Intrathecal baclofen (intra-thee-cal back-lo-fen) is a treatment used for children who have conditions that cause spasticity and dystonia, which means that their muscles are tighter than they should be.
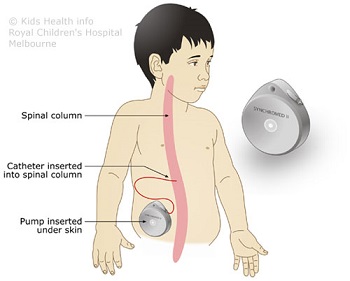
Baclofen is a medicine that helps the muscles to relax. Intrathecal baclofen is baclofen that is given into the space around the spinal cord. This is done via a pump that is permanently implanted inside your child's abdomen (tummy). The pump has a catheter (tube)
that goes to the spinal cord.
Why does my child need intrathecal baclofen?
Muscle tightness can stop your child from doing everyday tasks such as holding a cup, walking and sometimes even talking. Muscle tightness can cause pain in some children. Intrathecal baclofen can make it easier for your child to move their muscles, and it can relieve some of the
pain that muscle tightness causes.
Before your child's doctors decide if intrathecal baclofen is right for your child, many specialists will thoroughly assess your child. Your child may be seen by an orthopaedic surgeon, a neurosurgeon, different paediatricians, an occupational therapist, a physiotherapist and/or a nurse
consultant/coordinator.
There are many factors to consider when deciding who should have intrathecal baclofen treatment. Intrathecal baclofen does not suit every child or every family. You will need to live close to a medical centre that can manage the baclofen therapy and your child will need to attend
many appointments. All the people who help care for your child need to learn about baclofen and its side effects.
Trialling the therapy
Once your child's doctors and you have decided that intrathecal baclofen therapy might be right for your child, you will be booked in for a trial of the therapy, which will take place in hospital and involve a general anaesthetic. There are two types of trial:
- A bolus trial (also called a single-dose test trial) involves an injection of baclofen into the space surrounding your child’s spinal cord.
- A five-day catheter trial (also called a tube trial) involves an operation to have a tube placed in the spine. The tube is joined to an access port through which baclofen is delivered to your child’s spine.
The doctor will choose the most appropriate trial for your child. If your child responds well to the trial, you will have an appointment with a neurosurgeon to discuss the operation to insert the pump and how the pump works.
Intrathecal baclofen works differently for every child. Even though they have done a trial, your doctors cannot predict exactly how your child will respond to the therapy.
What to expect with an intrathecal baclofen pump
While your child is asleep (under a general anaesthetic), a neurosurgeon will implant the pump (about the size of a computer mouse) into your child's abdomen on one side near the hip bone. Joined to the pump is a long catheter, which is inserted into the space surrounding your
child's spinal cord. Your child will be in the operating theatre for about two hours.
A very small computer, called a programmer, tells the pump how much medicine to release. The baclofen will last from one to six months, depending on your child’s dose. When the medicine is running low, your child will have an appointment to have their pump refilled.
Complications of intrathecal baclofen therapy
Complications are rare, but it is important to know the possible side effects and what to do if something goes wrong. Side effects of the medication may include constipation, nausea and blurred vision. These usually settle over time, but if they continue, they can be managed in various
ways, which you can discuss with your child’s doctor.
Possible complications include:
- overdose of baclofen
- underdose (not enough) of baclofen
- infection of the site around the pump or tube
- infection of the wound from the surgery
- catheter kink (bent tubing), which prevents the flow of baclofen
- catheter break, causing a leak of baclofen
- catheter disconnection from pump, preventing baclofen from reaching spinal cord
- pump stops working properly.
Call your child's baclofen doctor or take your child to the hospital emergency department if:
- your child has a temperature higher than 38ºC
- there is redness or inflammation around the surgery site
- there is swelling around the pump area
- your child is drowsy or you can't wake them
- your child has slow breathing
- you think your child is too 'floppy'
- your child is unusually sweaty, itchy or grumpy
- your child’s muscles are tighter than usual
- you are concerned about the pump
- you hear beeping from the pump.
Always call an ambulance if you are worried about your child, even if you are unsure.
Care at home
Make sure you tell every medical person (doctors, nurses, radiologists, radiographers, pharmacists and other allied health professionals) caring for your child that your child has a baclofen pump. Every time your child is in any hospital for any reason it is very important that your child’s
doctors know that your child has an intrathecal baclofen pump. The doctors will need to consult with your baclofen team before carrying out any treatment on your child.
When planning a holiday, you must always consider how you will get help if you have concerns about your child's pump. You will need to have access to medical help that has knowledge of the pump, and you must know the emergency services number to call if you are travelling to another
country. Talk with your baclofen nurse or doctor if you are planning a holiday.
Key points to remember
- Intrathecal baclofen is a medicine that relaxes muscles. The medicine is given into the space around the spinal cord, using a pump that is implanted in your child’s abdomen.
- Intrathecal baclofen works differently for every child. Your doctors cannot predict exactly how your child might respond to the therapy.
- Your child needs a thorough assessment to decide if baclofen is suitable for your child and family, and will have a trial before going ahead with the treatment.
- Complications from an intrathecal baclofen pump are rare, but you must be aware of what can happen. Contact your baclofen doctor if you are concerned.
- Always tell every medical person caring for your child that your child has a baclofen pump.
For more information
Common questions our doctors are asked
How long will it take for my child to recover from the
operation to implant the pump?
Your child will have to remain lying down in bed for at
least 48 hours after the operation. After that, your child will be gradually
helped to sit up. If normally able to, your child can get out of bed
once they get used to sitting up again. If there are no complications and your
child is feeling well, they should be able to go home about five to seven days
after the operation. Your child's doctor will discuss this with you.
Can my child still go swimming, have spas and baths
once the pump is implanted?
Your child can usually go swimming and have baths six weeks
after the pump is implanted. This is provided the wound has healed and the
neurosurgeon has said it is OK to do so. Spa baths should be set to the
maximum temperature of 39ºC. Saunas should be avoided.
Can my child play sport with the pump in?
Your child should not play heavy contact sports as the pump
may be knocked out of place. Non-contact sports are fine. Your child
may need to wear some protective padding to cover the area around the pump.
Discuss this with your baclofen doctor.
How long will the pump last?
The battery on the pump lasts about five to
seven years. At this time your child will need another operation to
replace the pump.
Developed by The Royal Children's Hospital Developmental Medicine, Neurosurgery, Paediatric Rehabilitation, Orthopaedics and Physiotherapy departments. We acknowledge the input of RCH consumers and carers.
Reviewed October 2018.
This information is awaiting routine review. Please always seek the most recent advice from a registered and practising clinician.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit
www.rchfoundation.org.au.