Introduction
Delays in recognising neurovascular compromise can lead to permanent deficit, loss of limb and even death, therefore, assessment of neurovascular status is essential for the early recognition of neurovascular deterioration or compromise.
Aim
The aim of this clinical nursing guideline is to outline the required neurovascular assessment to recognise early compromise and prevent permanent damage to the limb(s).
Definition of Terms
- Active movement: Ability to voluntarily extend and flex an extremity or digit.
- Capillary refill: Is an assessment of arterial blood supply return. It is evaluated by firmly pressing on the nail bed of fingers or toes, briefly interrupting blood supply in the capillary system causing the nail bed to blanch, and timing how long it takes for the blood to return. Colour should return within 2-3 seconds once the pressure is released.
- Compartment Syndrome: An increase in pressure of a closed muscle compartment that causes muscle and nerve ischemia.
- Disproportionate pain: Pain that exceeds what is expected post injury or surgery, which is not relieved by analgesia.
- Fasciotomy: A surgical incision made through the fascia and into a muscle compartment due to increasing tissue pressures. The aim of this procedure is to release pressure to improve peripheral neurovascular status and prevent long term complications
- Muscle compartment: A well-defined space in the body that consists of a group of muscles, nerves and blood vessels in a particular segment. The muscle compartment is bound by fascia, a tissue that does not stretch or expand easily, and keeps the compartment in place. For example, the lower leg contains four muscle compartments.
- Musculoskeletal: Structurally includes a combination of muscles, bones, tendons, ligaments, joints and cartilage.
- Neurovascular: Is the structure and function of the vascular and nervous systems in combination.
- Passive movement: Assessors ability to extend and flex an extremity or digit.
Assessment
Criteria for neurovascular assessment
Patients who require neurovascular assessment include but are not limited to:
- Musculoskeletal trauma to the extremities
- Post-operative
- Internal or external fixation of fracture
- Orthopaedic surgery
- Spinal surgery
- Plastic surgery on extremities or phalanges
- Cardiac catheterisation
- Tourniquet applied for long periods
- Application of plaster cast
- Application of traction
- Burns patients
- Signs of infection in the limb
Frequency of observations
- 1 hourly for the first 24 hours post injury, surgery or application of cast.
- Then 4 hourly for a further 48 hours or as specified by the treating medical team.
- More frequently if any deviations from baseline observations. Frequency should be specified by the treating medical team.
For frequency
of observations for cardiac catheter patients please see the
Care of the Patient Post Cardiac Catheterisation Clinical Guideline.
Neurovascular assessment
A neurovascular assessment is required for each affected limb and includes assessment of:
Pain
The most important indicator of neurovascular compromise is pain disproportionate to the injury. Pain associated with Compartment Syndrome is generally constant, however, worse with passive movement to extension and is not relieved by opioid analgesia.
Indications of pain in non-verbal patients includes restlessness, grimacing, guarding, tachycardia, hypotension, tachypnoea and/or diaphoresis. If pain is disproportionate to injury, the medical team should be contacted immediately.
Please refer to the
Pain Assessment and Measurement Clinical Guideline for further information regarding paediatric pain assessment.
Sensation & Motor function
If neurovascular status is compromised, patients may report decreased sensation, loss of sensation, dysesthesia, numbness, tingling, or pins and needles. Altered sensation may be a result of a nerve block or epidural. If this is the case, this should be documented in the patient’s neurovascular assessment in
flowsheets in EMR.
When assessing motor function, the amount of pain on movement in the affected limb should be noted, including if it was pain on active or passive movement. It is imperative to compare movement of digits bilaterally and to baseline observations, as some
patients may have had limited or no movement previous to injury.
Refer to the table below for how to assess sensation and motor function for each nerve in the hands and feet.
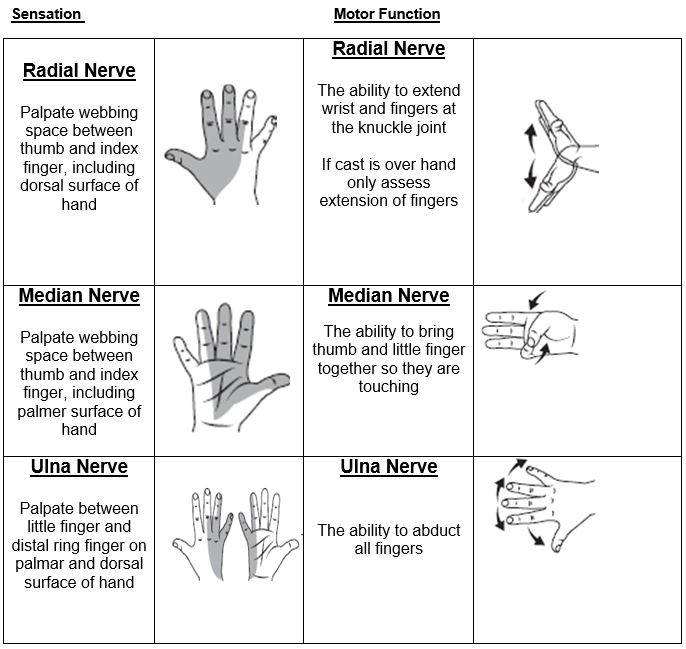
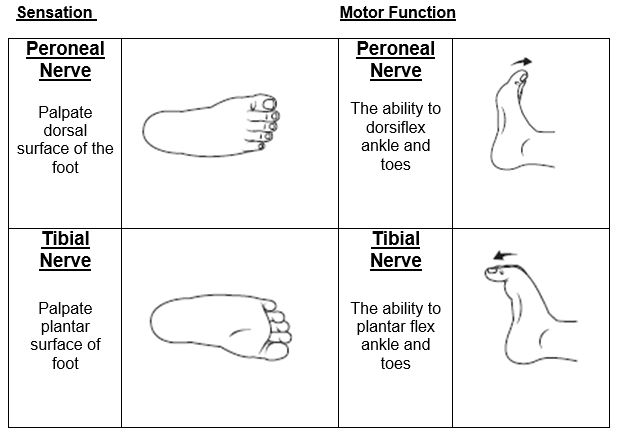
Images created by RCH.
Perfusion
Colour, temperature, capillary refill, swelling and pulses should be assessed when completing a neurovascular assessment. Neurovascular compromise can result in inadequate arterial supply (reduced blood flow from the arteries to the periphery of the affected limb) or inadequate venous return (reduced blood flow
from the periphery of the affected limb to the heart), resulting in changes in these parameters.
Please refer to the table below to identify indicators of normal perfusion, inadequate arterial supply, and inadequate venous return. Changes in perfusion should be escalated to the medical team immediately.

Documentation
A baseline neurovascular assessment of both limbs is essential in recognising neurovascular compromise. Neurovascular observations for both upper and lower limbs can be added into flowsheets in EMR for documentation via the orders tab.
Alterations in neurovascular status should be documented in flowsheets and the medical team should be notified immediately. Photographs can be taken with consent from the carers and/or patient (pending age) and saved in the media file in EMR, to document any changes in neurovascular status and allows medical teams to view
progress. See Clinical Images
Policy.
Management
If neurovascular compromise or deterioration is suspected, complete the below dot points whilst waiting for an urgent review from the medical team.
Management of Neurovascular Compromise
- Elevate limb, no higher than heart level. Lower extremities can be elevated with pillows or using bed mechanics. Upper limbs can be elevated on either a pillow, sling or box sling.
- Split plaster casts with treating teams approval or cut/remove bandages.
- Maintain limb alignment.
- Increase frequency of neurovascular observations (frequency to be decided by treating team).
- Notify treating team immediately.
If neurovascular status improves keep affected limb elevated and continue to monitor closely.
If neurovascular status does not improve or continues to deteriorate, the patient may need to attend theatres for pressure monitoring and/or fasciotomy.
For cardiac catheter patients:
If any changes in neurovascular observations (i.e. decreased in pulse pressures, changes in limb colour or colour of limb) are identified, findings should be escalated to the treating team or Catheterisation Fellow. Consider need for an ultrasound to
confirm or rule out a thrombus.
See Care of the patient post cardiac catheterisation guideline.
Compartment syndrome
Compartment Syndrome is a serious complication of musculoskeletal injury. Patients at high risk of Compartment Syndrome include open fractures, high-energy trauma, concurrent humerus and forearm fractures, crush injuries, and application of tight bandages and/or casts. Compartment Syndrome results from an increase in
pressure inside a compartment which comprises of muscle and nerves and is enclosed by facia. Fascia is inelastic and does not expand to increase volume or pressure. When the compartment pressure increases, nerves and muscles become compressed, resulting in decreased blood flow and tissue perfusion, muscle and
nerve ischemia, and loss or altered sensation, therefore, early detection and intervention is essential.
Compartment Syndrome is a surgical emergency. To relieve the pressure or reduce volume within the compartment, a surgical incision, known as a fasciotomy, is made through the fascia and into the affected muscle compartment. This will preserve blood flow to ischemic
muscle and nerves, thereby preventing long term neuromuscular complications such a muscle fibrosis, atrophy, contractures and deformities.
Indications of Compartment Syndrome include ‘the 5 Ps’ as listed below:
- Pain: Pain out of proportion to injury, extreme pain on passive movement and pain unrelieved with opioid analgesia, is the first and most reliable sign of Compartment Syndrome.
- Paraesthesia:
Results from nerve compression and generally is indicated by pins and needles, tingling or numbness.
- Pallor: Indicates arterial insufficiency below the level of injury. Below the level of injury will feel cold to touch and appear pale.
- Paralysis:
Is generally a late sign of compartment syndrome and results from prolonged nerve compression or muscle damage. Paralysis presents with inability to actively move the limb and increase pain on passive movement that is not relieved in extension.
- Pulseless:
Absent pulse is a late sign and indicates tissue death.
Additional indications of Compartment Syndrome include:
- Temperature:
Coolness of the limb distal to injury indicates decrease arterial supply.
- Capillary
Refill: Indicates limb perfusion. Capillary refill more than 3 seconds indicated inadequate limb perfusion.
- Swelling
and Increased Pressure: As a result of increased inter-compartment pressure, skin presents tight and shiny.
If Compartment Syndrome is suspected, the medical team should be contacted immediately for a review.
Discharge and Carer Information
During patient’s admission, carers and patients should be educated on the importance of performing neurovascular assessments and why it is necessary to continue to monitor even when the patient is sleeping.
Many patients who are at risk of neurovascular compromise leave hospital before the risk of Compartment Syndrome is over, therefore, discharge education on neurovascular assessment is crucial. Carers should be educated regarding the signs and symptoms of
neurovascular compromise, and when to return to their GP or RCH if they are concerned. Additionally, age-appropriate education should be provided to the patient, including encouragement for the patient to move their digits regularly.
For cardiac
catheter patients:
See Care of the patient post cardiac catheterisation guideline.
Links
- Nursing Guidelines
- Kids Health Information
Evidence Table
Click
here to view the Evidence Table for this guideline.
Please remember to read the
disclaimer.
The revision of this nursing guideline was coordinated by Hannah Harper, CNS, Platypus Ward, and approved by the Nursing Clinical Effectiveness Committee. Updated February 2023.