Although stroke is commonly thought of as an adult condition, stroke can occur in children at any age, including in the womb. Strokes are caused when the brain does not get enough oxygen, causing injury to the brain cells. Usually happens when there is reduced blood supply to the brain or when there are low levels of oxygen in the blood. Stroke is more common in new born babies than in older children.
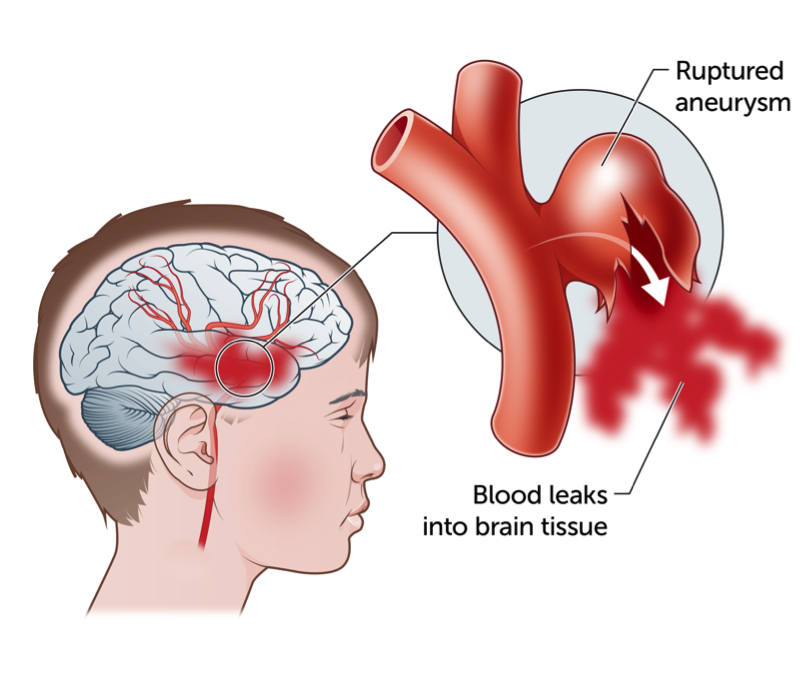
There are two types of strokes, an ischaemic stroke and a haemorrhagic stroke. A haemorrhagic stroke occurs when a blood vessel (artery or vein) leaks or bursts and bleeding occurs into an area of the brain.
What causes haemorrhagic stroke?
A haemorrhagic stroke occurs when a blood vessel bursts within the brain (intracerebral haemorrhage). The bleed itself can cause direct injury to the brain, while the blood can irritate the brain, causing swelling and potentially further injury.
Signs and symptoms of a haemorrhagic stroke
The symptoms of haemorrhagic stroke usually come on very suddenly. Every patient is affected differently and the severity of symptoms depends on the size and location of the bleeding. Symptoms of a haemorrhagic stroke include:
- sudden severe headache with no known cause
- drowsiness and/or loss of consciousness/collapsing
- sudden onset of impaired vision, slurred speech, weakness of the face, arm and/or leg (often on only one-side)
- seizures
- sudden onset of dizziness or loss of balance.
How is a haemorrhagic stroke diagnosed?
A haemorrhagic stroke may be diagnosed by a CT scan, a MRI/MRA scan, or a cerebral angiogram.
CT scan: a CT scan or computed tomography imaging is a type of X-ray. The CT scanner uses X-rays to create cross-sectional images of all or a part of the body. A CT scan can be performed on any area of the body.
MRI/MRA scan: A Magnetic Resonance Imaging (MRI) machine or scanner uses a powerful magnet and radio waves to take very clear and detailed pictures of the body. It is useful for looking at many parts of the body and often gives extra information to plain X-rays, ultrasounds or CT scans. During an MRI scan, the part of the body being scanned will have images taken from several different angles. The magnetic field used in an MRI is believed to be safe even for unborn babies. There is no ionizing radiation (e.g. X-rays) used in an MRI.
An MRI enables doctors to determine what part of the brain is affected by the stroke.
Cerebral angiogram: A cerebral angiogram is an X-ray test where a dye is injected directly into an artery through the groin whilst your child is under anaesthetic. This test gives detailed pictures of the arteries and veins (blood vessels) of the brain. This test is performed to look for abnormalities in blood vessels which may have caused the bleed.
Immediate treatment for haemorrhagic stroke
In some cases, a haemorrhagic stroke may require emergency surgery to remove the blood from the brain to relieve the pressure and swelling.
The surgical procedure is called a craniotomy. This is where a temporary window is made in the skull with a special drill that will allow the neurosurgeon to access your child’s brain. The neurosurgeon then removes the blood clot or inserts a tube to drain blood and fluid from the brain and minimise the pressure.
In some cases where the extra pressure and fluid can’t be relieved immediately, an external ventricular drain (EVD) may be inserted. An EVD is a temporary system that allows drainage of fluid from the brain.
What associated conditions can cause a haemorrhagic stroke?
A haemorrhagic stroke can be caused by underlying blood vessel problems and other medical conditions. Underlying blood vessel problems can include:
Ateriovenous malformation (AVM): An AVM is a collection of tightly tangled, abnormal, often enlarged blood vessels, which connect arteries and veins and thus contains blood under higher pressure. Most AVMs have no symptoms before they rupture. In some cases they may have a small leak initially which may irritate the brain and cause a seizure, and in some cases they are found unexpectedly on a scan done for other reasons. If an AVM ruptures, it caused bleeding within the brain, which is a haemorrhagic stroke.
Cerebral aneurysms: A cerebral aneurysm is a bulging, weak area in the wall of a blood vessel in the brain. Brain aneurysms in children are less common than in adults. Typically, aneurysms in children have no symptoms until they burst. A burst aneurysm can cause bleeding into the brain which can expand within the brain or put pressure on the area surrounding the brain.
Cavernoma: A cavernoma is an abnormal cluster of blood vessels than contains lower pressure blood flow in the brain. Unlike AVMs, cavernomas have low blood flow, which means they more commonly have small leaks, and may have had several leaks over time before they cause any symptoms, rather than the high pressure bleeds of an AVM.
Other causes of haemorrhagic stroke include
- blood clotting disorders
- head injuries
- brain tumours
- brain surgery
What are the effects of stroke?
Each child recovers from their stroke differently as recovery is dependent on the size and location of the stroke. The most common problems following stroke may include:
- weakness in one arm and/or leg
- trouble speaking, reading and/or writing
- changes to the way things are felt when touched (sensory problems)
- problems thinking or remembering (cognitive problems)
- changes to the way things are seen or felt (perceptual problems)
- trouble swallowing
- tiredness/physical and mental fatigue (also known as cognitive fatigue)
- problems controlling feelings
- seizures (particularly in babies and younger children).
In babies and very young children, the effects of stroke may not be obvious and can become more noticeable over time. Therefore, it is important that their development is closely followed over time.
Recovery and rehabilitation
It can be difficult to predict how a child will recover following a stroke. For some children, recovery can be remarkably quick, whereas other children may experience a slower recovery.
Much is still not known about how children’s brains compensate for the damage caused by stroke. Some brain cells may only be temporarily damaged and may resume functioning. In some cases, the brain can re-organise its own functioning and another part of the brain can take over.
Recovery after stroke is the greatest in the first few months, sometimes recovery can plateau, although further gains may be made for some years.
Rehabilitation can start as soon as the patient is stable. Rehabilitation treatments vary between patients because stroke affects people differently. Once acute medical intervention is no longer required, rehabilitation goals may be made. Rehabilitation may take place on the rehabilitation unit in your child’s treating hospital, or as an outpatient, and/or at home.
A rehabilitation team consists of many professionals, these can include
- rehabilitation physicians/specialists
- physiotherapists – to help with mobility and daily functioning
- occupational therapists – also for help with daily functioning, particularly hand function, and some types of visual and thinking problems due to stroke
- speech therapists – for help with communication and swallowing problems
- neuropsychologists – for help with thinking (cognition) and social interactions after stroke
- psychologists – for help with mood problems
- education advisors – for education support during hospitalisation as well as planning a return to school after stroke
- social workers – for family, accommodation and parking support during hospitalisation.
Going home and follow-up
Prior to going home, frequent meetings with your child’s treating team may be held and a potential discharge date will be set. Before going home, the health care team will discuss ongoing medical management and future goals. If ongoing rehabilitation is required, your child may return to the hospital for outpatient therapy or may be linked to community services for ongoing support.
Your child should have regular surveillance imaging and follow-up appointments with their treating team at the hospital.
Key points to remember
- A haemorrhagic stroke (brain bleeding) occurs when a blood vessel bursts within the brain (intracerebral haemorrhage).
- The symptoms of haemorrhagic stroke usually come on very suddenly.
- In some cases, a haemorrhagic stroke may require emergency surgery to remove the blood from the brain to relieve the pressure and swelling.
- A haemorrhagic stroke can be caused by underlying blood vessel problems, including an AVM, a cerebral aneurysm, head injuries and other medical conditions.
- Recovery following a stroke takes time. Although it is very difficult to predict how a child will recover following a stroke, recovery can be remarkably quick in some cases and slower in others.
For more information
Common questions our doctors are asked
Will my child make a full recovery?
Your child’s recovery will depend on the location, size and severity of their stroke. Each child recovers at a different pace. You will be kept updated about your child’s recovery and progress throughout the admission and during your outpatient reviews.
Is there a chance my child may have another stroke?
This depends on the underlying cause of your child’s stroke. If for example, your child suffered a haemorrhagic stroke as a result of a ruptured AVM, the risk of a recurrent stroke will be dependent on whether the AVM has been treated. Your child’s treating medical team will explain these risks to you in more detail.
Are there any medications my child should avoid following a haemorrhagic stroke?
Your child should avoid taking medications that increase their risk of bleeding (blood thinners).
Developed by The Royal Children's Hospital Neurology and Neurosurgery departments. We acknowledge the input of RCH consumers and carers.
Reviewed April 2020.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit
www.rchfoundation.org.au.