See also
Basic Paediatric ECG interpretation
Dehydration
Diabetic ketoacidosis (DKA)
Electrolyte abnormalities
Hyperkalaemia
Intravenous fluids
Key points
- The oral/enteral route is preferred for potassium administration
- Intravenous potassium is a high-risk medication and carries risks of inadvertent hyperkalaemia, fluid overload, and peripheral vein extravasation and thrombophlebitis. Rapid intravenous administration or overdose may cause cardiac arrhythmia or arrest
- Monitor fluid status and electrolytes in all children receiving potassium replacement. Children with an initial serum potassium <3.0 mmol/L should have cardiac monitoring, as should those receiving IV replacement
- Specialist advice should be sought for critical (K <2.0 mmol/L) or symptomatic hypokalaemia
Background
Hypokalaemia is defined as a plasma potassium level less than 3.5 mmol/L
| Severity |
Serum potassium (mmol/L) |
Mild |
3.0-3.4 |
Moderate |
2.5-3.0 |
Severe |
2.0-2.4 |
Critical |
<2.0 |
- In normal acid-base status, a 1 mmol/L decrease in serum potassium concentration represents a whole-body deficit of at least 200 mmol. Concurrent metabolic acidosis may falsely elevate the serum potassium and lead to an underestimation of total body deficit. Metabolic alkalosis can have the opposite effect
- Hypokalaemia is commonly associated with hypomagnesaemia. Serum magnesium should be measured and replaced as required
Causes of hypokalaemia
Decreased intake |
Increased losses |
Transcellular shifts |
Medications |
Spurious |
Illness
Fasting
Prolonged IV fluids not containing potassium
Eating disorder
Poor nutrition |
Gastrointestinal
- Vomiting
- Diarrhoea
- Fistula
- Laxative overuse
Renal
- Osmotic diuresis
- Aldosterone excess
- Mineralocorticoid excess
- Congenital disorders
- Renal artery stenosis
|
Metabolic alkalosis
Hypomagnesaemia
Hypernatraemia
Glucose/insulin administration
Diabetic ketoacidosis
Refeeding syndrome |
Loop diuretics eg furosemide
Thiazide diuretics
Amphotericin
Cisplatin
Insulin
Beta-agonists eg salbutamol,
adrenaline |
Sampling error
- Recent line flush
- IV fluids near sampling site
|
Prevention
In general, children eating a variety of foods will meet their daily potassium requirements (approximately 2-4 mmol/kg/day)
Consider maintenance fluids containing potassium (see Intravenous fluids) for children who are
- Nil by mouth and not receiving enteral fluids for prolonged periods, particularly if associated with increased losses
- At risk of hypokalaemia, see table above for causes
Assessment
History
- Hypokalaemia is often asymptomatic
- Symptoms of hypokalaemia are more likely when serum levels rapidly decrease to below 3 mmol/L
- Skeletal muscle weakness, paralysis (in severe cases)
- Smooth muscle weakness: ileus, constipation, nausea, vomiting
- Lethargy
- Fatigue
- Confusion
- Polyuria, usually if prolonged hypokalaemia
- Features of underlying cause
- Acute diarrhoea/vomiting
- Decreased intake
- Use of medications such as salbutamol, diuretics, laxatives
- History of hypoaldosteronism
Examination
- Tachycardia, bradycardia, arrhythmia
- Fluid status (see Dehydration)
- Decreased muscle strength, hypotonia and decreased deep tissue reflexes
Management
Investigations
- Repeat potassium to verify initial result
- Serum potassium level can be falsely elevated in haemolysed/finger prick samples. A venous sample should be taken if clinical suspicion of hypokalaemia
- Urea, creatinine and electrolytes
- BGL
- Venous blood gas
- Magnesium, especially if hypokalaemia is refractory to treatment (hypomagnesaemia promotes potassium wasting)
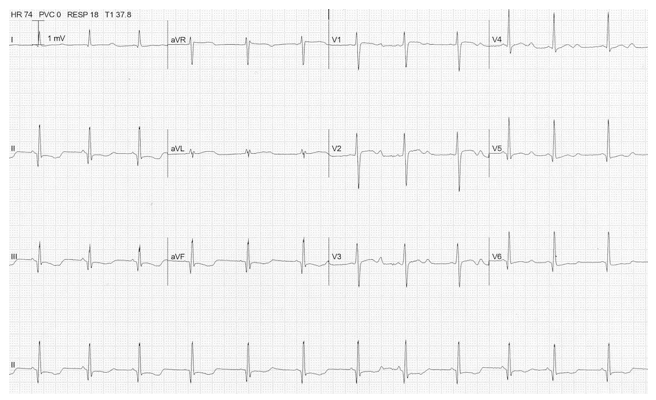
- ECG: if signs/symptoms of hypokalaemia, risk of cardiac arrhythmia, or serum potassium <3 mmol/L. See Basic Paediatric ECG interpretation
- Decreased T wave amplitude (usually earliest manifestation)
- Increased P wave amplitude
- T wave changes (flattening, inversion)
- ST changes (usually depression)
- Appearance of U wave
- QT prolongation
- Ventricular ectopic beats
- Arrhythmia
Treatment
Goals of treating hypokalaemia are to
- Prevent life threatening complications: arrhythmias, paralysis, rhabdomyolysis, diaphragmatic weakness
- Replace potassium deficit
- Identify and treat reversible causes, address underlying conditions
Replacement
Ensure child is passing urine before commencing potassium replacement
Potassium replacement is indicated if
- Serum potassium <3.0 mmol/L
or
- Serum potassium <3.5 mmol/L with symptoms, signs and/or ECG changes
In mild hypokalaemia (serum levels 3.0-3.5 mmol/L), optimal treatment depends on clinical situation. Consider:
- No acute treatment, monitor electrolytes
- Increasing maintenance potassium dose
- Replacing orally/IV if anticipated ongoing losses or inadequate intake
In children with stable haemodynamics and no ECG changes, aim for a gradual correction over 24-48 hours
Measure and correct serum magnesium as necessary
Route of administration
The oral/enteral route is preferred
- Potassium is well absorbed from the gastrointestinal tract
- It is best taken with or soon after food to reduce gastrointestinal irritation
Intravenous potassium replacement should be considered in
- a child who is unable to tolerate enteral medication
- an initial serum potassium <2.5 mmol/L
- presence of ECG changes
Oral/enteral dosing
Dosage
|
Acute replacement dose |
1-2 mmol/kg/dose orally (maximum 20 mmol per dose)
Dose may be repeated, after checking serum potassium level, to a maximum of 5 mmol/kg/day (maximum total daily dose 50 mmol) |
Maintenance dose
(if required) |
2-5 mmol/kg/day orally in divided doses (maximum 20 mmol per dose) |
Medication forms
|
Potassium content |
Notes |
Potassium chloride oral mixture (where available) |
1.33 mmol/mL |
- Rapid absorption
- Expected serum potassium rise after approximately 2 hours
|
Effervescent tablet
eg Chlorvescent® |
14 mmol per tablet |
- Rapid absorption
- Ensure tablets are completely dissolved before administration
- Expected serum potassium rise after approximately 2 hours
|
Controlled release enteric coated
eg Slow K®
(for maintenance dosing) |
8 mmol per tablet |
- Slow release, delayed absorption
- Use for mild or chronic hypokalaemia
- Tablets must be swallowed whole
- Expected serum potassium rise after approximately 4 hours
|
For acute oral potassium replacement, consider repeat serum potassium level at a time interval guided by the clinical context and the expected serum potassium rise
Intravenous dosing
Dosage
- Rapid intravenous administration or overdose may cause fatal cardiac arrhythmia or arrest. Administer via an infusion pump using Dose Error Reduction Software (DERS) where available. Note that concentrated potassium solutions should only be administered in critical care settings
- Include all sources of potassium when calculating replacement doses and infusion rates, eg additives to maintenance fluids, parenteral nutrition, oral/enteral supplements
- Potassium-containing fluids, including parenteral nutrition, may need to be paused during acute replacement to ensure the maximum rate of potassium administration is not exceeded
Acute intravenous potassium replacement dose
Acuity of treating area |
Acute replacement dose |
ECG monitoring required |
Repeat serum potassium level |
General ward |
0.2 mmol/kg/hour for 3 hours (max 10 mmol/hour)
Note: Dose likely to require intravenous fluid rate greater than maintenance fluid rate |
Only required if serum potassium <3 mmol/L or risk of cardiac arrhythmia |
1 hour after replacement completion
Check serum potassium level before administering further replacement |
Critical care area |
0.4 mmol/kg/hour for 1-2 hours (max 20 mmol/hour)
Note: Likely to require concentrated potassium infusion (see below) and central line |
Yes |
1 hour after replacement commencement
and
1 hour after replacement completion |
Maintenance dose (if required):
- 1-4 mmol/kg/day (max 10 mmol/hour)
- Doses greater than 4 mmol/kg/day should be discussed with a senior clinician or local retrieval service
Administration
Only administer potassium chloride IV by infusion. Never flush after potassium chloride infusions
Intravenous access |
Potassium concentration |
Dosage form |
Notes |
Peripheral line |
Usual maximum 40 mmol/L
(discuss with senior clinician if giving 40-60 mmol/L) |
Use premixed fluid bags where possible (various concentrations available)
When adding potassium chloride to an IV fluid bag, mix well by inverting the bag at least 10 times
Clearly label all bags, syringes, pumps and lines that contain potassium to avoid inadvertent flushing
Premixed product 10 mmol potassium chloride in 100 mL 0.29% sodium chloride can be administered via a peripheral line as the product is isotonic due to the reduced sodium content
|
Monitor intravenous access site for signs of extravasation or thrombophlebitis |
Central line |
Concentrations >60 mmol/L must be given via a central line only (maximum rate 0.4 mmol/kg/hour) |
There are several concentrated potassium formulations available
Only administer in areas where there is a clear protocol for administration and monitoring
Contact local retrieval service for further advice
|
Use should be approved by a senior clinician
ECG monitoring required |
Monitoring
Ensure regular monitoring of:
- vital signs
- clinical and fluid status including urine output
- any signs of hyperkalaemia (see Hyperkalaemia)
- IV site for phlebitis or Extravasation
Consider consultation with local paediatric team when
- Child requires admission
- Child requires potassium replacement
Consider transfer when
- Serum potassium <2.0 mmol/L
- Symptomatic hypokalaemia especially paralysis
- Significant ECG changes such as arrhythmia, ventricular or supraventricular ectopic beats, ST changes, T wave inversion
- Renal impairment, including oliguria or high/rising creatinine
- Risk of arrhythmia
- Fluid overload
- Neonates
- Child with complex medical condition
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
- Asymptomatic
- Potassium >3.0 mmol/L and stable
- Fluid losses replaced and ongoing replacement possible
- Plan for ongoing monitoring (ie repeat levels) in place
Additional information
ECG: ST depression, T wave inversion, prominent U waves
Last updated October 2024