Note: This guideline is currently under review.
Introduction
Aim
Definition of Terms
Background Information
Criteria for provision of thermoregulation assistance
Equipment
Assessment
Management
Documentation
Transfer to an open cot
Special Considerations
Companion Documents
Evidence Table
References
Introduction
The healthcare provider has a crucial role in preventing heat loss and providing a stable thermal environment for neonates and infants. The neutral thermal environment (NTE) has been defined as maintenance of the infants’ temperature with a stable metabolic state along with minimal oxygen and energy expenditure. The NTE is best achieved when infants can maintain a core temperature at rest between 36.5°C and 37.5°C. Thermoregulation is a vital body function, which is reflective of physiological maturity. Effective thermoregulation requires adequate energy stores (primarily glucose), insulation (fat deposits), hypothalamic function and muscle tone. It is widely supported that kangaroo mother care is the most effective method of regulating the neonatal temperature, however frequently in the critical care setting this is unable to be achieved. Furthermore, neonates and infants in the hospital setting frequently require a large portion of their body surface exposed for assessment and procedures which may lead to cold stress. Persistent cold stress is associated with increased morbidity and mortality; thus it is imperative to optimise thermoregulation. In order to ensure the neutral thermal environment is maintained in infants who are unable to achieve this with their own physiological measures, it is essential to provide environmental thermostability by blocking avenues of heat loss and applying adequate radiant warmth in a suitable cot.
Aim
To provide information to healthcare workers on the equipment available to apply assisted thermoregulation support to premature, neonatal and infant patients in the hospital setting, ensuring the most appropriate device is selected for patients will improve delivery of thermostability and optimise outcomes.
Definition of Terms
- Brown adipose tissue is a highly vascular type of fat around nape of neck, kidneys, between scapulae and axillas. Brown fat contains thermogenin, which is effective in generating heat during lipolysis by oxidation. This is activated when neonate’s temperature decreases below 36.5oC
- Cold stress is a cascade of physiological events caused by the infant’s use of chemically mediated thermogenesis in attempt to increase core temperature. Two specific alterations to thermogenesis occur in the infant suffering cold stress; vasoconstriction of the peripheries, which
allows heat to be drawn back to the core and metabolism of brown adipose tissue.
- Heat stress may also be incurred if an infant is exposed to high environmental temperatures, often associated with increased heart rate and decreasing stability. It is imperative to ensure frequent observation of probe placement when utilising a thermoregulatory device to
avoid a false-low reading if probe becomes detached, that will result in high heater output.
- HFJV: High frequency Jet ventilation, which is specialised for neonates, and requires a specialised circuit and JET ventilation box to be placed in close proximity to endotracheal tube. Requires easy access and close monitoring of neonate at all times.
- HFOV: High frequency oscillated ventilation, may be delivered by SLE ventilator or Sensormedics ventilator. Sensormedics circuit consists of large, immobile and rigid tubing, necessitating consideration in cot choice.
- Hybrid: A hybrid cot operates as an incubator, with the ability to raise the hood and function as an open-system radiant warmer. This cot is beneficial for premature infants who are best suited to being nursed in an incubator, where there is indication for frequent
access or surgery that necessitates an ability to provide open-system care. Surgery may be performed in the hybrid cot, however alternative thermoregulatory devices (cosytherm™ or bair hugger™) may be required, at the discretion of surgical team.
- Incubator: Incubators are utilised to provide a controlled, enclosed heated environment to ensure neutral thermoregulation is provided, enabling the infant to be nursed unwrapped. Incubators are the optimal choice for preterm infants requiring NTE support +/- environmental
humidification. Incubators support neurodevelopmental health for preterm babies, with reduction in noise and light within the enclosed environment. The incubator is not effective if frequent access to the baby is required for procedures or surgery, as temperature stability cannot be maintained with open
portholes or sides down. Can be operated in servo or environmental control settings.
- Open Care System: A thermoregulatory cot that is not enclosed, allowing easy access to the infant requiring frequent intervention as well as temperature support (e.g. Radiant warmer and Hybrid cots).
- Radiant warmer: Radiant warmers are an open care cot system designed to provide thermal stability to infants while allowing for continuous direct observation and accessibility. As this is not an enclosed system the temperature will fluctuate depending on the
surrounding environment. Delivery of humidification is very limited and unable to be accurately measured. Radiant warmers are most suitable for term neonates requiring NTE support, or for use during surgery and procedures on the unit. During surgery, alternative thermoregulation devices will be required, such as
the cosytherm™ mattress or bair hugger ™, at discretion of surgical team.
- Servo control: Heat output is automatically and constantly adjusted according to the programmed set skin temperature, which is continuously measured from the skin temperature probe. This is the preferred mode of applying thermoregulatory assistance to most neonates,
but requires close monitoring and assessment of probe site.
- Thermoregulation: The ability to regulate one’s core body temperature, even when environmental temperature is variable.
- Assisted thermoregulation is the application of controlled environmental temperature to maintain core body temperature within expected parameters.
Background Information
Modes of Heat Loss:
- Evaporation - Heat loss occurring during conversion of liquid to vapour
- Convection - Transfer of heat from the body surface to the surrounding air via air current
- Conduction - Transfer of heat from one solid object to another solid object in direct contact with it
- Radiation - Transfer of heat to cooler solid objects not in direct contact with the body
It is important to note that preterm infants are at a higher risk of heat loss via the 4 modes mentioned above. Preterm infants possess a disproportionate body mass-to-surface area ratio, reduced thermal insulation in decreased brown adipose tissue (BAT), a thin epidermis that has increased permeability, poor
vasomotor control and a naturally extended position that exposes a greater body surface area to the external environment. For these infants, cold stress will trigger a cascade of physiological responses that further impedes their transition to extrauterine life.
Criteria for provision of thermoregulation
assistance
- ≤ 32 weeks gestation OR ≤ 1800 grams
- Environmental humidity
- Surgery
- Moderate to high sedation therapies
- Muscle relaxation
- Phototherapy
- Prolonged procedure
- Observations requiring exposure of chest or abdomen
- Temperature instability for any reason
- Isolation for infection risk or additional precautions*
*Infants who have infection risk or require additional precautions may be nursed in an incubator to minimise environmental contamination in some instances. Incubators that are utilised for infection precautions only may not require the same thermoregulation principles as per
this guideline. Infants may be nursed in a low temperature environmental setting with light clothing and wraps.
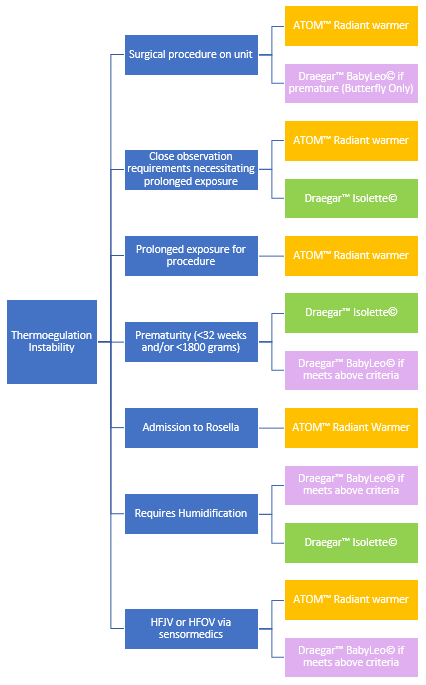
Equipment
- Isolette: The Draegar™ isolette is the incubator used at RCH. This is not suitable for neonates requiring HFJV or HFOV via the sensormedics due to limitations with space and inability to access the infant with ease in an emergency. Cares and
procedures should be completed through portholes where possible to minimise heat loss.
- Atom radiant warmer: The Atom™radiant warmers are available at RCH. The Atom is compatible with all modes of ventilation and other critical care equipment, and may also be used for short-term procedures in otherwise thermally stable infants. The atom cots
contain built-in scales to enable close monitoring of infant weight without removing from the bed.
See user tip-sheet.
- Babyleo® incuwarmer: The Draegar™ Babyleo® incuwarmer is the hybrid cot available on Butterfly unit, providing multiple functions to ensure optimised NTE, with ‘touch time’ mode increasing airflow to minimise alterations with open portholes during cares, and the ability to turn on the mattress heating to
ensure conductive heat is applied when necessary. Mattress setting should be set to desired core temperature for infant. Kangaroo mode is also available to provide continuous temperature monitoring of the infant whilst they are out of the cot for kangaroo cuddles. This reduces the need to disrupt family time, and
ensures the cot adjusts environmental temperature according to the infants needs prior to returning to the cot.
See user tip-sheet.
- Skin temperature probe: All devices have unique skin temperature probes. The ATOM™ skin temperature probes are reusable, and are fixated to the device. It is imperative that these probes are cleaned of adhesives to prevent organism
growth, and optimise monitoring function. The isolette and Babyleo® skin temperature probes are disposable. Heat reflective patches are required to adhere the probe firmly to the infant’s skin, with both hydrogel and foam patches available at RCH. Hydrogel patches are preferable in preterm infants
due to enhanced preservation of skin integrity.
When to choose which device
Assessment
Method of temperature assessment:
Rectal Temperature is taken on admission to Butterfly Unit to establish a baseline central temperature and patency of the anus. This should not be conducted as routine monitoring on other wards.
1. Place plastic sheath over thermometer
2. Dab a small amount of lubrication on end of thermometer
3. Insert thermometer 2cm into infant’s anus (1cm for preterm infant). Over-insertion may cause bowel perforation.
4. Turn thermometer on
5. Wait for 5 seconds post Celsius sign flashing
6. Remove thermometer
7. Clean with alcohol
Axilla Temperature is taken thereafter the initial rectal temperature.
1. Position the tip of the thermometer in the middle of the axilla
2. Lock the tip under the arm at a 35 - 45 degree angle in relation to the arm, using the arm to slightly apply pressure.
3. Turn thermometer on.
4. Wait 3 minutes for an accurate temperature reading.
5. Parents can be taught to safely take their baby’s temperature using the same process.
Frequency of Temperature Assessment:
Hourly until stable for 4 hours on:
- Admission
- Transfer to incubator, radiant warmer or open cot
- Commencement or cessation of phototherapy
- Commencement or cessation of humidity
- Commencement or cessation of servo control
When infant’s temperature is stable (for at least 4 hours prior):
- Hourly skin temperature documentation
- 3 - 4 hourly axillary for term infants
- 4 - 6 hourly axillary for preterm infants
Exceptions:
- 3 hourly for the first 24 hours when manual control is commenced, then 4-6 hourly
- Document heat output of device in servo control mode hourly, and check axailla temperature if there is a significant change in heating requirements.
- 3-4 hourly for all neonates in the first 24 hours when transferred to an open cot
- If temperature records outside normal range, commence hourly temperatures until 2 consecutive normothermic measurements (Refer to
temperature management nursing guideline)
- Infants on Neonatal Abstinence Syndrome (NAS) scoring charts require a temperature check a minimum
- 4 hourly or otherwise prior to each feed
Frequency of probe assessment:
- Visually inspect to ensure probe remains in complete contact with skin each hour, documenting site placement and skin temperature on EMR.
- When humidity is applied in incubator, more frequent checking of the site may be indicated as patch may become dislodged when moist. Closely monitor heat output and check site when there is a change in infant’s temperature or environmental temperature of ≥ 0.5°C.
Management
Probe placement: Optimal temperature probe placement for central surface monitoring is on the abdomen for a supine infant, ideally over the liver region; or on the back over the flanks if positioned prone.
The probe should NOT be placed on areas of brown adipose tissue (back, axillae, scapula, neck and kidneys) as brown fat metabolism is activated to generate heat during cold stress, delaying vasoconstriction at these sites, thus there will be a delay in detection of declining temperature stability. Additionally, bony prominences should be avoided due to reduced sensitivity to temperature changes.
It is imperative that the probe is not placed between the mattress and the infant, as this will create a false high reading, resulting in inadvertent cooling, and also poses a risk for pressure area development. The probe should be sited away from transcutaneous gas monitoring transducers. Ensure the probe is not in contact with any wound dressings.
It may be normal for a variance of skin probe temperature reading and axillary temperature of 0.5 – 1.0°C, and setting servo control should target appropriate skin temperature, not axillary temperature in the instance of a discrepancy.
The probe should be resited every 8 hours, or upon repositioning of the infant, with care taken when removing adhesive patch to minimise skin trauma. Skin adhesive remover (e.g. Niltac™) wipes may be utilised to aid with removal. Upon application it may take 4 - 5 minutes for temperature monitoring to stabilise.
Servo control is the preferred mode for all neonates and infants requiring assisted thermoregulation. Servo control maintains the infant’s temperature within a specific range by adjusting heat output to achieve pre-set skin probe temperature. This relies on appropriate placement of the skin probe, and continuous observation to ensure the probe remains well adhered to the skin and the heat output is not widely fluctuating. If there is a significant change in heat output from the device, closer assessment may be required to ensure probe remains well adhered. Increased thermoregulation requirements may be indicative of a deterioration and routine observations may need to be more frequent.
1. Infants weighing
<1750grams – Target axillary temperature of 36.8°C
2. Infants weighing >1750grams – Target axillary temperature of 36.5°C
Manual control is where a constant environmental temperature is set with continuous, unadjusted heat output. This mode may be used on all devices to pre-warm for an expected admission, when a temperature probe needs to be removed temporarily for a procedure, or when aiming to wean from an incubator to an open cot. This mode is not recommended for long-term use in other instances, as there is an increased risk of temperature instability in manual control. Air temperature must be set higher than ambient temperature of room. The temperature probe should remain insitu as a guide for nursing staff to monitor temperature continuously and adapt environmental temperature accordingly. Refer to environmental temperature for gestational age and weight chart.
Neutral Thermal Environment Chart
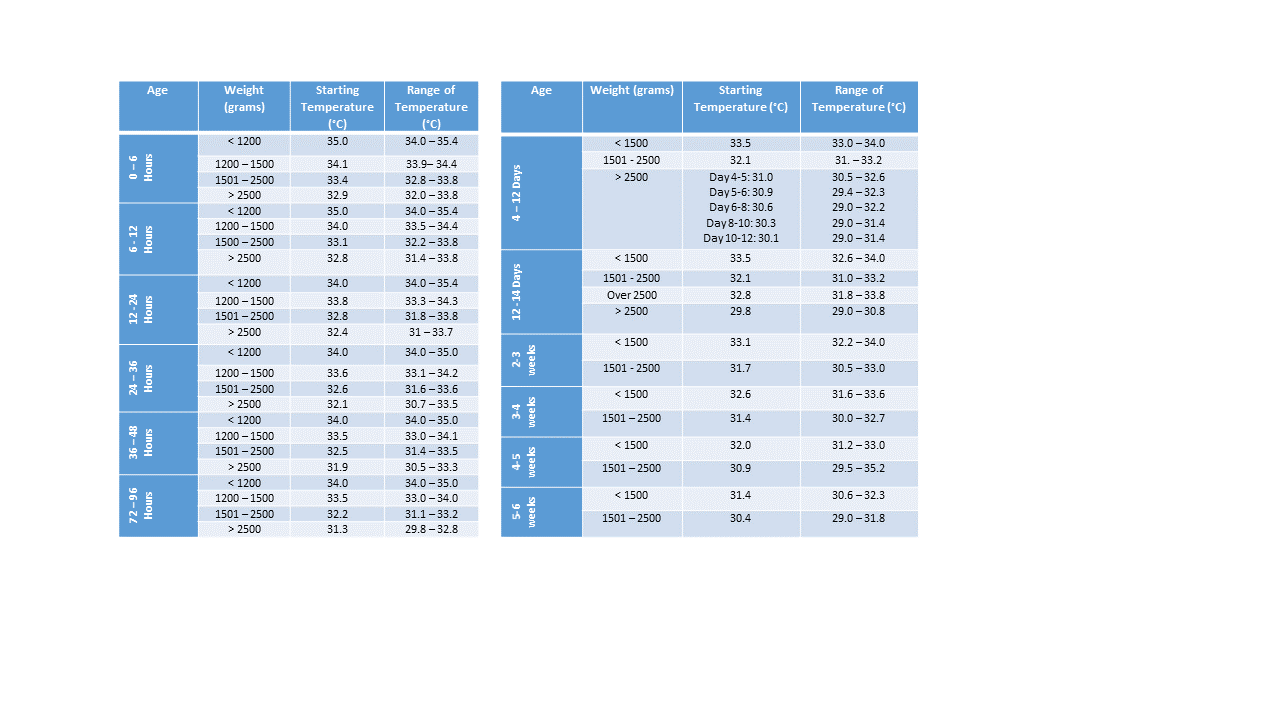
Generally speaking, the smaller infants in each group will require a temperature in the higher portion of the range, and for each age range, the younger infants generally require the higher temperature setting for the range.
Infants who do not fit the age and weight ranges for this chart should have the incubator set at 29°C with minimal clothing for observation as a starting point.
This data has been taken from GHS Neonatal Intensive Care
Unit Resident Handbook 2018-2019, adapted from Scopes JW, et al: Minimal rates
of oxygen consumption in sick and premature infants, Arch Dis Child 41: 407,
1966.
Temperature Outside
of Normothermic Range:
If the patient’s temperature is <36.5°C and not being actively cooled, initiate the following:
- Increase cot temperature by 0.5°C hourly
- Check axillary temperature hourly until 2 consecutive temperature of 36.5°C or above are recorded
- If the patient does not require close observation then layers (clothes & wraps) can be added but careful consideration needs to be given in blocking the transfer of heat and exacerbating the effects of conduction if the wraps/clothes are not pre-warmed.
If the patient’s temperature is >37.5°C, initiate the following:
- Assess environmental factors
- Assess physiological factors
- Decrease cot temperature by 0.5°C hourly
- Check axillary temperature hourly until 2 consecutive temperatures
<37.5°C.
- Consider whether this is an indication that the infant requires the set temperature to be weaned.
Considerations:
- Only ever alter incubator temperature by 0.5°C at any one time and allow at least one hour for the infant’s temperature to stabilise before making further changes
- Manipulation of incubator temperatures may obscure temperature instability associated with physiological features rather than environmental i.e. infection. This may put infants at risk of being nursed in inappropriately cold temperatures.
- NEVER switch the incubator off, as the fan does not work when the incubator is switched off. Once the incubator is switched off there is no circulation of air and therefore carbon monoxide levels increase. Please note that transfer of patients from room-to-room, out of the ward, etc. is an exemption to the
rule however, the duration in which the incubator is switched off needs to be minimised
- Inform AUM and/or Medical Team of any significant changes or concerns.
Documentation
Within the flowsheets of EMR, temperatures can be documented within the ‘observations’ section with the method of temperature selected from the drop-down options below. Furthermore, within ‘thermoregulation’, select either incubator or radiant warmer, and document the ‘skin temperature probe reading’, ‘skin temperature site’ and ‘set temperature/air temperature’ hourly.
Transfer to an open cot
Infants can be transferred to an open cot once they have met the following criteria:
- Weight ≥1800 grams
- Consistent weight gain
- Stabilized apnoeic and bradycardic episodes
- Medically stable condition
- No longer requiring invasive mechanical ventilation
- No longer requiring observations necessitating exposure of large surface area.
Once the infant meets the above criteria and discussion has taken place between the bedside nurse, medical team & AUM, the infant may be transferred to an open cot by using the following steps as a guide:
- If in an incubator, ensure thermo-control is set to air temperature mode and wean temperature by 0.5°C hourly (as a maximum) until the temperature is at the 26-27°C.
- Dress infant in pre-warmed clothing and wrap
- Ensure the infant maintains their temperature at this set temperature for 4 hours (hourly axilla temperatures)
- Place in open cot (preferably a Perspex cot)
- Assess temperature
- If the axillary temperature drops between 36.2°C and 36.5°C, increase clothing layers if possible and add a pre-warmed wrap/blanket.
- Check temperature hourly until stable for 4 consecutive hours
- If the axilla temperature remains unstable for a consecutive period of 3 hours (3 x hourly checks) then return the infant to a pre-warmed incubator.
- Infants nursed under a radiant warmer may be transferred to a normal cot when they are able to be dressed and wrapped appropriately, maintaining normothermia without heat output requirement.
Special Considerations
- Environmental humidity may also be applied to preterm infants in incubator and hybrid cots. See environmental humidity guideline.
- Infection control: The incubator and hybrid cots need to be changed every 7 days. If humidity is ceased, the cot should be changed immediately. In critical neonates who are deemed to unstable to move, the incubator may be utilised for up to 14 days, unless humidification has been used. The Babyleo® requires a comprehensive cleaning procedure if humidity has been in use. Please ensure the waterbag remains attached to the cot, and the laminated card in the drawer is placed on the mattress to ensure cleaning staff can easily identify the required process.
- Surgery on Unit will require application of thermoregulatory support under instruction and provision of surgical team. Whilst surgery may be conducted on the radiant warmer and hybrid beds, the heating output will need to be off, with the mattress of the Babyleo® disconnected. The cosytherm mattress is available on Butterfly, which may be appropriate during surgical procedures, and should be set to desired patient temperature. Alternatively, the surgical team may provide the bair hugger. This system consists of warming units and disposable blankets that distribute warm air across the patient before, during and/or after surgery.
- Palliative Care patients who require thermoregulatory support may be nursed on the cosytherm heated mattress in an open cot to enable families to access their baby more freely, and facilitate portability to ensure families can spend time away from the unit making memories whilst maintaining the comfort of their infant.
- Kangaroo care is beneficial for its neurodevelopmental and thermoregulatory properties and should be provided to neonates of all gestation unless there are contraindications, as outlined in
skin-to-skin care for the newborn nursing guideline.
Companion Documents
Evidence Table
The
evidence table for this guideline can be viewed here.
References
- Aydemir, O., Soysaldi, E., Kale, Y., Kavurt, S., Bas, A., Demirel, N. (2014). Body temperature changes of Newborns Under Fluorescent versus LED phototherapy: Authors’ reply. Indian Journal of Pediatrics, 81 (9), 990. DOI 10.1007/s12098-013-1279-1
- De La Fuente, L., Campbell, D., Rios, A., Graff, M., & Brion, L. (2006). Frequency analysis of air and skin temperature in neonates in servo-controlled incubators. Journal of perinatology, 26. 301-305.
- Engorn, B., Kahntroff, S., Frank, K., Singh, S., Harvey, H., Barkulis, C., Barnett, A., Olambiwonnu, O., Heitmiller, E., & Greenberg, R. (2016). Perioperative hypothermia in neonatal intensive care unit patients: effectiveness of a thermoregulation intervention and associated risk factor. Pediatric Anesthesia, 27,196 – 204. doi:10.1111/pan.13047
- Fellows, P. (2010) Management of thermal stability. Neonatal intensive care nursing, 2nd ed., pp 87 – 120.
- Greenspan, J., Cullen, A., Touch, S., Wolfson, M., Shaffer, T. (2001) Thermal Stability and Transition Studies with a Hybrid Warming Device for Neonates. Journal of perinatology, 21. 167 – 173.
- Handhayanti, L., Rustina, Y., Budiati, T. (2017). Differences in Temperature Changes in Premature Infants During Invasive Procedures in Incubators and Radiant Warmers. Comprehensive child and adolescent Nursing, 40 (1), 102 -106. doi.org/10.1080/24694193.2017.1386977
- Joseph, R., Derstine, S., & Killian, M. (2017). Ideal site for skin temperature probe placement in Infants in the NICU: A review of the literature. Advances in Neonatal Care, 17(2), 114-122. Doi: 10.1097/ANC.0000000000000369
- Martins, L., Silveira, S., Avila, I., Moraes., Silva dos Santos, D., Whitaker, M., & de Camargo, C. (2018). Thermoregulation protocol implementation for newborns in surgical procedures. Rev Gaúcha Enferm. 2019;40. doi: https://doi.org/10.1590/19831447.2019.20180218.
- Molgat-Seon, Y., Daboval, T., Chou, S., & Jay, O. (2013) Perinatal/Neonatal case presentation – Accidental overheating of a newborn under an infant radiant warmer: a lesson for future use. Journal of perinatology, 33, 738-739. doi:10.1038/jp.2013.32
- Molgat-Seon, Y., Daboval, T., Chou, S., & Jay, O. (2014) Assessing neonatal heat balance and physiological strain in newborn infants nursed under radiant warmers in intensive care with fentanyl sedation. European journal of applied physiology, 114. 2539 – 2549. Doi: 10.1007/s00421-014-2964-0
- Vilinsky, A., Sheridan, A. (2014). Hypothermia in the newborn: An exploration of its cause, effect and prevention. British Journal of Midwifery, 22. 557-562.
WHO recommendations on newborn health: guidelines approved by the WHO Guidelines Review Committee. Geneva: World Health Organization; 2017 (WHO/MCA/17.07). Licence: CC BY-NC-SA 3.0 IG
Please remember to read the
disclaimer.
The development of this nursing guideline was coordinated by Sarah Gardner, CSN/CNS, Butterfly Ward, and approved by the Nursing Clinical Effectiveness Committee. Updated June 2020.