of the skin and has 10-20 layers in adults and term neonates. It protects against toxins, irritants, allergens and pathogens, retains heat and water as well as maintaining a normal microbiome. During the first year of life the stratum corneum is not fully mature and is approximately 30% thinner than that of adult skin. Directly under the stratum corneum is the basal layer of the epidermis and then the dermis which are also thinner and underdeveloped in neonates compared to adults. In preterm neonates the stratum corneum has only 2-3 layers. This deficiency and immaturity of the stratum corneum results in increased fluid and heat loss leading to electrolyte imbalance, reduced thermoregulation and increased infection risk.
Understanding the physiological and anatomical skin differences of preterm and term neonate skin is important in aiding thorough assessment and appropriate management of the skin.
Please see
key differences in neonate skin for further information on the structure and function of neonate skin.
This
guideline provides recommendations for the skin care of neonates (birth to 28
days of age) of all gestational ages. Additional considerations for preterm
neonates and product suggestions are identified in the boxes below each
section.
Aim
To maintain skin integrity and minimise heat loss in the neonate requiring hospitialisation. This is achieved by understanding the key differences of preterm and term neonate skin enabling appropriate assessment and management of our neonatal population using evidence based practice.
Definition of Terms
- Atopy - Family history of eczema, asthma or allergic rhinitis
- Stratum Corneum - The outer most layer of the epidermis
- pH - Represents the acidity or alkalinity of a solution on a logarithmic scale where 7 is neutral,
< 7 is more acidic and > 7 more alkaline.
- Vernix Caseosa - Waxy white substance on newborn skin
- Layers of the Skin - Epidermis, Dermis and Hypodermis (subcutaneous tissue)
Assessment
Assessment of neonate skin should be undertaken daily, or more frequently as clinically indicated. Neonates at increased risk of systemic infection and longer hospital stays will be identified promptly. The Neonatal Skin Condition Score (NSCS) may be used to measure skin condition objectively.
NSCS Criteria
Dryness:
1 = Normal, no signs of dry skin
2 = Dry skin with visible scaling
3 = Very dry skin with cracking and/or fissures present
Erythema:
1 = No evidence of erythema
2 = Visible erythema (
<50% body surface)
3 = Visible erythema (>50% body surface)*
Breakdown:
1 = None evident
2 = Small and/or localized areas
3 = Extensive
Interpretation of the results
The relevant medical team must be notified if a neonate scores a single score of 3 in one area or a combined score of 6 and above. A dermatology referral may also be appropriate.
|
Management
Nappy Care
The perineal environment is prone to changes in the skin barrier causing skin irritation. Increased moisture, prolonged contact with irritants, and an alkaline skin surface may contribute to skin breakdown.
- Nappy changes should occur at regular intervals (where clinically appropriate) to avoid irritation to the perineal skin environment
- Evaluation of the perineal area is required at each nappy change to ensure early identification of perineal dermatitis and candida infections
- Disposable nappies are preferred
- Cotton balls or soft disposable towels (i.e. Rediwipes™) with warm water are the preferred cleansing method
- A pH neutral cleanser (see product suggestions in bathing section) may be used if stools are dry and difficult to remove
- Wipes should be avoided (if required they should be free from alcohol and fragrance)
- Barrier creams should be used on all neonates at risk of perineal dermatitis at every nappy change at the first sign of erythema or skin breakdown
- The removal of barrier creams between nappy changes is not necessary, rather apply another layer. Barrier creams containing plant extracts and/or fragrance should be avoided
- Risk factors for perineal dermatitis include: Frequent stooling; antibiotic use; malabsorption; opiate withdrawal; abnormal rectal sphincter tone
PRETERM INFANT CONSIDERATIONS
Nappy care for the preterm infant is as above and assessed on an individual basis
|
PRODUCT EXAMPLE
Cleansing: Rediwipes, cotton wool, pH neutral cleanser (as below in bathing section)
Barrier Creams: SudoCream™, Kenkay Zinc and Castor Oil cream™, Desitin™, Bepanthan™
|
Eye & Oral Care
- Routine assessment of the eyes and mouth (minimum 4 hourly)
- Assess for exudate, skin condition and moisture level
Eye Care
- assessment
should be utilised to identify abnormalities.
- If exudate appears, eyes should be wiped from the inner corner outwards with a single-use cotton ball soaked in 0.9% sodium chloride (NaCl)
- Exudate from the eyes can be a common occurrence in the neonate however, an increase in exudate, purulent in colour may signify an infection and as such required medical review
- The neonate with reduced functioning of the eyelids (i.e. preterm neonate, sedated/muscle relaxed neonate) will require routine eye care to maintain lubrication.
- Minimum 4 hourly cleaning of the eyes with 0.9% NaCl from the inner corner outwards with a single-use cotton ball
- Application of a lubricating eye ointment
- Monitor for signs infection and abrasion
Oral Care
The term neonate with normal anatomy and physiology of the mouth does not require routine oral care. Routine assessment should be utilised to identify abnormalities.
- The neonate requiring regular oropharyngeal suction; intubation or other oral supportive devices (i.e. replogle tube) will require routine oral care to reduce injury to the lips and oral mucosa as follows:
- Minimum 4 hourly cleaning of the lips with sterile water for injection; ensuring not to pull away any skin that may be lifting prematurely
- Application of paraffin ointment to the lips
- Assessment of the tongue and oral mucosa’s moisture levels; may require a prescribed oral treatment (i.e. mucositis caused by chemotherapy)
- Assessment of the skin condition around the mouth in particular, pressure injuries caused by equipment (i.e. ETT, Replogle tube)
- Oral Immune Therapy with EBM is the provision of small amounts of EBM on a cotton bud (0.2mL split between each cheek) every 2 – 4 hours.
- Oral Immune Therapy with EBM is the provision of small amounts of EBM on a cotton bud (0.2mL split between each cheek) every 2 – 4 hours
- Oral Immune Therapy with EBM provides a level of immunoprotection, particularly in the extremely preterm neonate and empowers families in the care of the neonate.
Bathing
General Bathing Principles
Implement safety principles when bathing neonates
- Use standard precautions, including wearing gloves until after the neonates first bath
- Ensure bath equipment is not a source of cross contamination among neonates
- Implement environmental controls to create a neutral thermal environment and to minimise heat loss
- The choice of bathing technique depends on the neonates gestational age and clinical status
Swaddled-Immersion
- Recommended technique for neonates
- Benefits include a reduction of behavioural and physiological stress including temperature variation.
- The technique includes swaddling the neonate in a light swaddling cloth (i.e. muslin wrap or cloth nappy), submerging their body to the level of the shoulders, gently exposing each limb one at a time to wash and if distress is shown at any point, pausing and providing containment holding and/or nutritive sucking.
Sponge
bathing
- The least recommended technique as this method can result in haemodynamic compromise (i.e. heat loss) and behavioural distress. If sponge bathing is required, ensure the neonate is kept contained where possible to reduce behavioural distress, a warm environment is utilised (i.e. radiant
warmer or isolette) and physiological monitoring is continued.
First Bath (applies to all neonates, additional considerations for preterm neonates given below)
- Provide the first bath once the neonate has achieved cardiorespiratory and thermoregulatory stability
- Delaying the first bath to at least 6-24 hours after birth
is preferential
- For neonates born to a HIV-positive mother, the first bath should occur as soon as possible after birth
- Use warm tap water (temperature should be 37-37.5 °C) and a pH neutral or slightly acidic cleanser if required to assist with removal of blood and amniotic fluid
- Keep bath time short (approximately 5 minutes)
- Leave vernix intact as much as possible
- Use appropriate rewarming measures after bathing, including skin-skin contact
Routine Bathing
- Frequency of bathing and time of day should be based on individual need in consultation with the family
- Appropriate safety measures should be implemented
- Disinfect the bath before and after each use
- Maintain an adequately heated external environment, with an ideal room temperature of 21 – 24°C (close the doors to the room to minimise convective heat loss)
- Water should be deep enough to allow the neonates shoulders to be well covered
- A neutral or mildly acidic (pH 5.5 -7.0) cleanser (see suggestions below) may be used
- Cleansers should be free of potential irritants such as fragrance, alcohol, essential oils, botanicals and harsh detergents (eg. sodium lauryl sulfate)
- Neonates should be immediately covered with a towel and patted dry
- Ensure all skin folds are dried thoroughly (armpits, groin, neck and behind the ears)
- As per COCOON, encourage, support and involve parents in the bathing of their neonate
- An emollient may be applied for skin dryness (see section on emollient use for suggestions)
|
Preterm Infant Considerations
- Consider weight, gestational age and severity of illness when bathing preterm neonates
- For neonates less than 32 weeks gestation, consider the use or warm water only bathing during the first week of life due to skin irritation and risk with cleansers. Avoid rubbing.
- For neonates more than 32 week’s gestation, pH neutral or slightly acidic cleansers may be utilised. Neonates may be bathed every 2-3 days
- Use warm sterile water when areas of skin breakdown are evident
- If skin is dry, flaking or cracked after the bath, an emollient may be applied to the skin
|
|
Product Suggestions
Cleansing: QV Wash™, QV Gentle Cleanser™, Hamilton Skin Therapy Gentle ash™, Cetaphil Gentle Cleanser™, Avene Trixera Cleansing Gel™, Kenkay Body Wash™, Mustela Stelatopia Cream Cleanser™, CeraVe Hydrating Wash™, Dermeze Soap Free Wash™, Laroache Posay Lipikar
Syndet™
Emollients: As per Emollient box below |
Adhesives
A number of measures can be undertaken to ensure a reduced incidence of skin trauma with the use of adhesives in NICU
- Choose adhesives that cause the least trauma whilst still effectively securing medical devices
- Consider protecting the skin with silicone-based skin protective films
- Tape should be backed with cotton wool or tape
- Avoid removing adhesives until at least 24 hours after application
- Remove adhesives horizontally using warm water with soft paraffin
- Avoid using Solvents (Convacare™ wipes)
- If an adhesive remover is required, consider the use of a silicone based adhesive remover (ConvaTec Niltac)
ETT/NPT Strapping
- Use a silicone-based skin protective film (i.e. Comfeel™ or Duoderm™)
- Ensure tapes are cut to an appropriate size and mirror the size of the skin protective film
ECG Dots
- Consider if ECG dots are truly necessary; the neonate may be safely monitored using a saturation probe only.
- Exclusive use of hydrogel electrodes
- Assess electrode site regularly
- Replace electrodes every 7 days or after bathing
- Remove electrodes using the ‘horizontal method’, slowly and gently with a moistened gauze square
Transcutaneous Monitoring (TCM)
- Rotate between two sites every 2 – 4 hours
- Avoid having more than two TCM sites at any one time
- Decrease the TCM site temperature if redness at the site develops
Taping (Venous and Arterial Access)
Current best practice exists for the taping of venous and arterial lines, however the following are general considerations.
- Continual reinforcement of a CVAD dressing is not recommended as this leads to an increased risk of infection, skin breakdown and CVAD dislodgement
- Use Steri -Strips to strap around intravenous cannula
Intraoperative Eye Taping
- Silicone tapes are the preferred product for taping neonate eyelids intraoperatively
- If silicone tapes are unavailable, standard acrylate adhesive tapes are preferred (Micropore)
|
Preterm Neonate Considerations
Tegaderm and Leukoplast tapes are to be avoided in neonates less than 27 weeks (at minimum all leukoplast is to be ‘double backed’ or dabbed with cotton wool to reduce adherence to surface area. |
|
Product Examples:
Dressings: Comfeel, Duoderm, Transparent adhesive dressings (Tegaderm™), Hydrocolloids, Gel electrodes, Silicone based tapes (Siltape™, Mepitac™, 3M Kind Removal Silicone Tape™)
|
Disinfectants
Very little data is available on what disinfectants are best suited to the neonate skin, in particular preterm neonate skin.
- If a disinfectant is required in neonates less than 14 days of age and/or less than 30 weeks gestation, gently cleanse the skin with sterile water after the procedure.
|
Preterm Neonate Considerations
Chlorhexidine Gluconate aqueous solutions (0.1% Chlorhexidine Gluconate) are preferred in the preterm infant. The surrounding area should be cleansed thoroughly with a moistened gauze square after use. A number of studies have shown chemical burns in preterm infants where Povidone-Iodine and Isopropyl Alcohol were used, this should therefore be avoided.
|
|
Product Example
Disinfectants: 0.1% Chlorhexidine Gluconate, 0.5% Chlorhexidine in 70% isopropyl alcohol
|
Umbilical Cord Care
- Keep the cord area clean with water. Do not use alcohol wipes
- Cleanse with water and a pH neutral cleanser if soiled with urine or stool
- Fold the nappy down below the umbilicus
- Cord clamp may remain in situ until separation
- Where possible the umbilical stump should be kept exposed to air or loosely covered with clean clothing to avoid irritation and promote healing
- Avoid exposing the periumbilical skin to chemicals in order to prevent periumbilical burns
- Regular assessment is necessary to differentiate between normal umbilical cord healing and potential problems including infection
Emollients
Emollients restore lipid levels, improve hydration, preserve natural moisturising factors and offer significant buffering capacity to normalise skin pH and maintain skin microbiome.
- Apply an emollient top to toe daily at the first sign of dryness, fissures or flaking
- Maintain sterility by ordering patient specific containers or decanting products on to paper towel prior to application
- Emollient use is not associated with negative thermal effects or burns and may be used in conjunction with phototherapy or radiant heat
- Emollients should contain well- tolerated preservatives
- Emollient use may interfere with the use of adhesives
|
Preterm Neonate Considerations
Some evidence states that prophylactic emollient use in preterm neonates weighing 750 grams or less is associated with an increased risk of infection. Emollient use in this population should be weighed against the risk of infection and be in consultation with the Neonatologist.
|
|
Product Example
Emollients: QV Cream™, Cetaphil Cream™, CeraVe cream™ Kenkay Extra Relief Cream™, Mustela Stelatopia Moisturising Cream™, La Roache Posay Lipikar Baume AP™, Bioderma Atoderm Crème™, Dermeze Treatment Cream™, Hamilton Skin Therapy Cream™, Avene Xeracalm™
|
Common newborn rashes
Erythema Toxicum Neonatorum
A common condition affecting as many as half of all full term neonate neonates. Most prominent on day 2, although onset can be as late as two weeks of age. Often begins on the face and spreads to affect the trunk and limbs. Palms and soles are not usually affected.
Clinical features: Erythema Toxicum is evident as various combinations of erythematous macules (flat red patches), papules (small bumps) and pustules. The eruption typically lasts for several days however it is unusual for an individual lesion to persist for more than a day.
Treatment: The neonate is otherwise well and requires no treatment.

Figure 1. Erythema Toxicum Neonatorum (
http://www.huidziekten.nl/afbeeldingen/erythema-toxicum-neonatorum-2.jpg)
Neonatal Milia
Affects 40-50% of newborn babies. Few to numerous lesions.
Clinical features: Harmless cysts present as tiny pearly-white bumps just under the surface of the skin. Often seen on the nose, but may also arise inside the mouth on the mucosa (Epstein pearls) or palate (Bohn nodules) or more widely on scalp, face and upper trunk.
Treatment: Lesions will heal spontaneously within a few weeks of birth.

Figure 2. Neonatal Milia (
http://www.forestlanepediatrics.com/wp-content/uploads/2014/04/Milia.jpg)
Miliaria (Heat Rash)
Arises from occlusion of the sweat ducts. In neonates, lesions commonly appear on the neck, groins and armpits, but also on the face.
Clinical features: 1-3mm papules (vesicular or papular).
Treatment: Remove from heated humid environment or adjust incubator temperature. Cool bathing or apply cool compresses. Topical steroids may be used to facilitate relief while the condition resolves.

Figure 3 & 4 Miliaria (
http://www.leememorial.org/HealthInformation/graphics/images/en/2892.jpg)
Pityrosoprum Folliculitis
Neonatalacne or 'milk spots'. Affects babies within the first few weeks of life. Increased activity of the neonates' sebaceous glands cause inflammation and folliculitis.
Clinical features: Erythematous dome shaped papules and superficial pustules arise in crops, commonly affecting the cheeks, nose and forehead. This rash is not itchy.
Treatment: Will resolve within weeks without treatment or may be treated with ketoconazole shampoo (i.e. Sebizole shampoo) diluted 1:5 with water. Apply with a cotton bud twice a day. Rinse off with water after 10 minutes. Or apply Hydrozole cream bd to the affected areas until the rash has resolved.

Figure 5 & 6 Pityrosoprum Folliculitus (Images courtesy of of Dr David Orchard, Dermatologist RCH)
Links
Evidence Table
Evidence table for the
Neonatal and Infant Skincare guideline can be viewed here.
References
- Albahrani, Y. & Hunt, R. (2019). Newborn Skin Care. Pediatric Annals. 48 (1), 11-15
- Allwood, M. (2011). Skin care guidelines for infant’s 23-30 week ‘gestation: a review of the literature. Neonatal, Paediatric and Child Health Nursing, 14(1), 20-27.
- Association of Women’s Health, Obstetric and Neonatal Nurses (2018). Neonatal Skin Care (Forth Edition) – Evidence Based Clinical Practice Guideline.
- Blackburn, S. (2007). Maternal, Fetal & Neonatal Physiology: A clinical perspective. Missouri: Saunders Elsevier
- Blume-Peytavi, U., Lavender, T., Jenerowicz, D., Ryumina, I., Stalder, J., Torrelo, A. & Cork, M. (2016). Recommendations from a European Roundtable Meeting on Best Practice Healthy Neonate Skin Care. Pediatric Dematology. 33 (3). 311-321.
- Chalmers, J., Haines, R., Bradshaw, L., Montgomery, A., Thomas, K., Brown, S. et al. (2020). Daily emollient during infancy for prevention of eczema: the BEEP randomised controlled trial. The Lancet. Published online Feb 19, 2020.
- Clemison, J., & McGuire, W. (2016). Topical emollient for preventing infection in preterm infants (review). Cochrane Database of Systematic Reviews 2016, Issue 1. Art. No.: CD001150. DOI: 10.1002/14651858.CD001150.pub3.
- Expert Forum: Neonatal Skin Health and Skin Care Symposium 2015. www.researchreview.com.au
- Gregory, J., Anschau, N., McCutchan, D., Patterson, J., Martin, S., & Allwood, M. (2011). Skincare Guidelines for babies in NICU. Kaleidoscope, The Children’s health network.
- Horimukai, K., Morita, K., Masami, N., & Mai, K., et al. (2014). Application of moisturizer to neonates prevents development of atopic dermatitis. Journal Allergy and Clinical Immunology, 134, pp. 824.
- Lund, C., Nonato, L., Kuller, J., Frank, L., Cullander, C., & Durand. (2010) Disruption of barrier function in neonatal skin associated with adhesive removal. Journal of Pediatrics, 131 (3), pp. 367 – 372.
- New Zealand Dermatological Society (NZDS), http://dermnetnz.org/, May 2013
- Simpson, E., Chalmers, J., Hanifin J., & Thomas, K., et al. (2014). Emollient enhancement of the skin barrier from birth offers effective atopic dermatitis prevention. Journal Allergy and Clinical Immunology, 134, pp. 818 - 823.
- Skjerven, H., Rehbinder, E., Vettukattil, R., LeBlanc, M., Granum, B., Haugen, G., et al. (2020). Skin emollient and early complementary feeding to prevent infant atopic dermatitis (PreventADALL): a factoial, multicentre, cluster-randomised trial. The Lancet. Published online February 2020.
- The Royal Children’s Hospital. Clinical Practice Guidelines - Nappy Rash. Retrieved from: http://www.rch.org.au/clinicalguide/guideline_index/Nappy_Rash/
- The Royal Women’s Hospital (2016). Clinical Practice Guideline - Skin Care for Newborn Babies.
Varda, K., & Behnke, R. (2000). The effect of timing of initial bath on newborn’s temperature. Journal of Obstetric, Gynecologic & Neonatal Nursing, 27 (32).
Please remember to read the
disclaimer.
The development of this nursing guideline was coordinated by Robyn Kennedy, Nurse Practitioner, Dermatology and Alanah-Rae Crowle, Associate Nurse Unit Manager/CNS, Neonatal Intensive Care and and approved by the Nursing Clinical Effectiveness Committee. Updated May 2020.