See also
Basic Paediatric ECG interpretation
Electrolyte abnormalities
Intravenous fluids
Resuscitation: Care of the seriously unwell child
Resuscitation: Hospital management of cardiopulmonary arrest
Key points
- Moderate or severe hyperkalaemia can cause life-threatening arrhythmias and cardiac arrest. Perform an ECG and commence cardiac monitoring
- Stop any medications or fluids which cause hyperkalaemia
- Seek specialist advice for children with underlying renal disease or complex co-morbidities
Background
Hyperkalaemia:
- Serum potassium >5.5 mmol/L (normal range = 3.5-5.0 mmol/L), or
- Serum potassium >6.0 mmol/L in neonates
Severity |
Serum potassium (mmol/L) |
Mild |
5.5-6.0 |
Moderate |
6.1-7.0 |
Severe |
>7.0 |
Hyperkalaemia is potentially life threatening, and can result in arrhythmias and sudden death
Causes of hyperkalaemia
| Decreased excretion |
Increased production |
Transcellular shifts |
Medication |
Exogenous
source |
Pseudohyperkalaemia |
- Renal disease (acute/chronic renal failure, renal anomaly)
- Adrenal mineralocorticoid deficiency
|
- Trauma
- Rhabdomyolysis (crush injury, convulsion, infection)
- Haemolysis
- Tumour lysis syndrome
- Burns
|
- Acidosis (diabetic ketoacidosis, lactic acidosis)
- Hypertonicity (hyperglycaemia)
|
- NSAIDs
- Trimethoprim
- Heparin
- Chemotherapy
- K-sparing diuretic
- ACE inhibitor
- Angiotensin II receptor blockers
- Beta-blockers
- Succinylcholine
- Digoxin
- Mannitol
|
- Iatrogenic potassium administration (oral, IV)
- Increased ingestion
- Massive transfusion
|
- Artefact of collection process or technique (eg haemolysed sample)
- Significant thrombocytosis (platelets >1000 x 109/L)
- Significant leucocytosis (WCC >70 x 109/L)
|
Assessment
History and examination
Hyperkalaemia can be initially asymptomatic or can present with severe symptoms and signs:
- Nausea, vomiting
- Fatigue
- Paraesthesia, muscle weakness, reduced tendon reflexes, flaccid paralysis
- Ileus
- Respiratory depression/hypoventilation
- Palpitations, arrhythmia, syncope, cardiac arrest
Assess for possible causes (see table above)
Management
Investigations
Children with moderate or severe hyperkalaemia need continuous cardiac monitoring and IV access
Confirm potassium level with a second sample
- If initial potassium level is critically high and hyperkalaemia is likely based on clinical scenario, initiate treatment before waiting for a repeat venous sample result
- Acute increase of potassium is associated with higher risk of arrhythmia
Do an ECG to identify conduction disturbance (see Additional information and Basic paediatric ECG interpretation)
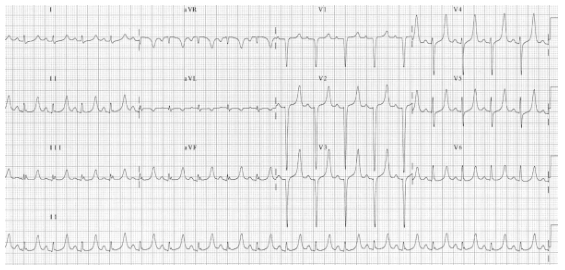
- Tall/peaked T wave (early)
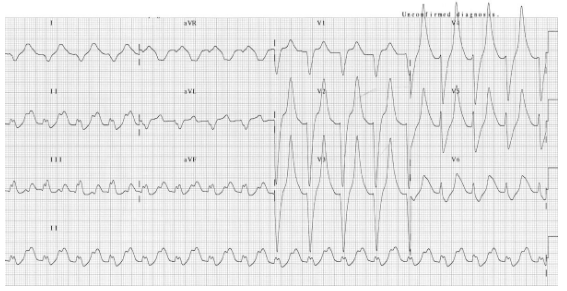
- Prolonged PR interval
- Flattening, widening or loss of P wave
- Widening of QRS (increased risk of arrhythmia)
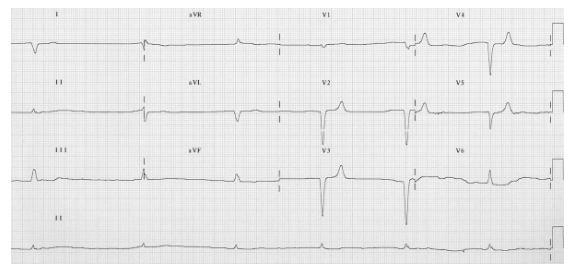
- Bradyarrhythmia, conduction blocks
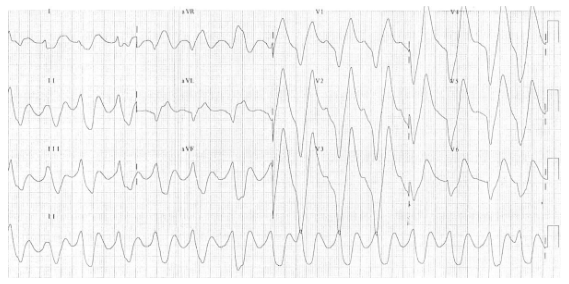
- Severe hyperkalaemia: sine wave (fusion of QRS and T wave), ventricular arrhythmia, pulseless electrical activity, asystole
A normal ECG does not exclude risk for arrhythmia. Life threatening arrhythmia can occur without warning
Other investigations
- Urea, creatinine and electrolytes
- Blood glucose level
- Venous blood gas
- +/- urine analysis and urinary electrolytes
- Consider other investigations based on suspected underlying cause:
- CK
- Cortisol, aldosterone and hormonal precursor levels (particularly if hyponatraemia)
- Digoxin level (if relevant)
Treatment
Goals of treating hyperkalaemia are
- Correct underlying cause
- Discontinue any potassium-containing fluids or medications
- Stabilise cardiac membrane in life-threatening hyperkalaemia with ECG changes: calcium IV
- Reduce serum potassium levels
- Shift potassium into cells: salbutamol nebulised, insulin and glucose IV
- Remove potassium from body: resonium PR
.png)
Medications
Calcium
Stabilises myocardium in life-threatening hyperkalaemia (does not reduce potassium)
2 options
- Calcium gluconate 10%: 0.15 mmol/kg, maximum 6.6 mmol
(0.68 mL/kg, max 30 mL), slow IV/intraosseous injection over 2-5 minutes if unstable, 15-20 minutes if stable- Preferable if only peripheral line available, as less irritant to veins
- Calcium chloride 10%: 0.14 mmol/kg, maximum 6.8 mmol
(0.2 mL/kg, max 10 mL) slow IV/intraosseous injection over 2-5 minutes if unstable, over 15-20 minutes if stable
Continuous cardiac monitoring. Discontinue if heart rate drops significantly
- Monitor closely for extravasation
- Not to be given simultaneously with bicarbonate
- Not to be given if digoxin toxicity
- Onset of action: <3 minutes. Should see normalisation of ECG. If not, repeat dose (twice) or IV infusion titrated to response
- Duration of action: approximately 30 minutes
Salbutamol
Salbutamol via nebuliser
- ≤25 kg: 2.5 mg neb 1-2 hourly
- >25 kg: 5 mg neb (max 10-20 mg) 1-2 hourly
- Onset of action: 30 minutes
- Duration of action: 2-3 hours
Only consider salbutamol IV if severe hyperkalaemia AND after discussion with senior clinician. Monitor for tachycardia
Insulin and glucose (give together)
Severe hyperkalaemia
- Glucose 10% 5 mL/kg IV bolus (if no hyponatraemia)
- Insulin short acting (eg Actrapid®) 0.1 unit/kg IV bolus (max 10 units)
- Followed by insulin/glucose infusion (see below)
Moderate hyperkalaemia
- Glucose 10% with 0.9% sodium chloride IV at maintenance rate
- Insulin short acting (eg Actrapid®) infusion: 0.1 unit/kg/hour IV
Insulin administration:
Insulin vials are highly concentrated in relation to dosage and have a high risk of medication error
To safely prepare the insulin dose, first dilute 10 units of insulin (= 0.1 mL) to a total of 10 mL with sodium chloride 0.9% to make a final concentration of 1 unit/mL. Withdraw the prescribed insulin dose from this 1 unit/mL solution
- Close monitoring of glucose every 30-60 minutes
- Onset of action: 15 minutes
- Duration: peak 60 minutes, 2-3 hours
Bicarbonate
In metabolic acidosis only
- Severe hyperkalaemia and metabolic acidosis
- Sodium bicarbonate 8.4% 1 mmol/mL: administer 1-3 mmol/kg (1-3 mL/kg) IV over 5 minutes
- Mild to moderate hyperkalaemia and metabolic acidosis
- Sodium bicarbonate 8.4% 1 mmol/mL: administer 1 mmol/kg (1 mL/kg) slow IV infusion over 30 minutes
- Do NOT give simultaneously with calcium
- Onset of action: 30-60 minutes
- Duration: 2-3 hours
Polystyrene sulfonate resins (resonium)
- Mild effect, multiple doses necessary, may be used as long-term agent
- Sodium polystyrene sulfonate (Resonium A®) or calcium polystyrene sulfonate (Calcium Resonium®) 0.5-1 g/kg 6 hourly (max 30 g) PR or oral (with lactulose)
- Not to be used if ileus, recent abdominal surgery, perforation, or hypernatraemia
- Repeat if required
- Separate oral administration from other oral medications by at least 3 hours
- Onset of action: 1 hour PR, 4-6 hours oral
- Duration: variable
Dialysis
To be organised with local paediatric renal or intensive care team. Transfer to tertiary centre
Consider consultation with local paediatric team when
- All children with moderate or severe hyperkalaemia
- Underlying medical cause eg renal abnormalities
Consider transfer when
- All children with severe hyperkalaemia
- All children requiring dialysis
- Child requiring care beyond the comfort level of the hospital
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
- Potassium level is normal and stable
- Child is asymptomatic with normal ECG
- Cause of hyperkalaemia identified and treated adequately
Additional information
ECG: peaked T waves
ECG: prolonged PR interval, broad bizarre QRS complexes, peaked T waves
ECG: bradyarrhythmia, slow junctional rhythm, peaked T waves
ECG: huge, peaked T waves, sine wave appearance
Last updated August 2024