Introduction
Aim
Definition of Terms
Maintaining a safe environment for all patients
Educating families and carers
Risk assessment
Management
Considerations for discahrge
Companion documents
Links
Evidence table
Introduction
Falls are the most common cause of paediatric injury leading to emergency department visits. It is widely acknowledged that children are at risk of falls, with many education programs supporting prevention, it is important that this education is reflected in the hospital environment. Children fall as they grow, develop coordination and new skills; often unaware of their limitations. RCH incident data suggest those at the highest risk of falls are those in the toddler age group (1-2 years) and the adolescent group (10-17 years).
Aim
The intention of this guideline is to raise awareness and educate nursing staff and the multidisciplinary team of the importance of maintaining a safe environment for all patients; assist with identifying patients who are at high risk of falls; provide the tools to educate families and carers of the potential risk of falls and outline strategies to develop management plans of care to reduce risk for high risk patients.
Definition of Terms
Fall - A fall is an event which
results in a person coming to rest inadvertently on the ground or floor or
other lower level.
Anticipated falls - may occur when a patient whose
score on a falls risk tool indicates she or he is at risk of falls.
Unanticipated falls - occur when the cause of the
fall is not reflected in the patient's risk factor for falls, conditions exist
which cause the fall, yet these are not predictable (e.g., the patient faints
suddenly).
Near miss fall – when a fall was likely but did
not occur, but was averted due to action by patient, carers or staff.
Accidental falls - occur when a patient falls
unintentionally, usually as a result of tripping or slipping, as a result of
equipment failure or other environmental factors. Patients cannot be identified
as being at risk for falls prior to this type of fall.
Risk assessment tool - a conceptual framework that
organises knowledge on the aetiology of predicting falls.
Maintaining a safe environment for all patients
All paediatric patients are considered at risk of falling and simple prevention strategies should be put in place to ensure the risk of injury is minimized. A safe environment should be maintained for all patients within the Royal Children's Hospital (RCH). Standard safety measures should be put in place for all patients regardless of identified risk, these include:
-
Orientate all patients, parents/carers to
room and ward
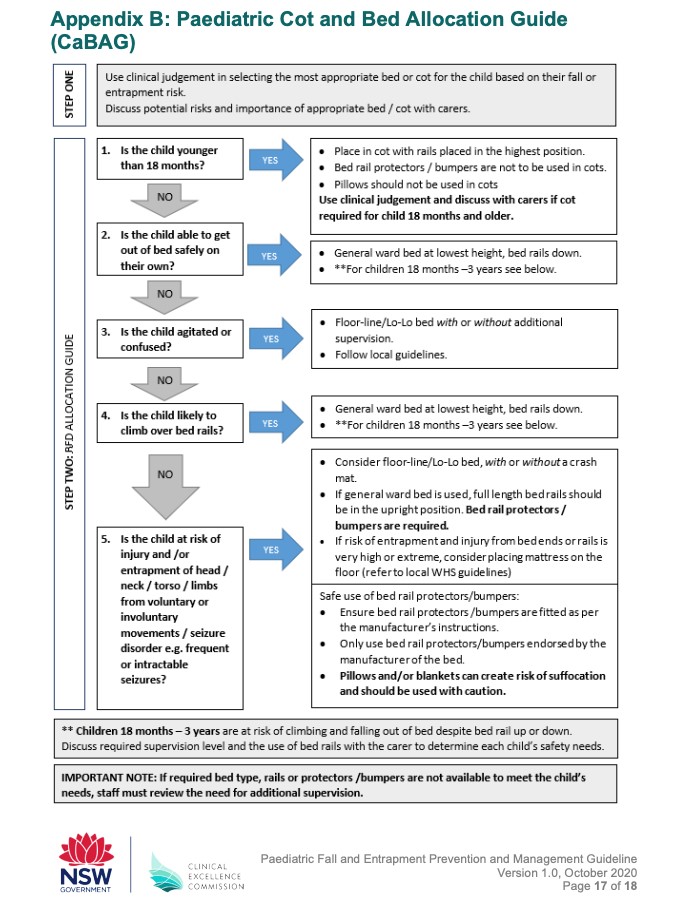
- The Choice of nursing a patient in a bed or
cot is a clinical decision based on what is appropriate for the patients
age and development and based on their fall or entrapment risk. This can
be assessed by following the flow chart; Appendix B: Paediatric Cot and
Bed Allocation Guide (CaBAG). Usually children under
18 months should be nursed in a cot although each child needs to be
individually assessed.
- The use of side rails and cot sides is also
an individual assessment and can also be guided by the flow chart CaBAG.
- Keep beds in low position with brakes on and
bed ends in place
- Appropriate non slip footwear for ambulating
patients
- Nurse call within reach, educate patients and
families on its functionality
- Maintain adequate lighting in child's room;
low level lighting at night.
- Keep floors clear of clutter including
equipment and toys
- Secure and supervise all children with a
safety belt or harness in wheelchairs, highchairs, strollers, infant
seats and any specialist seating (e.g. Tumbleforms)
- Children on trolleys are always under the
immediate and direct supervision of a staff member or a caregiver
- Infants in an incubator have portholes
securely fastened and door closed unless directly attended
- Hourly rounding will support the provision of
proactive care such as the need for assistance to the bathroom
- Assist unsteady patients with ambulation;
refer to physiotherapy notes where available
- Place necessary items a patient may need
within reach (drinking water, phone, etc)
- Patients who have received sedation or
general anaesthetic may be unsteady and require supervision
- Ensure appropriate equipment is available,
well maintained and serviced appropriately (such as wheelchairs and
commodes)
Educating families and carers
Half of falls incidents within the RCH occur when a parent or carer is present. Whilst most parents are aware of maintaining a safe environment for their children in the home environment, many are unaware of the environmental risks when in hospital due to being in an unfamiliar environment accompanied with increased levels of anxiety related to hospital admission.
The hospitalisation of children provides an opportunity to reinforce parent/carer information and education concerning normal psychological and motor development of small children, which is related to falls risks and other hazards both inside and outside hospital.
Parents/carers should be encouraged to:
- Reinforce hospital orientation with their
child
- Provide non slip footwear for their child
whilst in hospital - no mobilizing in socks
- Maintain physical contact with infant when
cot sides are down, when bathing or weighing their infant
- Assist their child to the toilet when
appropriate
- Use bed rails or cot sides where appropriate
when leaving child's bedside, even for short periods
- Inform nursing staff when their child is
unattended
- Assist child with mobilising as needed when
out of bed/cot
- Familiarise themselves with the parent fact sheet to ensure they understand and are aware
of the potential risk of falls in hospitals Preventing falls in
hospital. Parents
can download the RCH kids health app to access all RCH fact sheets.
- Patients and carers are encouraged to participate
in the development and use of falls prevention management plans while in
hospital
Risk Assessment
All patients have a falls risk
assessment completed using the Little Schmidy
Falls Risk Assessment Tool completed at the following stages:
- On admission or as soon as practical after
the admission
- Daily or when a patient's condition changes
- When the patient is transferred from one
ward/department to another
- Following a fall incident
![]()
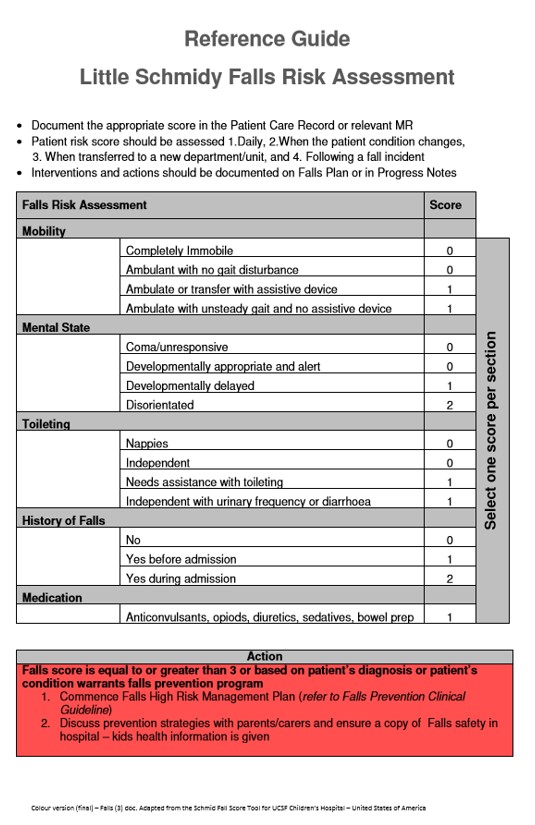
The falls risk assessment score
is documented in the Primary Assessment flow sheet in the EMR.
The falls risk assessment tool
does not replace clinical judgment, if a patient does not present with a high
risk score but is thought to be high risk by medical or nursing staff, allied
health, parents or carers extra precautions to protect such patients should be
documented and actioned
Factors influencing risk
include:
Factors influencing risk include:
- Environmental Issues: Are a common cause of
falls, some examples of previous incidents at the RCH have included
inappropriate use of cot side or side rails, equipment clutter, wet
floors, nurse call buttons out of patient reach or the use of faulty
equipment. By implementing the standard safety measures listed above
these risks can be greatly reduced
- Age: RCH incident data identified the adolescent
group (10-17 years) have the highest risk of falls in hospital closely
followed by the toddler group (1 -2 years). The developmental stage and
ambulation capabilities are key potential fall risk factors
- Medical Diagnosis: Various medical
conditions may increase a child's risk of falling. Some high risk
diagnosis includes drop seizures, severe ataxia, epilepsy surgery or
patients who have had a craniectomy, for these patients soft helmets may
be considered
- Mental State: Altered mental state is
the most commonly identified risk factor for falling and is perhaps the
most difficult to manage in terms of minimizing the risk of falling.
Assessment of bed and sleeping safety should be completed for those with
significant neurological impairment, who might be impulsive. Agitated, or
have symptoms associated with Post
Traumatic Amnesia (PTA)
- Mobility: Impaired mobility and orthopeadic
restrictions are key potential fall risk factors, interventions such as
non slip footwear, supervising or assisting with transfers can reduce
risk
- Elimination: Special toileting needs are a factor for
increased risk of falling. Simple strategies such as regularly checking
patients and toileting patients regularly will help minimise risk
- Bedrest: The majority of falls occur at the
patient's bedside, interventions such as ensuring the bed is in a low
position, the brakes are locked, appropriate use of bed rails and
ensuring patients can reach necessary items will reduce the risk of
falling
- Medications: Use of medications such as Barbiturates,
Phenothiazines, Sedatives, Hypnotics, Antidepressants, Laxatives and
Diuretics may increase the risk of falls. Care should be taken to check
the patient regularly following administration and inform the
parents/carers of possible associated side effects
- Length of Stay: RCH incident data shows
that most of our patients who fall do so in the first 5 days of admission
and have had previous admissions to hospital
- History of Falls: Patients who have a
history of falls in hospital or at home have an increased risk of falling
again, appropriate precautions should be implemented
See
Clinical Guideline (Nursing): Nursing Assessment for more detailed assessment information.
Management
Standard safety measures should be put in place for all patients regardless of the risk identified.
Falls score equal to or greater than 3 necessitates the implementation of a Falls High Risk Management Plan which is located in the Primary Assessment flowsheet within the EMR.
Falls score equal to or greater
than 3 necessitates the implementation of a Falls High Risk Management Plan which is located in the Primary Assessment
flowsheet within the EMR.
For all patients identified as
high risk, i.e., those with a falls risk score of 3 or greater; a Falls High
Risk Management Plan must be commenced. The plan will be developed in
collaboration with the child's parent or carer and will be specific to the
patient's individual needs.
The plan will remain in use until
the patients falls risk score changes. If the falls risk score alters a new
plan will be implemented as the patients needs may have changed. Patient risk
should continue to be assessed daily, once the patient's risk score is less
than 3 and the patient's risk of falling is reduced, a management plan is no longer
required; however it is important that a safe environment is always maintained.
A referral may be needed to a
physiotherapist or an occupational therapist if there has been a change to a
patients mobility or function during an admission.
A physiotherapist can advise as
to how to safely support the patient during positioning, transfers, standing,
walking and use of mobility aids.
An occupational therapist can
ensure safe setup of the ward bedroom, bathroom and toilet to minimise falls
risks and recommend management techniques/assistive equipment for self care
tasks.
In the event of the occurrence of
a fall:
- Ensure patient safety
- Provide immediate supportive action for the child
- Conduct a physical examination, measure and document vital signs
- Commence neurological observation if the child's head was the first point of impact
- Do not move the patient until injuries are identified
- Notify appropriate medical staff
- Ensure safe transfer back to bed, consider using a hoist if necessary
Documentation of a Falls event
-
Record the incident in the EMR, including:
description of event (location, activity occurring, time, who was
present), assessment findings, interventions and patient outcomes,
notification of the incident to the parent.
- Report the incident through the hospital
incident reporting system, VHIMs. All falls, including near misses should
be reported. The information from reported falls is used to gain insight
of the causes of falls for patients at the RCH and continuously improve
the local falls prevention program
- The Medical staff/AUM or NUM to inform
the parents if they are not present that: A fall has occurred
- Update the falls risk assessment and management
plan after a fall has occurred
Considerations for discharge
Some patients may have a high
risk score at the time of discharge. For this patient group the following
should be considered:
-
Parent/carer education, tips and advice on how to manage their child in the home environment
- A referral to an occupation therapist and/or physiotherapist may be necessary if the patient at the time of discharge is below their baseline mobility and function.
- An Occupational Therapy referral - to assist parents and carer in the safe setup of the home environment and recommend management techniques/assistive equipment for self care tasks.
- A Physiotherapy referral - to educate parents and carers how to safely support their child during positioning, transfers, standing, walking and use of mobility aids.
High risk patients may be eligible for Post Acute Care (PAC). To make a
referral contact the RCH Complex Care Hub.
Companion Documents
Little Schmidy Falls Risk Assessment Tool
Paediatric
Fall and Entrapment Prevention and Management Guideline Appendix
B: Paediatric Cot and Bed Allocation Guide (attached below)
Links
Evidence Table
Click here to view the
evidence table.
Please remember to
read the disclaimer.
The development of this nursing guideline was coordinated by Sarah Sly, Improvement Manager, and approved by the Nursing Clinical Effectiveness Committee. Updated April 2022.