Introduction
A wound is a disruption to the integrity of the skin that leaves the body vulnerable to pain and infection. The skin is the body’s largest organ and is responsible for protection, sensation, thermoregulation, metabolism, excretion and cosmetic. Poorly managed wounds are one of the
leading causes of increased morbidity and extended hospital stays. Therefore, wound assessment and management is fundamental to providing nursing care to the paediatric population.
Aim
The guideline aims to provide information to assess and manage a wound in paediatric patients. Ongoing multidisciplinary assessment, clinical decision-making, intervention, and documentation must occur to facilitate optimal wound healing.
Definition of Terms
PHYSIOLOGY OF WOUND HEALING
Wound healing occurs in four stages, haemostasis, inflammation, proliferation and remodelling, and the appearance of the wound will change as the wound heals. The goal of wound management is to understand the different stages of wound healing and treat the wound accordingly.
- Haemostasis(occurs within the first few seconds): blood vessels constrict to stop bleeding and form blood clots
- The goal of wound management: to stop bleeding
- Inflammation(0-4 days): neutrophils and macrophages work to remove debris and prevent infection. Signs and symptoms include redness and swelling.
- The goal of wound management: to clean debris and prevent infection
- Proliferation(2-24 days): the wound is rebuilt with connective tissue to promote granulation and repair the wound
- The goal of wound management: to promote tissue growth and protect the wound
- Remodelling(24 days- 1 year): epithelial tissue forms in a moist healing environment
- The goal of wound management: to protect new epithelial tissue
WOUND CLASSIFICATION
- Acute wound: a wound which occurs suddenly and progresses through the stages of healing as expected
- Chronic wound: a wound which fails to progress or progresses slowly through the stages of healing. Healing can be greater than 4-6 weeks.
- Surgical wound: a wound which is secondary to surgical intervention e.g. scalpel incision, surgical drain
- Non-surgical wound: an acute or chronic wound which is not secondary to surgical intervention
Assessment
Wound Assessment
Having the knowledge, skills and resources to assess a wound will result in positive outcomes, regardless of product accessibility.
Time
TIME is a valuable acronym or clinical decision tool to provide systematic assessment and documentation of wounds. It stands for Tissue, Infection or Inflammation, Moisture balance and Edges of the wound or Epithelial advancement.
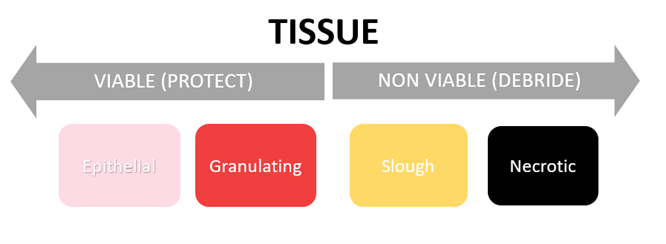
Tissue
Tissue is usually described by colour.
- Epithelial tissue: Appears pink or pearly white and wrinkles when touched. Occurs in the final stage of healing when the wound is covered by healthy epithelium.
- Granulating tissue: Appears red and moist. Occurs when healthy tissue is formed in the remodelling phase that is well vascularised and bleeds easily.
- Slough tissue: Appears yellow, brown or grey. Slough is devitalised tissue made of dead cells or debris.
- Necrotic tissue: Appears hard, dry and black. Necrotic tissue is dead tissue that prevents wound healing.
- Hyper granulating tissue: Appears red, uneven or granular. Occurs in the proliferative phase when tissue is over grown.
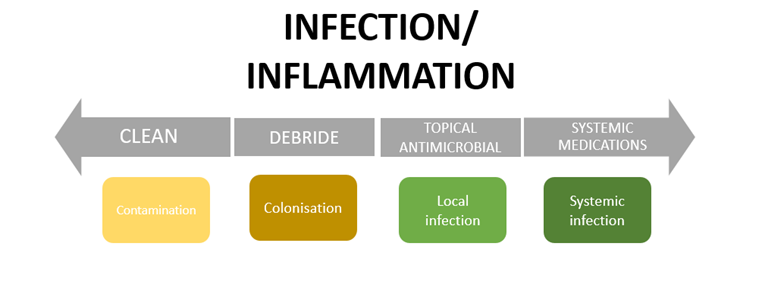
Infection/Inflammation
Inflammation is an essential part of wound healing; however, infection causes tissue damage and impedes wound healing.
- Contamination: The presence of microorganisms that are contained and do not multiply. It does not provoke a host response so healing is not impaired. Antimicrobials are not indicated.
- Colonisation: Microorganisms multiply but do not provoke a host response. The infection is contained but wound healing may be delayed. Antimicrobials are not indicated.
- Local infection: Invasion by an agent that, under favourable conditions, multiplies and produces effects that are injurious to the patient. When microorganisms and bacteria move into the wound tissue and invokes a host response. Healing is impaired and can lead to wound breakdown. Topical
antimicrobials are indicated.
- Spreading and
systemic infection: Microorganisms spread from the wound through the vascular and or lymphatic systems and involves either a part of the body (spreading) or the whole body (systemic). Healing is impaired. A systemic approach is needed e.g. topical antimicrobials and the use of antibiotics to
prevent sepsis.
- Biofilms: represent a survival mechanism of microorganisms and are therefore ubiquitous in nature. They are complex, slime-encased communities of microbes which are often seen as slime layers on objects in water or at water-air interfaces. The degree of bioburden in the wound from the microorganisms is
indicated by a poor response to antimicrobial or antibiotic treatment, delayed wound healing or increase in exudate or inflammation.
Odour
ODOUR can be a sign of infection. It can be described as:
- No odour
- Slight malodour: odour when the dressing is removed
- Moderate
malodour: odour upon entering the room when the dressing is removed
- Strong malodour: odour upon entering the room when dressing is intact
If any of the above clinical indicators are present (including fever, pain, discharge or cellulitis) a medical review should be initiated and consider a Microscopy & Culture Wound Swab (MCS).
Moisture/Exudate
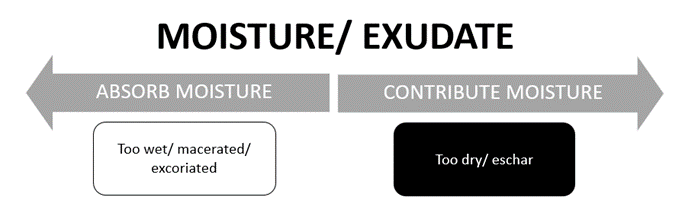
Moisture/ exudate is an essential part of the healing process. It is produced by all wounds to:
- Maintain a moist environment
- Cleanse the wound
- Provide nutrients and white blood cells
- Promote epithelialisation
The overall goal of exudate is to effectively donate moisture and contain it within the wound bed. Excess exudate leads to maceration and degradation of skin, while too little moisture can result in the wound bed drying out.
Exudate description:
- Serous: appears clear to yellow. Normal, typical in the inflammatory phase. Serous drainage is clear, thin, and watery.
- Haemoserous: appears clear to yellow with a pink tinge. Typical in the inflammatory or proliferative phase.
- Sanguineous: common exudate blood. Can be associated with hyper granulation.
- Purulent: containing pus milky, typically thicker in consistency, grey, green or yellow. This indicates infection.
- Haemopurulent: blood and pus. Often due to an established infection.
Edges
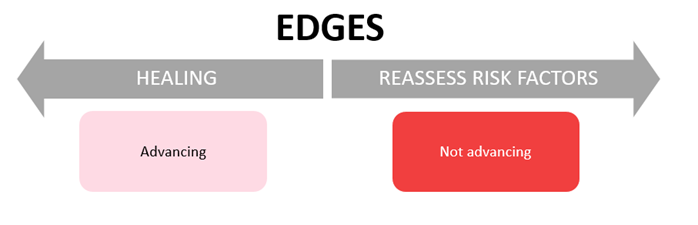
Advancing of edges can be assessed by measuring the depth (cavity/sinus), length and width of the wound using a paper tape measure.
- Advancing: edges are pink. Healing is taking place.
- Not advancing: edges are raised, rolled, red or dusky. Go back to stages of wound healing and goals of wound management and consider factors affecting wound healing (see below). Is there something that is not being addressed?
Surrounding skin
Assess the surrounding skin (peri wound) for the following:
- Cellulitis: redness, swelling, pain or infection
- Oedema: swelling
- Macerated: soft, broken skin caused by increased moisture
Pain
Pain is an essential indicator of poor wound healing and should not be underestimated. Pain can occur from the disease process, surgery, trauma, infection or as a result of dressing changes and poor wound management practices.
Assessing pain before, during, and after the dressing change may provide vital information for further wound management and dressing selection. See RCH
Pain assessment and measurement guideline.
Accurate assessment of pain is essential when selecting dressings to prevent unnecessary pain, fear and anxiety associated with dressing changes. Prepare patients for dressing changes, using pharmacological and non-pharmacological techniques as per the RCH
Procedure Management Guideline.
Factors affecting wound healing
Factors affecting wound healing can be extrinsic or intrinsic. It is essential for optimal healing to address these factors.
Extrinsic/
local factors:
- Wound management practices and moisture balance (e.g. wound dehydration or maceration)
- Stable temperature (approximately 37oC)
- Neutral or acidic pH
- Infection
- Wound location
- Mechanical stress, pressure or friction
- Presence of foreign bodies
Intrinsic/
systemic factors:
- Nutrition
- Underlying or chronic disease
- Decreased mobility
- Impaired perfusion
- Medications (including immunotherapy, chemotherapy, radiation or NSAIDs)
- Mental health (including stress, anxiety or depression)
- Patient knowledge, understanding or compliance
- Age of patient
Management
Wound Management
Effective wound management requires a collaborative approach between the nursing team and treating medical team. Referrals to the Stomal Therapy, Plastic Surgery, Specialist Clinics or Allied Health teams (via an EMR referral order) may also be necessary for appropriate management and dressing selection, to optimise wound
healing.
Wound healing may be by:
- Primary intention: the wound edges can be pulled together e.g. surgical incision (using sutures, staples, steristrips or glue), small wounds, paper cuts
- Secondary intention: the wound edges don’t come together and need dressing products to promote granulation
- Tertiary intention/ delayed primary intention: the wound is cleaned before it can be closed due to a high risk of infection e.g. contaminated wounds
- Negative pressure wound therapy: Topical negative pressure or vacuum assisted closure (VAC) is a foam dressing attached to a device to assist with wound closure, proliferation, moisture removal and stabilisation of the wound environment. Typically used in open or dehisced wounds, grafts, flaps or
pressure injuries.
Frequency of dressing changes:
- Frequency of dressing changes is led by the treating team or indicated by product manufacturers
- Consider less frequent dressing changes in the paediatric population to promote wound healing and prevent unnecessary pain and trauma
- It is advised that wounds are reviewed at least every 7 days to monitor wound healing and reassess goals of wound management
Procedure
Things to consider prior to procedure:
- Can the dressings be removed by the patient at home or prior to starting the procedure?
- Are there any hygiene requirements for the patient to attend pre procedure (eg shower/bath for pilonidal sinus wounds)?
- Does the patient need pain management or procedural support? See
Procedure Management Guideline
- Is the environment suitable for a dressing change?
- How will the patient be best positioned for comfort whilst having clear access to the wound?
- Select either
standard aseptic technique or surgical aseptic technique.
- Is all the appropriate equipment available or does this need to be sourced from a different area?
- Do the treating team need to review the wound or do clinical images need to be taken?
1. Inform and consent patient
2. Perform hand hygiene
3. Clean surfaces to ensure you have a clean safe work surface
4. Perform hand hygiene
5. Open and prepare equipment, peel open sterile equipment and drop onto aseptic field if used (dressing pack, appropriate cleansing solution, appropriate dressings, stainless steel scissors, tweezers or suture cutters if required)
6. Perform hand hygiene, use gloves where appropriate
7. Remove dressings, discard, and perform hand hygiene
8. Clean and assess the wound (wound and peri wound should be cleaned separately if washing the patient)
9. Perform procedure ensuring all key parts and sites are protected
10. Perform hand hygiene and change gloves if required
11. Apply new dressings
12. Apply fixation if required
13. Perform hand hygiene
14. Dispose of single-use equipment into waste bag and clean work surface
a. Single-use equipment: dispose after contact with the wound, body or bodily fluids (not into aseptic field)
b. Multiple-use equipment: requires cleaning, disinfection and or sterilisation after contact with the wound, body or bodily fluids
c. Stainless steel scissors that do not come into contact with the wound, body or bodily fluids can be re-used for the sole purpose of cutting that patient’s unused dressings. Scissors should be cleaned with an alcohol or disinfectant wipe before and after use.
Wound Cleansing
Cleansing
solutions:
Ensure cleansing solutions are at body temperature.
- Potable (drinkable tap) water
- Washing under a shower may be appropriate after carefully considering the risks associated with contamination from pathogenic microorganisms
- Sterile water
- Normal saline
- Surfactants or antiseptics for biofilm or infected wounds e.g. Prontosan™
Cleansing
technique:
- Avoid immersion or soaking wounds in potable water
- Washing the wound must be separated from washing the rest of the body
- Use a scrubbing or irrigation technique rather than swabbing to avoid shedding fibres
See also
RCH Procedure Skin and surgical antisepsis
Principles of Aseptic
Technique:
Standard or surgical aseptic technique is used as per the RCH Procedure Aseptic
Technique.
- Standard aseptic technique: selected for simple wound dressings, usually procedure of less than 20- minute duration. Involves few key parts or key sites. Use nonsterile gloves, a general aseptic field and non-touch techniques (or sterile gloves when directly
touching a key part or key site).
- Surgical aseptic technique: selected for large or complex wound dressings that involve a longer duration and more key parts or key sites. Use sterile gloves, a critical aseptic field, and sterile solutions.
Select personal protective equipment (PPE) where appropriate. Outlined in the Procedures:
Standard Precautions and
Transmission based precautions
Debridement:
Debridement is the removal of dressing residue, visible contaminants, non-viable tissue, slough or debris. Debridement can be enzymatic (using cleansing solutions), autolytic (using dressings) or surgical.
Determining when debridement is needed takes practice. If you are not familiar with wound assessment/debridement confer with a senior/expert nurse.
For complex wounds any new need for debridement must be discussed with the treating medical team.
Dressing Selection
It is important to select a dressing that is suitable for the wound, goals of wound management, the patient and the environment.
Primary
Dressings:
Dressings that have direct contact with the wound and have the ability to change the wound (e.g. moisture donation/ retention, debridement and decreasing bacterial load)
|
TYPE |
EXAMPLES |
USE |
DURATION |
|
Silver dressing |
Acticoat 7™
Aquacel Ag™
Mepilex Ag™
PolyMem Silver™ |
-Broad spectrum antimicrobial agent to reduce/ treat infected wounds
-If the silver needs to be activated, it should be done with water (normal saline will deactivate the silver) |
Can be left on for 7 days (Acticoat3™ is changed every 3 days). Should only be used for 2-3 weeks |
|
Alginate |
Kaltostat™
Algisite™
Sorbsan™ |
-Moisture management for moderate- high exudate
-Absorbs fluid to form a gel (can be mistaken for slough)
-To fill irregular shaped wounds e.g. cavities
-Ideal for bleeding wounds due to haemostatic properties |
Change every 1-7 days depending on exudate. Stop using once wound bed is dry |
|
Foam |
Allevyn™
Tielle™ |
-For low- high exudate
-Used for granulating and epithelializing wounds as it provides protection
-Can be used in conjunction with other dressings to increase absorption and prevent maceration
-Not to be used with hydrogel |
Change every 1-7 days depending on exudate |
|
Hydro fibre |
Aquacel™ |
-Moisture management for moderate- high exudate
-To fill irregular shaped wounds e.g. cavities. Needs to be bigger than the wound as it will shrink in size
-Prevents peri wound maceration |
Continue to use until there is low- nil exudate |
|
Impregnated gauze |
Xeroform™
Mepitel™
Bactigras™
Jelonet™ |
-Protects the wound base and prevents trauma to the wound on removal
-Does not absorb exudate |
Can be left on for up to 14 days (for orthopaedic wounds) |
|
Dry dressing |
OpSite™
Primapore™
Gauze |
-Protective dressing for low- moderate exudate
-Can adhere to the wound bed and cause trauma on removal (consider the use of an atraumatic dressing/ impregnated gauze) |
Stop using when exudate is too high or the wound has healed |
|
Hydrocolloid |
Comfeel™
Duoderm™
Hydrocoll™ |
-Moisture donation for low-moderate exudate
-Self-adhesive and water repellent
-Forms a gel when exudate present (white bubbles)
-Not for use in infected wounds
-Can be used as a primary or secondary dressing |
Change every 3-7 days |
|
Iodine dressing |
|
-Iodine is only be used in acute superficial wounds as it can damage granulating tissue so should be used with caution
-Has antifungal and antibacterial properties |
|
|
Hydrogel |
Instrasite Gel™
Intrasite Conformable™
SoloSite™
Burnaid™ |
-Moisture donation for low- moderate exudate
-Used on dry/ necrotic wounds as it hydrates the wound bed and promotes autolytic debridement |
Change every 3-7 days depending on exudate |
|
Film dressing |
Tegaderm™
OpSite™ |
-Protective dressing for nil-low exudate
-Non-adsorbent
-Water resistant
-Allows for inspection through dressings |
|
|
Silicone foam |
Mepilex™
Mepilex Lite ™
Allevyn Gentle™ |
-Protective dressing for low- heavy exudate
-Absorbs moisture and distributes pressure (good for pressure injuries)
-Atraumatic to the wound and surrounding skin
-Can be used on infected wounds |
Change every 1-7 days depending on exudate |
|
Silicone foam adhesive |
Mepilex Border™
Allevyn Gentle Border™ |
-Same as silicone foam but includes adhesive film |
|
|
Medical honey |
Medihoney™
Manuka Honey™ |
-For infected, contaminated or malodorous wounds as it promotes autolytic debridement |
|
|
Hypertonic saline |
Mesalt™ |
-For moderate-high exudate or hypergranulation tissue
-Used for moist necrotic wounds and draining infected wounds |
For best results change frequently (more than once daily). Stop using when wound is granulating or epithelising |
Secondary
dressings:
Dressings that cover/ compliment primary dressings and support the surrounding skin.
|
TYPE |
EXAMPLE |
USE |
LENGTH |
|
Absorbent/ Protective pad |
Melolin™ |
-Provides protection for moderate exudate
-Can adhere to the wound bed and cause trauma on removal (consider the use of an atraumatic dressing) |
|
|
Fabric tape |
Hypafix™
Fixomull™
Mefix™ |
-Permeable dressing but can be washed and dried
-Conforms to the body and controls oedema
-Can be used as a primary dressing or secondary dressing as well |
|
|
Tape |
Micropore™ |
-Provides wound support
-Non allergenic |
|
|
Tubular bandage |
Tubular Form™ (Tubigrip)
Tubifast™ |
-Provides protection and compression |
|
|
Bandage |
Crepe bandage
Elastic conforming gauze bandage (handiband) |
-Provides extra padding, protection and securement of dressings |
|
* Dressings not available on ward imprest/more extensive dressing supplies can be sourced in hours from
stores or
EDC.
Documentation
It
is an expectation that all aspects of wound care, including assessment,
treatment and management plans are documented clearly and comprehensively.
Documentation of wound assessment and management is completed in the EMR under the Flowsheet activity (utilising the LDA tab or Avatar activity), on the Rover device, hub, or planned for in the Orders tab. For more information follow the
Parkville EMR | Nursing – Documenting Wound Assessments (phs.org.au)
Clinical images are a valuable assessment tool that should be utilised to track the progress of wound management. See
Clinical Images- Photography Videography Audio Recordings policy for more information regarding collection of clinical images.
Discharge Planning
Wound management follow up should be arranged with families prior to discharge (e.g. Hospital in the Home, Specialist Clinics or GP follow up).
- Education can be provided on
Wound Care at home using the Kids Health Info app or fact sheets.
- Families can be directed to the RCH
Equipment Distribution Centre or local pharmacy for extra dressing supplies.
Companion Documents
Links
Evidence Table
The evidence table for this guideline can be viewed here.
Please remember to read the disclaimer
The revision of this clinical guideline was coordinated by Mica Schneider, RN, Platypus. Approved by the Clinical Effectiveness Committee. Updated February 2023.