See also
Febrile child
Sepsis
Local antimicrobial guidelines
Key points
- Orbital cellulitis is an emergency with serious complications including intracranial infection, cavernous sinus thrombosis and vision loss
- Urgent imaging and surgical consultation (ENT and ophthalmology) should be considered for any child with suspected orbital cellulitis
- Periorbital cellulitis in a well child can often be treated with oral antibiotics if follow-up is assured
Background
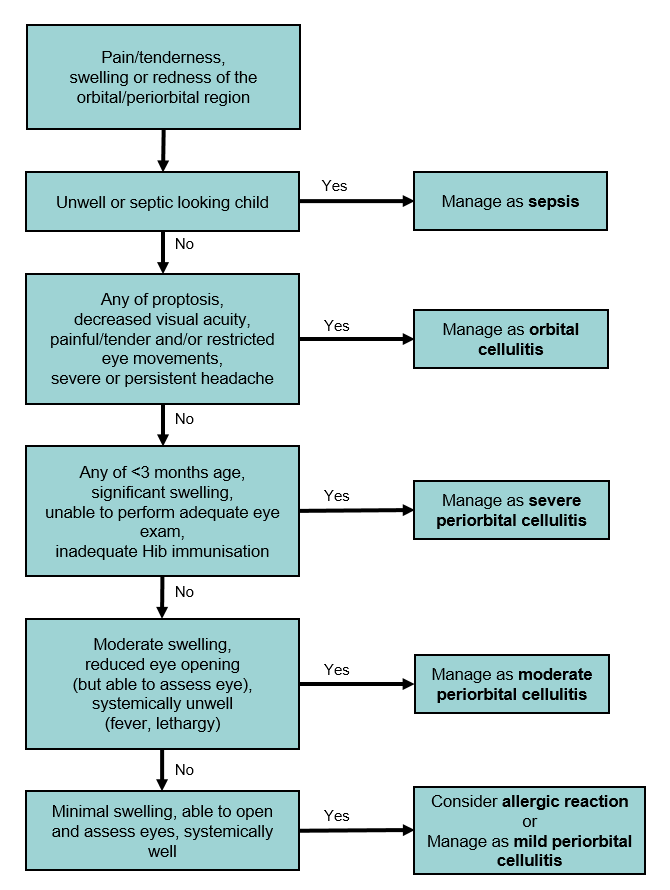
- Periorbital and orbital cellulitis are distinct clinical diseases, though have overlapping clinical features and therefore can be difficult to differentiate
- Orbital cellulitis:
- infection within the orbit, (ie postseptal,
the structures posterior to the orbital septum)
- surgical emergency with major complications
including loss of vision, abscess formation, venous sinus thrombosis and
extension to intracranial infection with subdural empyema, and meningitis
- the majority (>80%) of cases relate to local
sinus disease
- Periorbital cellulitis:
- infection of the eye lids and surrounding skin
not involving the orbit (ie preseptal, the structures anterior
to the orbital septum)
- The globe is not involved in either infection
Assessment
Typical presentation of periorbital/orbital cellulitis
- Unilateral eyelid swelling and erythema
- Unilateral eye pain or tenderness
Consider gonorrhoea and Chlamydia infections in neonatal presentation (send PCR swabs) see Acute red eye
Red flags concerning for orbital
cellulitis
- Painful or restricted eye movements
- Visual impairment:
- reduced acuity
- relative afferent pupil defect
- diplopia
- Proptosis
- Severe headache or other features of intracranial involvement
Differential diagnosis
Bilateral findings and/or painless (or non-tender) swelling in a well looking child is more likely to be an allergic reaction
Management
Antimicrobial recommendations may vary according to local antimicrobial susceptibility patterns; please refer to local guidelines; these may include advice regarding community acquired MRSA
Orbital cellulitis
- Admission
- Keep fasted until need for surgery clarified
- Seek ENT and Ophthalmology advice urgently
- Consider urgent contrast enhanced CT scan of orbits, sinuses +/- brain
- Investigations:
- FBE and blood culture
- Lumbar puncture is contraindicated due to risk of raised intracranial pressure secondary to possible intracranial extension
- Antibiotics (see below)
- Treat underlying sinus disease eg nasal decongestants, steroids (often guided by ENT)
Periorbital cellulitis
Severe
Inpatient investigations and management as per orbital cellulitis
Moderate
Inpatient management or consider Hospital In The Home (HITH) admission if available locally
- Consider blood culture if febrile and unwell
- Antibiotics (see below)
- Once improving change to oral antibiotics
- If not improving or deteriorating within 24–48 hours, consider managing as severe periorbital cellulitis
Mild
Summary of antibiotic treatment
|
Intravenous therapy |
Oral therapy |
Total duration |
|
Orbital cellulitis |
3rd generation cephalosporin
- Cefotaxime 50 mg/kg (max 2 g) IV 6 hourly OR
- Ceftriaxone 100 mg/kg (max 4 g) IV daily
If suspected MRSA, add vancomycin (see link for dosing) Duration based on clinical severity and improvement. Usually at least
3-4 days, then switch to oral
|
Amoxicillin with clavulanic acid (doses based on amoxicillin component) 22.5 mg/kg (max 875 mg) oral bd
|
10–14 days |
Severe periorbital cellulitis
|
Moderate periorbital cellulitis |
Cefazolin 50 mg/kg (max 2 g) IV 8 hourly OR Ceftriaxone 50 mg/kg (max 2 g) IV daily (HITH) OR If suspected MRSA, Clindamycin 15 mg/kg (max 600 mg) IV 8 hourly OR oral
Duration based on clinical severity and improvement. Usually 1-2 days,
then switch to oral |
When improving, switch to oral antibiotics as per mild periorbital cellulitis
If suspected MRSA: Clindamycin 15 mg/kg (max 600 mg) oral TDS OR Trimethoprim/sulfamethoxazole (8/40 mg/mL) 4/20 mg/kg (max 320/1600 mg) oral BD
|
7–10 days |
|
Mild periorbital cellulitis |
Not applicable |
Cefalexin 20 mg/kg (max 750 mg) oral TDS OR Cefuroxime
3 months – 2 years: 10 mg/kg (max 125 g), 2 – 12 years: 15 mg/kg (max 250 mg) oral BD |
7-10 days |
Consider
consultation with local paediatric team when
- Orbital cellulitis suspected
- Moderate-severe periorbital cellulitis present
- No improvement or deterioration after 24–48 hrs of therapy
Consider
transfer when
- Severe periorbital cellulitis or orbital cellulitis present
- Suspecting intracranial involvement with altered conscious state, seizures or focal neurological signs
- Child requires care above the level of comfort of local hospital
For emergency advice and paediatric or neonatal ICU
transfers, see Retrieval
Services
Consider
discharge when
Mild periorbital cellulitis:
- oral antibiotic course prescribed
- follow-up assured
Moderate periorbital cellulitis:
- after 24–48 hrs of IV antibiotics and with improvement
- able to tolerate oral antibiotics
- follow-up assured
Last updated December, 2021