Note: This guideline is currently under review.
Introduction
Asthma is a respiratory problem that affects one in nine children in Australia, and is the most common reason children visit hospitals. At the Royal Children’s Hospital (RCH) it is one of the leading causes of presentation to the Emergency Department. Providing appropriate education and self-management skills to these families will help to decrease the number of asthma presentations to the hospital.
Aim
The aims of this guideline are:
- To ensure all patients with asthma and their families at RCH receive consistent, timely and current asthma education before discharge
- To adequately prepare patients and their families for discharge
- To provide an education framework for nurses caring for patients with asthma and ensure excellence in care is being delivered
Definition of terms
- NESB: Non-English speaking background
- Metered dose inhaler (MDI): Device that delivers a specific amount of medication into the lungs, in a short burst of aerosolised medicine (sometimes referred to as a ‘puffer’)
- Puff: A puff refers to the delivery of one spray of medication from the MDI
- WAAP: A Written Asthma Action Plan is a tool that outlines the asthma management required on a day-to-day basis and provides instructions on what to do when the patient becomes unwell
- 4x4x4 rule: Nationally recognised ‘First aid for asthma’. Give 4 puffs of Ventolin, take 4 breaths after each puff, wait 4 minutes, and if no improvement, keep giving 4 puffs every 4 minutes until ambulance arrives
Assessment
- Patients admitted to RCH with a diagnosis of asthma or viral associated wheeze
- Patients assessed as ready to be discharged
- The family’s social situation, health literacy and cultural needs should be considered. This may include:
- NESB, access to services, parent/carer health etc.
- Education needs (patient and parent/carer)
Management
For acute asthma management please refer to RCH CPG - Asthma acute
Asthma education is the responsibility of all nurses from all departments at RCH. It is important the information provided is consistent. Education should be commenced as soon as practicable following admission to allow for timely discharge. Ongoing management and support post discharge should also be considered via the Complex Asthma Service or Community Asthma Program (please see Discharge Planning later in the guideline).
Education topics and resources
Patients and parents/carers should be presented education in several formats:
Important factors to cover are:
- What is asthma?
- Triggers
- Signs and symptoms
- Treatment/management
- When to seek medical review, using the WAAP
It is important to ensure patients and parents/carers have an understanding of every medication prescribed, including Salbutamol, and if applicable Prednisolone and Preventers. It is important that they understand:
- Why medication/s have been prescribed
- The action of the medication/s
- How long they need to take medication/s for
- Side effects
- Storage requirements
- Checking of expiry dates and if the medication canister is empty. Advise
parent/carer to check the counter on all puffers, where applicable, to monitor
usage.
Spacers
A spacer device should be used for children of all ages, including adolescents, whenever they use a MDI. Ensure the patient and parents/carers are able to demonstrate correct technique when using the MDI and spacer (including correct placement of mask and shaking MDI between each puff), and that they understand the appropriate cleaning and storage requirements.
Provide and explain the Kids Health Info: Asthma - use of spacers fact sheet
Refer families to Kids Health Info: Asthma – videos for demonstration of spacer technique
Written Asthma Action Plan (WAAP)
Provide the patient and parents/carers with a WAAP and go step by step through the plan, ensuring they understand what is written, and highlighting when to present to their GP or hospital (i.e. needing reliever more frequently than 3 hourly). Families need to be aware of the importance of following this plan when their child/adolescent has asthma symptoms. The WAAP must only be completed by medical staff.
Ensure that the patient and parents/carers understand their Asthma Emergency First Aid requirements - i.e. 4x4x4 rule (as documented under ‘Danger Signs and Critical Asthma First Aid’ section of the WAAP).
Advise parents to give Salbutamol for asthma symptoms only as required. Written plans for weaning of Salbutamol are not recommended.
Smoking cessation
It is important to highlight to families the adverse effects of cigarette smoke exposure on children/adolescents with asthma. If you are not comfortable with talking to parents about this subject, your AUM/senior RN could be of assistance.
If support is required in relation to quitting you can refer patients/parents/carers to Quit or their local GP.
Documentation
All patients admitted to RCH with asthma should have the appropriate ‘Inpatient Asthma Education’ elements added to their Education record in EPIC, if these have not been previously added. It is then the responsibility of the RN on each shift to document the patient’s and parent/carer’s progress in relation to this education. For each new admission, the status of the patient’s and parent/carer’s education should be reviewed to ensure that they maintain a good understanding of all the education elements.
Discharge Planning and Follow-up/ Review
All patients with asthma should have a clear follow up plan on discharge. This may include:
- A follow-up appointment scheduled with GP, Outpatient Department or Paediatrician/Respiratory Consultant
- A Complex Asthma Servicereferral for eligible patients (medical referral required) (see Complex Care)
- A Community Asthma Program (cohealth or DPVHealth) referral (nursing or medical referrals accepted) if the family require further education and support
- Advise family to seek an urgent GP review in the days following discharge if their condition deteriorates, or fails to improve significantly within 48 hours
- Encourage families to keep an asthma diary to monitor Salbutamol use
Special Considerations
- Anaphylaxis – Asthma increases the risk of fatal anaphylaxis. Close monitoring of asthma and allergy follow-up is essential
- Allergic rhinitis – Control in spring should be reviewed and managed by the child’s GP/Paediatrician (advice should also be given for thunderstorm asthma events)
- NESB – Alternative education resources are essential for these families:
Discharge checklist
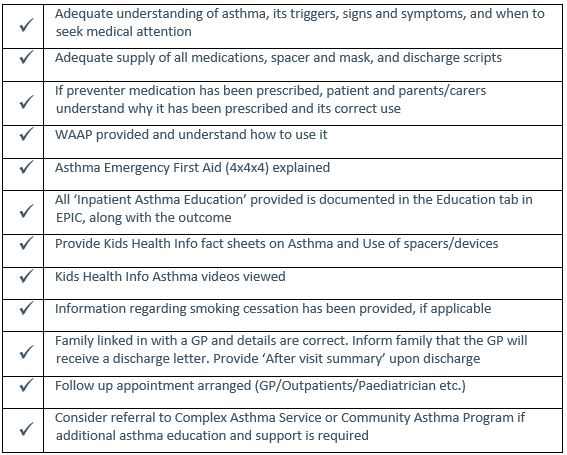
4 Key Points for parents/carersSigns/symptoms – Able to identify asthma signs and symptoms, including what is normal for their child, so they can better appreciate the signs when their child is unwell Puffs (medication) – Know how much Salbutamol to give their child (6 puffs <6yrs, 12 puffs >6yrs), and understand their child’s preventer medication and adherence strategies Spacer technique – Able to demonstrate correct spacer technique
Plan – Know when to attend GP, hospital or call 000 (as per WAAP) |
Companion documents
Links
Evidence table
The evidence table for this guideline can be viewed here.
Please remember to read the disclaimer.
This nursing guideline was updated by Katie Rogers and Adele Berry, CNC’s - Complex Asthma Service, and approved by the Nursing Clinical Effectiveness Committee. Updated November 2021.