Table of contents will be automatically generated here...
Introduction
Femoral fractures are often managed using skin traction prior to their definitive surgical management. Some require short term traction i.e. 24 hours whereas others require it for a number of weeks i.e. 6 weeks. Traction limits movement and reduces the fracture to help decrease pain, spasms and swelling. The purpose of traction is to restore and maintain straight alignment and length of bones following fractures.
Aim
This clinical guideline aims to ensure that the application and management of skin traction is consistent and that potential complications are identified early and managed correctly.
Definition of terms
- Fracture: Any type of break in a bone.
- Traction: Traction is the application of a pulling force to an injured part of the body or extremity.
- Skin traction (bucks traction): Skin traction is applied by strapping the patient’s affected lower limb and attaching weights.
- Counter traction: Application of force in the opposite direction used to oppose/offset traction.
- Neurovascular observations: Are an assessment of circulation, oxygenation and nerve function of limbs within the body.
- Compartment syndrome: Increased pressure within one of the body's compartments which contain muscles and nerves, causing pain, muscle and nerve damage due to insufficient blood flow.
Management
Acute management
- Ensure order for skin traction is documented by the Orthopaedic Team – (including weight to be applied in kilograms)
- Preparation of equipment:
- Hospital traction bed with bar at the end of the bed
- Traction kit paediatric OR adult size (foam stirrup with rope and bandage)
- Overhead traction frame
- Pulley
- Traction weight bag
- Water
- SleekTM (high strength waterproof adhesive strapping tape)

Image 1: Traction kit in adult and child
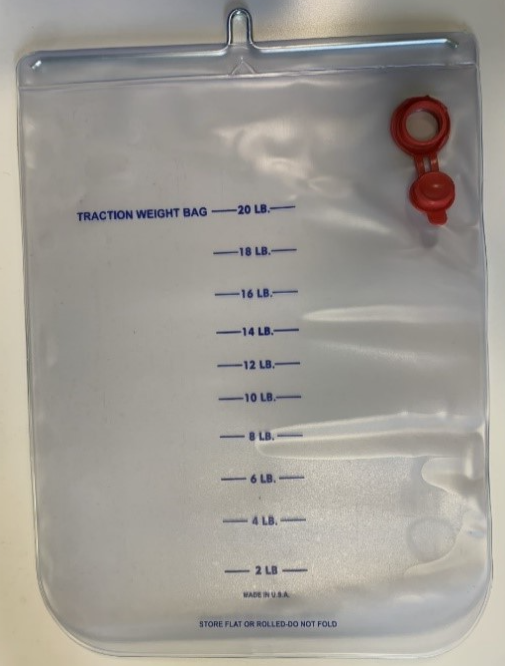
Image 2: Traction weight bag
Pain relief medications
- A femoralnerve block is the preferred pain management strategy and should be administered in the Emergency department prior to being admitted to the ward.
- Diazepam, paracetamol, and oxycodone should always be charted and used in conjunction with the femoral nerve block.
Education
- Explain the procedure to the parents and patient before commencing.
- Plan appropriate distraction from play therapy, parents or other nursing staff.
- See
Procedural Management Guideline.
Application of traction
Preparation
- A minimum of two nurses will be required for the application of traction.
- Before applying traction ensure that the patient’s skin and neurovascular observations have been assessed on the affected limb and compared to the non-affected limb and have been appropriately documented. Large abrasions or lacerations may be contraindications to skin traction.
- Ensure all equipment is ready at the bedside prior to starting and that the patient has had adequate analgesia.
- Ensure the correct amount of water has been added to the traction weight bag as per medical orders.
- Before starting tie the rope to the bottom of stirrup ensuring a strong knot has been tied.
Apply traction
- Discuss procedure with child and family.
- Prepare child by having them lay flat on the traction bed.
- Put foam stirrup around the arch of foot on patients affected limb, ensuring the stirrup is even on both sides.
- The second nurse will assist by lifting the patients’ leg off the bed to allow for easier application of the crepe bandage. While doing this the nurse will need to support the limb in natural alignment (knee and toes to celling) and apply gentle manual traction to the affected limb.
- The long sides of the stirrup will sit along the outside and inside of the patient’s ankle and lower leg.
- The first nurse is to start to apply the crepe bandage, starting at the patient’s ankle, and working the way up the lower leg using a figure 8 bandaging technique.
- Ensure the bandages and stirrup are free of wrinkles and bumps that could cause pressure.
- Secure crepe bandage with tape.
- Place rope over the pulley and attach traction weight bag. If necessary, trim rope to ensure traction weight bag is suspended in the air and does not rest on the floor.
- Rope must always be in pulley system ensuring it is taut and in vertical line with the patients’ limb.

Image 3: foam stirrup applied to patients’ leg.

Image 4: Stirrup and crepe bandage applied to leg
Ongoing management
Maintain skin integrity
- Patient’s legs, heels, elbows and buttocks may develop pressure areas due to remaining in the same position and the pressure of the bandages.
- Position a rolled-up towel/pillow under the heel to relieve potential pressure.
- Encourage the patient to reposition themselves or complete pressure area care four hourly.
- Remove the foam stirrup and bandage once per shift, to relieve potential pressure and observe the condition of the patient’s skin. At this time, while the bandages are down you can moisturise the skin.
- Minimise the sheet's wrinkles and aim to keep dry to reduce potential skin damage.
- Assess and document the condition of skin throughout care in the progress notes and care plan.
- Ensure that the pressure injury prevention score and plan is assessed every shift and documented.See
Pressure injury prevention and management.
Traction care
- Ensure that the traction weight bag is hanging freely, this bag must NOT rest on the bed or the floor.
- If the rope becomes frayed replace immediately.
- The rope must be in the pulley tracks at all times, and should be vertically aligned with the patients’ leg, not on an angle.
- Ensure the bandages are free from wrinkles which may cause pressure injury.
- The bed can be tilted to maintain counter traction, reducing slide down the bed, however ensure the weight is hanging freely.
- The formula for calculating traction weight is 10% of a patient’s body weight, unless otherwise stated by the medical team.
Observations
- Check the patient’s neurovascular observations hourly and document in flowsheets. See the
Neurovascular observation guideline.
- If the bandage is too tight it can cause blood circulation to be slowed. If this is the case the bandage will need to be removed and reapplied maintaining circulation.
- Monitoring of swelling of the femur should also occur to observe for compartment syndrome.
- If neurovascular compromise is detected, remove the bandage and reapply bandage. If circulation does not improve notify the orthopaedic team.
Pain Assessment and management
- Regular hourly assessment of pain is essential to ensure that the correct analgesia is administered to manage the patient’s pain.
- Paracetamol, diazepam and oxycodone should all be charted and administered as necessary.
- Pre-emptive analgesia ensures that the patient’s pain is sufficiently managed and should be considered prior to pressure area care.
- Assess and document outcomes of all employed pain management strategies.
Activity
- The patient can sit up in bed and participate in quiet activities such as craft, board games and watching TV. Child Life Therapy will be beneficial for patients in traction long term.
- Non-pharmacological distraction and activity will improve patient comfort.
- The patient can move in bed as tolerated for hygiene to be completed.
- Patients who are in traction for several weeks should have a referral to the education department/kinder.
Theatre time
- The patient should be transported to theatre in traction to reduce pain and maintain alignment.
Special considerations
- The foam stirrup, bandage and rope are single patient use only.
- Traction may be contraindicated in someone with large abrasions or lacerations.
Potential complications
- Skin breakdown/pressure areas
- Neurovascular impairment
- Compartment syndrome
- Joint contractures
- Constipation from immobility and analgesics
Companion documents
References
- Ahmed, A., Beaupre, L., Rashiq, S., Dryden, D., Hamm, M., Jones, A. (2011). Comparative effectiveness of pain management interventions for hip fracture: a systematic review. Annals of internal
medicine, 155(4), 234-246.
- Anglen, J. & Choi, L. (2005). Treatment options in Paediatric Femoral Shaft Fractures. Journal
of Orthopaedic Trauma, 19 (10),724-733.
- Bailey, J. (2003). Orthopaedic care. Nursing Center, 33(6), 58-63.
- Parker, M. Handoll, P. (2009). Pre-operative traction for fractures of the proximal femur in adults. The Cochrane Collaboration, 1-30.
- Hedin, H., Borgquist, L. & Larsson, S. (2004). A cost analysis of three methods of treating femoral shaft fractures in children.Acta Orthopaedic Scand, 75 (3), 241-248.
- Orthopaedic Traction: Care and management (2014). The Children’s Hospital Westmead Practice Guideline.
- Pressure area prevention management clinical practice guideline (2014). Royal Children’s Hospital.
- Split Russell’s/Bucks Traction (2012). Cincinnati Children’s Health Topics.
- Saygi, B., Ozkan, K., Eceviz, E., Tetik, C. & Sen, C. (2010) Skin traction and placebo effect in the preoperative pain control of patients with collum and intertrochanteric femur fractures. Bullentin of the NYU Hospital for joint
diseases, 68(1) 15-17.
- Smith, C. (1994). Nursing the patient in traction. Nursing Times, 36-39.
- Stewart, J. & Hallett, J. (1994). Traction and orthopaedic appliances 2nd edition. 4-14.
- Styrcula, L. (1994). Traction Basics. Orthopaedic Nursing, 13(2), 71-74.
- Trompeter, A. & Newman, K. (2013). Femoral shaft fractures in adults. Orthopaedics and
Trauma, 27(5), 322-331.
- Wilson, D., Curry, M. & Hockenberry, M.(2009). The child with musculoskeletal or articular dysfunction. In Hockenberry, M.J., & Wilson, D. Wong’s Essentials of pediatric nursing. (8th ed.). (pp 1106-1173). St Louis: Mosby.
- Whiteing, N. (2008). Fractures: pathophysiology, treatment and nursing care. Nursing
Standard, 23(2), 49-57.
Evidence table
The evidence table for this guideline can be viewed on the linked pdf.
Please remember to read thedisclaimer.
The development of this nursing guideline was coordinated by Holly Pannell, RN, Platypus Ward, and approved by the Nursing Clinical Effectiveness Committee. Updated December 2022.