Introduction
Regional anaesthesia (RA) or neuraxial analgesia is the administration of local anaesthetic (LA) into the epidural space through an indwelling catheter. Epidural analgesia has shown to provide better pain relief than parenteral opioids. Children can experience
moderate to severe pain post-operatively and it is likely to be worse in the first 24-72 hours.
Uncontrolled pain can cause stress responses that are detrimental to recovery. RA provides excellent analgesia and reduces surgical stress response while decreasing the need for opioids. RA epidural is used for moderate to severe pain.
The insertion of the epidural catheter will be determined by the type and site of surgery. This will enable the LA effect to block the nerve impulses associated with the area of spinal nerves innervating the surgical site and giving the best post-operative analgesia.
It is important to communicate and educate families and children about the expectation and sensations of the epidural and why it is important to assess and monitor observations.
It is important to understand and identify epidural complications to ensure the safety of the patient and provide effective analgesia.
Children and young people who have epidural analgesia require suitably trained nursing staff to care for them to minimise side effects and complications and ensure analgesia is optimal.
Aim
To provide guidance on safe care of children and young people with an epidural and consideration of potential complications.
Definition of Terms
- Central block: Central neuraxial block (spinal, epidural and caudal).
- Dermatome: A dermatome is an area of skin innervated by a single spinal nerve. At each vertebra nerve roots exit bilaterally.
- Epidural Space: Found Between ligamentum flavum and the dura mater, it extends from the foramen magnum to the coccyx. Contains fat, blood and connective tissue.
- Local
anaesthetic (LA): A drug that reversibly blocks the transmission of pain along nerve fibers. LA can block transmission in autonomic, sensory and motor fibers.
- Sensory nerve: Sensory nerves respond to pain, temperature, touch and pressure. Pain and temperature nerve fibres are affected by LA.
- OILS check: following a standardised procedure for pump programming and checking of infusions. Orders, Infusions, Lines and Securement (OILS).
Indications
Epidurals are used post major surgery to provide excellent analgesia to a discrete area of the body by blocking the sensory nerves with minimal side effects. Epidurals can minimise the opioid requirements and optimise rest and recovery in the post–operative period.
The epidural infusion may be prescribed for children and young people who:
- who may be sensitive to side effects of opioids
- Are assessed to be at risk of respiratory suppression in the setting of IV, IM or oral opioids
Have cerebral palsy and experience high muscle tone and are undergoing orthopaedic surgery.
Assessment and Management
Post
Anesthetic Care Unit (PACU)
The initial assessment of a child with an epidural in the PACU includes:
- baseline observations
- Pain assessment
- Assessment of the effectiveness of the epidural including:
(Information about dermatome distribution and assessment of sensory block and assessment of motor block is located at the end of this guideline)
The sensory block and motor block should be documented in the Flowsheets in EMR, noting the motor block may be dense due to the possible higher concentration of LA given intra operatively.
Any issues with sensory or motor block identified by the PACU nurse should be escalated to the treating anaesthetist and/or the In-charge anaesthetist. These issues should be communicated to the Children’s Pain Management Service (CPMS) team prior to
patient transfer from PACU.
All general post-operative observations, fluids and medications should be checked and documented at this time.
Epidural
assessment
Checking of the epidural infusion should be incorporated into OILs check at handover times see Standardised checking procedure for infusion pump programming at the RCH.
The sensory block (dermatomes) should be assessed 4 hourly and at the following times:
- In PACU after rousing from the anaesthetic, and immediately after patient initial bolus dose,
- On return to the ward,
- If the patient complains of pain,
- One hour after a bolus or rate change.
The motor block (bromage) should be assessed 4 hourly and at the following times
- In PACU after waking from the anaesthetic,
- On return to the ward,
- Prior to ambulation if required,
- One hour after a bolus or rate change.
The catheter insertion site should be checked at least 8 hourly for any redness, tenderness or leaking. If visible the catheter markings should be checked to make sure there has been no movement of the epidural catheter. The dressing should be checked and reinforced if any tape is lifting.
The epidural infusion would be expected to last for 3 - 4 days unless there are adverse events.
All patients who have an epidural in situ must have a working intravenous (IV) to allow access for management of any adverse events.
Clinical
observations
Clinical observations are to continue until the epidural has ceased including hourly sedation, heart rate, respiratory rate, pain score (while awake).
Blood pressure and temperature are to be assessed at least 4 hourly until the epidural has ceased.
Please see the
Nursing Assessment Guideline and/or the
observation and continuous monitoring guidelines for more information.
Pressure
injury care
The decreased sensation and movement caused by the epidural analgesia may cause nerve compression and pressure areas.
Children/young persons who require epidural anaesthesia are at increased risk for pressure acquired injury. All children/young persons who have an epidural therefore need to be assessed for an individual prevention plan based on the Glamorgan Pressure Injury Risk Assessment Tool. For more information see the
pressure injury prevention and management nursing guideline.
Pressure care should be strictly observed at a minimum of 4 hourly, or more frequently as required, to susceptible areas such as heels, lateral malleoli and sacrum. Pressure mattresses, and pressure supports should be used to reduce risk and documented
in the primary assessment flowsheet. See the
pressure injury prevention and management guideline for more information.
Adverse events
The following adverse events or concerns about the epidural or patient should be urgently reported to the Children’s Pain Management Service (CPMS) urgently – page 5773
- Clinical observations outside the parameters for age should be reported to CPMS.
- A fever 38.5 degrees
- Any changes or increase in pain
- Any changes in the sensory block becoming high above T3 (for example breathing difficulties).
- No block or inadequate block/unable to relieve pain
More information regarding epidural
complications can be found below.
Special considerations
NICU
Neonates rarely have epidural analgesia but the main difference is a lower concentration of LA and/or a lower hourly rate and the expected duration of infusion is less at 36 hours.
Lumbar
epidurals
Children and young people who have lower limb surgery will have a lumber epidural and as this area innervates the urinary bladder it is important for the child/young person to have an indwelling urinary catheter inserted while in theatre. The urinary
catheter will need to stay in until the epidural infusion has ceased.
Management
of complications/troubleshooting
Report to CPMS Pge 5773 urgently if
- Any major change in motor function,
- Almost complete or complete motor block in legs,
- Reduced motor function in hands or fingers (with a thoracic epidural),
- CPMS must be notified if the patients’ vascular access IV has dislodged or needs replacing.
There are three types of complications associated with epidurals: complications related to epidural catheter insertion, complications related to epidural drugs, complications related to pain.
Complications related to epidural catheter insertion
Headache (post dural puncture headache)
- If the epidural needle has inadvertently penetrated the dura and there is a CSF leak the patient may experience a low- pressure headache. This may not be evident until the patient mobilises. This is of a very low incidence and most cases will improve spontaneously.
- Conservative treatment is rest, fluids, analgesia and rarely a blood patch (autologous blood inserted into the epidural space). Requiring an anaesthetic procedure.
Back pain
- This is usually at the insertion site; it is common and transient.
- Moderate to severe back pain must be reported to CPMS urgently for investigation.
- Epidural abscess - this is very rare.
- Epidural haematoma - this is very rare and will require urgent investigation.
Both abscess and haematoma will present with moderate to severe back pain and sensory and motor deficits
Complications related to epidural drugs
Overdose/toxicity
- Signs of LA toxicity are dizziness, blurred vision, decreased hearing, restlessness, tremor, hypotension, bradycardia, arrhythmia, seizures, and sudden loss of consciousness.
- Cease the RA infusion.
- May require resuscitation and management of cardiac, neurological and respiratory side effects.
Complications
related to pain
Pain escalation
- Assess dermatomes, if there has been a receding block an epidural bolus may be required and the infusion rate may need to be increased.
- The first line analgesia is an epidural bolus before administration of other analgesia.
- Check if the epidural catheter become disconnected, if the epidural catheter been dislodged, or if the epidural infusion is leaking.
Removal of the epidural
At the same time the epidural infusion has ceased it is important to give other prescribed analgesia to ensure pain management is optimised as the LA wears off over the next 4-6 hours.
Speak to CPMS and Medical team if patient is on heparin, prior to removal of epidural.
Removal of the epidural catheter is performed using
standard aseptic technique
- Explain the removal technique to the patient and carer with age-appropriate language.
- Have the patient sitting up and bending gently forward or lying on their side supported and comfortable.
- After turning the epidural infusion off, remove tape, holding the epidural catheter at the site of insertion at the skin gently pull with a steady pressure. If there is any difficulty in removing the catheter stop and call CPMS Page 5773.
- After removal assess the insertion site, ensure tip of catheter is intact. Document the level the epidural catheter was inserted at (cm at the skin).
- The exit site does not require a dressing, however the site needs to be checked in the next 12-24 hours for any abnormality such as infection or haematoma.
- After the removal of epidural analgesia, IV or/and oral analgesia will be needed as regular and PRN to ensure the patient is able to continue recovery.
Education
All families are given an epidural information card from CPMS outlining any issues to be concerned about once they have gone home.
A contact telephone number for RCH and CPMS is provided for the family if they have any ongoing concerns.
Dermatome
distribution, assessment of sensory block and assessment of motor block
Dermatome distribution (Dermi Boy RCH)
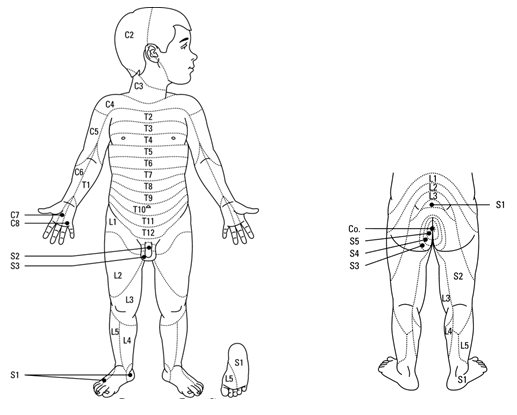
Assessing
Sensory Block
If the patient is able to
understand and report
- Explain the procedure to the patient and family.
- Wrap an ice cube in tissue or paper towel leaving an area exposed.
- Place the ice on an area well away from the dermatomes and ask how cold does this feel.
- Apply the ice to an area expected to be numb and ask if it feels the same, for example as cold as your face or different?
- Apply the ice above and below this area, until you determine the upper and lower dermatomes blocked.
- Assess one side of the body then the other to see if the block is unilateral or bilateral.
If the
patient is unable to understand or report due to age or cognition, an assessment should still be performed and documented.
Patients may report the ice feels warm, the same or colder.
- While assessing the epidural block, observe for any change in facial expression as the ice is applied, muscle flinching or pushing away.
- Gentle palpation over the surgical site can also give an impression of comfort if the epidural is effective or pain if the epidural is not effective.
Assessing
Motor Block
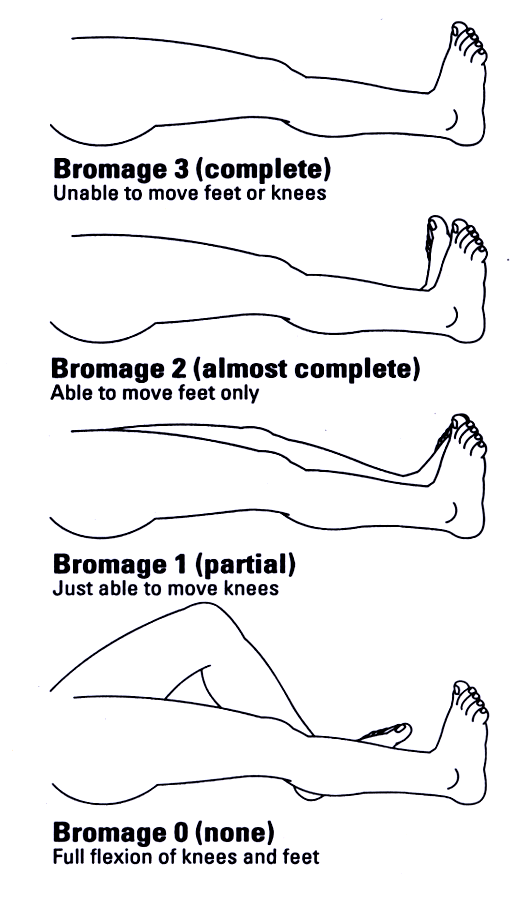
Motor nerves as well as sensory nerves may be affected by LA.
It is important to assess motor block:
- To prevent pressure areas,
- To assess safety for standing/walking if allowed,
- To detect complications e.g. epidural haematoma, or abscess.
Procedure
when assessing motor block
- Explain procedure to patient and family.
- Ask the patient to flex their ankles and knees.
- Document the score in the clinical observation chart.
There may be a difference between legs. Assess if the patient is able to move their feet or knees prior to the epidural e.g. some children with neuromuscular impairment may not be able to voluntary move and poor pro-perception can also make it difficult.
Links
Evidence Table
You can view the
evidence table for this nursing guideline here.
Please remember to read the
disclaimer.
The development of this nursing guideline was coordinated by Sueann Penrose, Registered Nurse, Anaesthesia & Pain Management, and approved by the Nursing Clinical Effectiveness Committee. Revised August 2023.