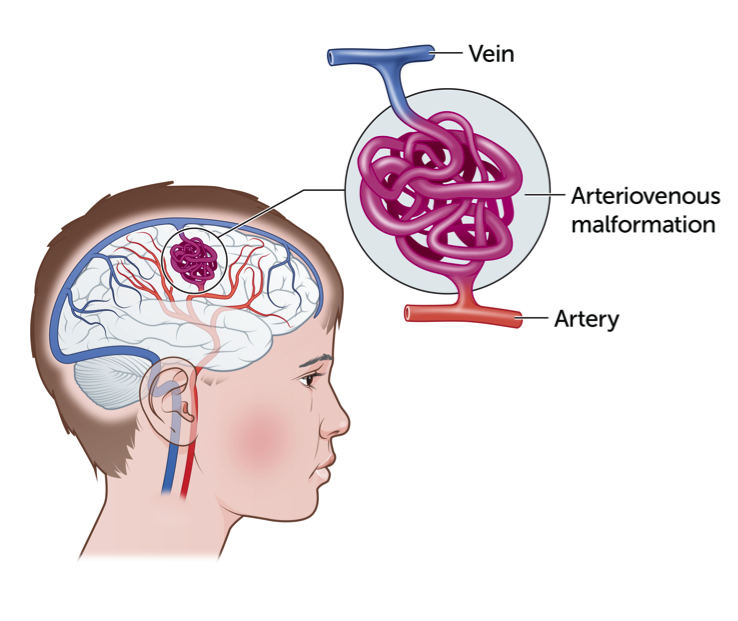
A Cerebral Arteriovenous Malformation (AVM) is a collection of tightly tangled, abnormal looking, and enlarged blood vessels. AVMs are abnormal and complex connections between arteries and veins which interfere with the circulation of blood. As a result, some AVMs can burst and cause bleeding into or around the brain, which is also known as a haemorrhagic stroke. A haemorrhagic stroke is a medical emergency and requires immediate treatment.
AVMs can occur anywhere there are blood vessels, including the brain. It is believed that most AVMs develop before birth when the brain is developing, although they are thought to be relatively rare in children.
What causes a Cerebral Arteriovenous Malformation?
The exact cause of an AVM is not known, however they are thought to develop in a child during their mother’s pregnancy, or soon after birth. AVMs are not directly inherited, they are not infectious and do not spread to other parts of the body.
AVMs in the brain occur in approximately 1 in 3,300 people and bleeding from an AVM most often occurs between 10 and 30 years of age.
Signs and symptoms of a Cerebral Arteriovenous Malformation
In most cases, there are no signs or symptoms of an AVM until it bursts. However, in some cases, symptoms can include:
- seizures
- brief stroke like symptoms (weakness of the face, arm and/or leg down one side of the body; tingling or numbness of the face, arm and/or leg down one side of the body; difficulty speaking and/or difficulty understanding speech; sudden onset severe headache) with exertion or blood pressure changes
The symptoms of a burst AVM usually come on very suddenly, this is known as a haemorrhagic stroke. Every patient is affected differently and the severity of symptoms depends on the size and location of the bleeding.
Symptoms of a haemorrhagic stroke include
- sudden severe headache with no known cause
- drowsiness and/or loss of consciousness and collapse
- sudden onset of impaired vision, slurred speech, weakness of the face and arm and/or leg
- seizures
- sudden onset of dizziness or loss of balance.
How is a Cerebral Arteriovenous Malformation diagnosed?
An AVM may be diagnosed by a MRI/MRA scan, a CT scan or a cerebral angiogram.
MRI/MRA scan: A Magnetic Resonance Imaging (MRI) machine or scanner uses a powerful magnet and radio waves to take very clear and detailed pictures of the body. It is useful for looking at many parts of the body and often gives extra information to plain X-rays, ultrasounds or CT scans. During an MRI scan, the part of the body being scanned will have images taken from several different angles. The magnetic field used in an MRI is believed to be safe even in the second half of pregnancy. There is no ionizing radiation (e.g. X-rays) used in an MRI.
An MRI scan allows doctors to determine what part of the brain is affected by the AVM.
In addition to the MRI, a Magnetic Resonance Angiogram (MRA) may also be completed. An MRA specifically looks at the blood vessels in the brain and neck and those around the AVM.
CT scan: a CT scan or computed tomography imaging is a type of X-ray. The CT scanner uses X-rays to create cross-sectional images of all or a part of the body. A CT scan can be performed on any area of the body.
Cerebral angiogram: A cerebral angiogram is an X-ray test where a dye is injected directly into an artery through the groin whilst your child is under anaesthetic. This test gives detailed pictures of the arteries and veins (blood vessels) of the brain. This test is performed to look for abnormalities in blood vessels.
Treatment for a Cerebral Arteriovenous Malformation
Your child’s treatment will depend on their own situation. However, a bleeding AVM in the brain (haemorrhagic stroke) is a medical emergency and requires immediate attention. The AVM may also require a combination of treatments.
The goal of emergency treatment is to prevent further complications by limiting bleeding, controlling the pressure of suddenly expanding blood on the brain tissue, controlling seizures (if any) and, if possible, removing the AVM.
Conservative management: if there are no or almost no symptoms, or if the AVM is in an area that can’t be easily treated, conservative management may be needed. Conservative management means avoiding invasive procedures and monitoring the AVM with frequent brain scans.
Brain surgery: to completely remove an AVM in the brain and evacuate any dangerous bleeding, brain surgery may be necessary for your child.
Stereotactic radiosurgery/radiotherapy: if an AVM has not ruptured, or is small and in an area that may be difficult or unsafe to reach, stereotactic radiosurgery or radiotherapy may be appropriate. In this procedure, a cerebral angiogram is done to find the AVM. High energy sources are then placed on the AVM to produce damage to the blood vessels. This causes a scar and will allow the AVM to slowly “close off”. This means there will be no blood coming in or out of the AVM. The “close off” usually occurs over a one-two year period.
Interventional/endovascular neurosurgery: It may be possible to treat part or (less commonly) all of the AVM by placing a catheter (a small tube) inside the blood vessels that supply blood to the AVM, to block off blood flow to abnormal blood vessels. Materials used to block off these vessels can include liquid tissue adhesives (glue) and micro coil. The best treatment depends on the location and size of the AVM.
Going home and follow up
Prior to going home, frequent family meetings may be held and a potential discharge date will be set. The health care team will discuss ongoing medical management and future goals for your child. If ongoing rehabilitation is required, your child will return to the hospital for outpatient therapy or may be connected with community services for ongoing support.
Your child will have regular surveillance imaging and follow-up appointments with their treating team.
Key points to remember
- AVMs can occur anywhere there are blood vessels, including the brain
- an AVM is a collection of tightly tangled, abnormal looking, and enlarged blood vessels. As a result, some AVMs can burst causing bleeding into or around the brain, which is also known as a haemorrhagic stroke
- AVMs in the brain occur in approximately 1 in 3,300 people
- the symptoms of a burst AVM usually come on very suddenly, this is known as a haemorrhagic stroke. Every patient is affected differently and severity of symptoms depends on the size and location of the bleeding
- your child’s treatment will depend on your child’s situation. A bleeding AVM is a medical emergency and requires immediate attention.
For more information
Common questions our doctors are asked
Can a cerebral AVM grow back or come back?
Yes it is possible that after treatment for a cerebral AVM there may be recurrence of a tiny cluster of AVM vessels in the area treated. This is why your treating team of doctors will arrange follow up imaging (with MRI or angiogram) for several years after the initial treatment to check for this possibility. The chances of this developing is small but if it does develop it will require further treatment.
Developed by The Royal Children's Hospital Neurology and Neurosurgery departments. We acknowledge the input of RCH consumers and carers.
Reviewed May 2020.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit
www.rchfoundation.org.au.