Burn injuries
see also:
Key points
-
Burn injuries should be managed
as a trauma case requiring primary and secondary survey
-
Accurate Total Body Surface Area
(TBSA) estimation is essential for fluid resuscitation decision making – it
does not include epidermal burn
-
Optimal fluid
resuscitation is crucial – inadequate resuscitation contributes to
intravascular hypovolaemia and organ failure; excessive resuscitation
contributes to fluid creep with extension of the burn wound and systemic oedema
causing cardiorespiratory compromise, intra-abdominal and limb compartment
syndrome
-
Managing pain and preventing
complications are an important part of burn assessment and patient care
-
Close supervision of children at
all times will help prevent burns
-
Some minor burns will be able to
be managed at non- Paediatric
Burn Unit
-
Burn management requires
multidisciplinary approach including
psychosocial care which addresses the significant impact a burn can have on a
child and their family
Background
Burns
are common in children. Burns range from minor wounds that can be managed in an
outpatient setting to moderate wounds,
requiring transfer to Paediatric Burns Unit and surgical management,
through to major wounds with associated traumatic injuries requiring retrieval
to Paediatric Intensive Care and Burns Unit.
Scald burns in young children are the most common type of burn. Most
burns are mild and can be managed in a community setting, however major burns
require prompt and h
Burns in children are different to those in adults due to their
differences in their physical attributes, developmental abilities and emotional
maturity.
An accurate assessment of a burn depth is difficult, especially
early post injury. All burn injuries should be considered part of a trauma assessment,
and non-accidental inflicted injury should be considered.
Epidemiology
Burns are a significant cause of morbidity and mortality in
children, and a common cause for hospital admission.
Most burns occur in the home, predominantly in the kitchen. Most burns
are not very severe and are small; <10% total body surface area (TBSA). Most
hospitalisations are short (<1 day), though many burns require community
care and some for prolonged periods of time.
Globally,
nearly 96, 000 children under the age of 20 were fatally injured as a result of
a fire-related burn in 2004[i]. Within all countries burn risk correlated with
socioeconomic status. Regional
differences in burns exist; in
2018 children under 5 years
of age in African Region have 2 times incidence of burn deaths than their
worldwide counterparts; boys under 5 years
of age from low-middle income countries of the Eastern Mediterranean Region are
nearly twice as likely to die from burns as similar boys from
the European Region; burn injuries requiring medical care is almost 20 times
higher in Western Pacific Region compares to the Region of the Americas[ii].
In the developing world open cooking fires are a major source of
burns; commonly hand burns. Burn injuries to hands are particularly disabling due
to impaired functionality and lack of adequate rehabilitation/assistance
devices in the developing world - even a small hand burn can affect an
individual’s ability to perform activities of daily living independently and
perform physical labour for a family’s livelihood.
The death rate in low-income and middle-income countries is eleven
times higher than that in high-income countries – 4.3 per 100 000 as compared
to 0.4 per 100 000[i].
The type and cause of paediatric burns are related to the age and
developmental stage of the child. Young children are most likely to incur a burn
injury: 70% paediatric burns occur in <5 year old children. Infants have the
highest death rates. The highest rates of hospital admission are of children
<4 years old which correlates
Males are over represented in all age groups for burns and the
gender imbalance increases with age. From 10-14 years of age males have a sharp
increase in burn injuries from exposure to highly flammable liquid (eg petrol).
In Australia, burn
and scald injuries are especially high for infants and children <4 years of
age. Hot drinks, food, fats and
cooking oils cause more than half of the scalds in this group, with face,
trunk and arm burns being the most common sites of injury. Aboriginal
and Torres Strait Islander people have higher rates of burns in all ages
compared to other Australians, and whilst
all Australians have the highest rate of burns in less than 4 year olds
Aboriginal and Torres Strait Islander children of this age are more likely than
other Australians to be burned (174 cases per 100,000 compared
to 45 cases per 100,000
population)[iv].
Other
risk factors for paediatric burns include poverty, overcrowding, lack of
safety measures or adequate parental supervision including young girls being
given a household role of cooking. Children with some underlying medical conditions are also at
increased risk of burns such as epilepsy and physical or cognitive
disabilities. Children
are at risk of burns from neglect and inflicted burns as child abuse.
Pathophysiology
A burn is a thermal injury
resulting in a wound characterised by an inflammatory reaction leading
initially to local oedema from increased vascular permeability, vasodilation
and extravascular osmotic activity. It is caused by direct effect of the burn
agent on microvasculature and resultant chemical
inflammatory mediators.
A burn is an injury with both
local and systemic responses. There are three major types of burn: thermal,
electrical and chemical. Changes in tissue after the burn
trauma are very important. In large burns fluid loss from damaged tissue causes
decreased plasma and increased haematocrit with decreased cardiac output which
contributes to widespread cellular hypoperfusion resulting in multisystem
damage.
Local response
Zone
of coagulation – this is the primary site
of injury and the site of maximum damage. This zone comprises irreversible
tissue loss due to exposure to heat, electricity and/or chemicals.
Zone
of stasis – this surrounding zone has decreased
tissue perfusion and is a penumbra of potentially salvageable tissue. Good quality
first aid and burn resuscitation aims to reverse ischaemia and minimise the size
of this zone. Risks to increasing size include increased depth of burn, prolonged
hypotension, infection and oedema. This zone changes making initial burn
assessment difficult. The full extent of injury is only apparent after several
days.
Zone
of hyperaemia – this outer zone comprises
and area with increased perfusion and will
recover unless there is an additional insult.
Skin loss decreases the
body’s ability to preserve heat and water and act as a barrier to prevent
infection. Resuscitation and treatment aim to correct these consequences.
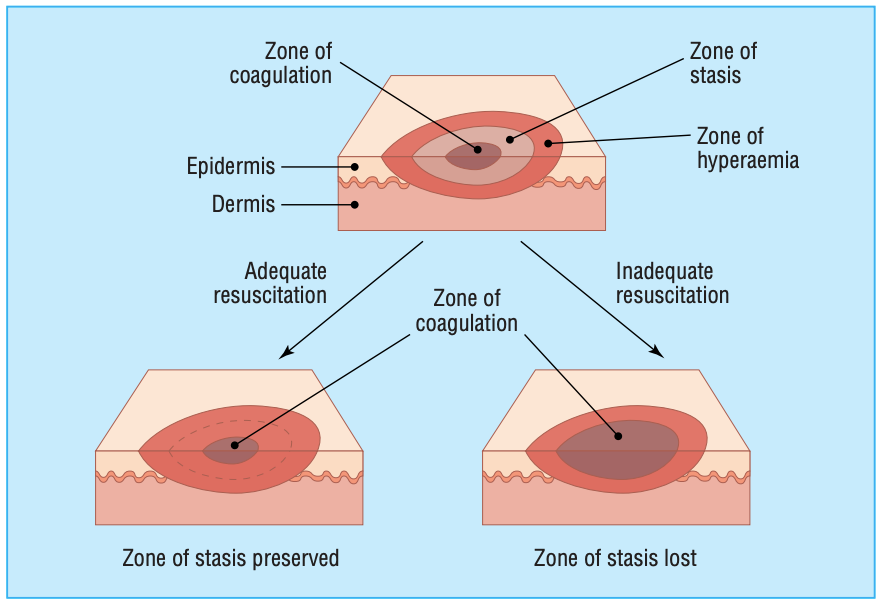
Figure 1: Jackson's Burn Wound Model, 1947. (Reproduced
with permission: Figure
2 Hettiaratchy
S, Dziewulski P. ABC of burns: pathophysiology and types of burns British Medical
Journal.
2004;328(7453):1427–1429Ds).
Systemic response
Once TBSA >30% a systemic
inflammatory response will occur.
The renal and hepatic systems are susceptible to dysfunction due to
resultant fluid and protein loss and a decreased blood volume. In
major burns the fluid state of the patient must be carefully managed. Adequate
and timely fluid resuscitation due to excess losses from the burn are crucial
in curbing the extent of systemic dysfunction from this mechanism. Similarly,
over resuscitation with excess fluid can have detrimental effects on
cardiorespiratory function and contribute to compartment syndrome in the limbs
and abdominal cavity.
A widespread inflammatory response also occurs as the result of a burn injury
with release of catecholamines, vasoactive mediators and inflammatory markers
which can trigger a systemic inflammatory response syndrome (SIRS) resulting in
multiple organ dysfunction syndrome (MODS).
Figure 2: Systemic response to burns
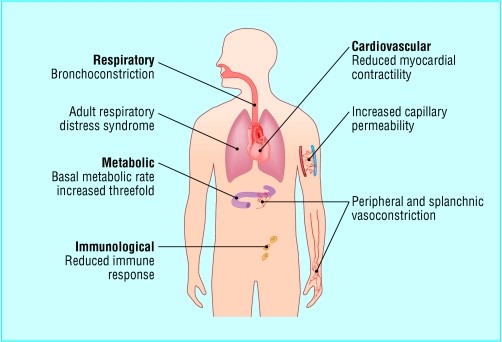
Reproduced with
permission. (Figure 3 Hettiaratchy S, Dziewulski P. ABC of burns:
pathophysiology and types of burns British Medical Journal.
2004;328(7453):1427–1429[v]).
SIRS also contributes to
immunosuppression rendering a patient more susceptible to bacterial infection
and sepsis. The systemic
response worsens initial organ damage caused by shock and reduces the body’s
ability to fight infection; this leads to an increased risk of sepsis which
further triggers inflammation, immunoparesis and infection.
Following a burn injury, a hypermetabolic state ensues where catabolism
increases and anabolism decreases resulting in loss of muscle and bone mineral
density. Wound healing may also be affected. This hypermetabolic state is
sustained despite wound closure. Protein breakdown continues 6 – 9 months after
the initial burn making nutritional support to sustain lean body mass and
promote wound healing of crucial import. Bone growth can be delayed for 2 years
after a burn injury in children.
How children are different to adults
Children have thinner skin
than adults, therefore the time to burn, or the
energy required to cause a burn is less. This means that a
burn agent at any given temperature, will
cause a deeper burn, at a faster rate,
in a child compared to an adult.
Young children are at risk of hypothermia, especially during
initial cooling of the burn and from increased evaporative loss due to their
larger surface area to body mass ratio.
Children have an increased blood volume relative to their mass
therefore fluid resuscitation needs to accommodate for this: large volumes per
unit body weight are required compared to adults. Small children are more
likely to become hypoglycaemic and
The risk of airway compromise in children following inhalation
injury is greater due to a smaller airway opening and greater risk of closure
from oedema.
The systemic inflammatory response in children tends to be
stronger with more vulnerability to their effects, including am increased
susceptibility to the resultant hypermetabolic state.
As children are still growing their need for skin growth and
elasticity to accommodate this growth complicate wound and scar management.
Assessment: History of burn
Time of
injury
Mechanism of injury,
including circumstance for specific pattern of burn
- Scald: estimate temperature and ask about the nature of
the liquid
- Recently boiled water?: likely to be close to 100 degrees Celsius,
- Hot drink with milk?: likely to be a cooler than recently boiled water
- A solute in the liquid?: eg boiled rice – raises the
temperature of liquid
- Viscous liquid? more viscous fluids result in more severe burns as they remain in contact with skin for longer
- Common causes include scalds from hot drinks(tea/coffee), kettles, bath, noodles
- Contact: estimated temperature and nature of the surface
- Common causes include irons, hair straighteners, exhausts, campfires,
metal clips on car seats
- Radiant:
- Common causes include sunburn - this may be associated with neglect. Some burns sustained during house fires or bush fires can be due to radiant heat.
- Friction:
- Common causes include falling on, or touching, moving treadmills, or road rash after a motor vehicle crash
- Flame / explosion:
- ask about the product
that burned/exploded: to predict temperature
and predict secondary effects
- ask about the location where the patient was exposed: indoor flame injuries are more likely
associated with inhalation injury as compared to those in open spaces; indoor explosions may be associated with greater traumatic injuries
- ask about the duration
of exposure: to predict extent of burn
- Common causes include flash burns after pouring accelerants (kerosene, petrol) onto BBQ's / bonfires, as well as in house fires
- Electrical:
- Low voltage (<1000V - typically domestic), high voltage (>1000V - often industrial) and lightening have different patterns of injury and complications
- Type
of current: alternating current
(AC) or direct current (DC). DC
typically provides a single convulsion or contraction usually propelling person
away from source, whereas AC causes repeated
convulsions and cardiac arrhythmias such as VF and is
considered more dangerous; a
larger magnitude of DC is required to cause injury than AC
- Was there
a flash or arcing: more likely to cover a
large surface area and be more superficial,
time and duration of contact: to predict severity of burn
- Common cause include young children chewing on electrical cords
- Chemical:
- ask about the type of product: to
predict extent of burn and secondary effects (alkali vs acid burns)
-
look at clothing for stain colour
- Cold:
- direct contact with cold surface or exposure
(frostbite)
- Inhalation:
- common causes include inhalation of hot gases during a house fire, or flame burns to the face. May be of greater consequence if they have occurred
in enclosed space
First aid
- Time started (was it within 3 hours)
- Agents used - cool running water vs less effective agents (standing water, cold compress, ice, home remedies)
- Duration - was it at least 20mins of cool running water?
- If clothes and jewelry were removed
- Decontamination method (for chemical exposure)
Any
circumstances to implicate co-existing non-burn injuries
Any
circumstances to implicate non-accidental injury or vulnerable child
Tetanus
status
Assessment: Primary survey
Like all traumas,
paediatric burn assessments require an initial
primary survey with the aim of identifying and managing immediate life threats:
do not be distracted by the burn injury until all
immediate life threats have been addressed. The list below indicates some of the key examination findings to look for during the primary survey. These findings may signal the presence of an immediate life threat requiring management during the primary survey. Do not neglect to apply personal protective equipment (PPE) which is especially
important to protect health care workers where the patient
has a chemical burn.
Examination
- Signs of
airway burn/inhalation injury: stridor, hoarseness, black sputum or
respiratory distress, singed nasal hairs or facial swelling
- Sign of
oropharyngeal burn: presence of soot in mouth, intraoral oedema and
erythema
- Significant
neck burn
Management
- If suspicion of
airway burns apply high flow oxygen
- Protect the cervical spine with
cervical spine motion restriction if there is associated trauma
Breathing
Examination
- Signs of inhalation injury as above
- Full thickness and/or circumferential
chest burns
- Tension pneumothorax
secondary to an explosion / associated trauma
Management
Circulation
Examination
- If early
shock is present, consider causes other than the burn
- For
circumferential burns check peripheral perfusion (and
Management
- IV or IO access (preferably 2 points of access)
- Consider IV fluid resuscitation
Resuscitative Fluid management in burns >10% TBSA
- This is required to compensate
for excess fluid losses in the first 24 hours after burn
- Calculate
requirements from time of the burn, not time of presentation
- Calculate
fluid volume using Modified Parkland Formula (MPF) (below)
- Hartmann’s
Solution is the fluid of choice - if unavailable, use 0.9% N saline
- Glucose in maintenance
fluid is required for children <20kgs
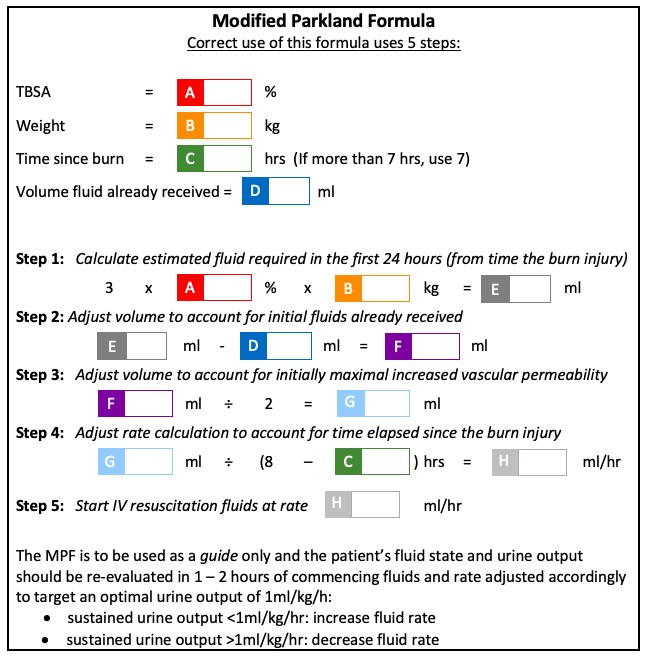
Patients with delayed fluid resuscitation, electrical conduction
injury and inhalation injury have higher fluid requirements. Discuss with
specialist team.
For burns >10% TBSA
- In dwelling catheter (IDC) is
recommended to monitor urine output
- Nasogastric tube (NGT) is recommended with
nil by mouth state to manage an initial gastroparesis associated with burns and
later to ensure adequate caloric intake in the coming days
Fluid creep
Fluid creep refers to excessive fluid administration to
patients with burns. Adequate fluid resuscitation is a crucial part of managing
children with major burns; if provided early it restores intravascular volume
and maintains tissue perfusion both to the burn wound which avoids extension of
the injury into the zone of stasis, and to the body which evades more
widespread complications such as renal failure and reduces mortality[iv].
The Modified Parkland formula above should be used as an
initial guide to fluid resuscitation but the ongoing fluid replacement in a
child with a major burn must include regular and in-depth fluid assessment
beyond the urine output alone. If a child with a major burn is overhydrated it
can lead to the development of systemic interstitial oedema which independently
cause complications such as limb ischaemia from increased limb compartment
pressures, renal failure from intra-abdominal compartment syndrome and
respiratory failure from airway swelling and trauma.
To avoid fluid creep, avoid over estimation of TBSA,
include all resuscitation fluids received by patient when calculating the
appropriate resuscitation volume. If the fluid volumes appear greater than the
predicted requirements from the modified Parkland formula alternative causes
should be sought and managed. A fluid assessment of a patient with major burns
includes not only the urine output but clinical fluid examination, biochemical
markers, ventilatory parameters and end organ perfusion markers.
Disability
- Neurological
state: GCS and pupillary response
- If suspicion of carbon monoxide poisoning
apply high flow oxygen
- Neurovascular
status if limb involved (asses with doppler ultrasound if necessary) –
requires elevation of the effected limb and hourly neurovascular
observations
Exposure
Fully expose the patient in order to assess the extent of injury in terms of:
- the percentage of Total Body Surface Area (TBSA) that is affected by the burn and
- the burn depth
Check the patient's temperature (it is easy for small children to become hypothermic after cooling). The principle is to keep the patient warm, but the burn cool. The 20 mins of cool running water during first aid can be split into shorter sessions, with warming of the patient in between, as long as all the cooling occurs within the first 3 hours.
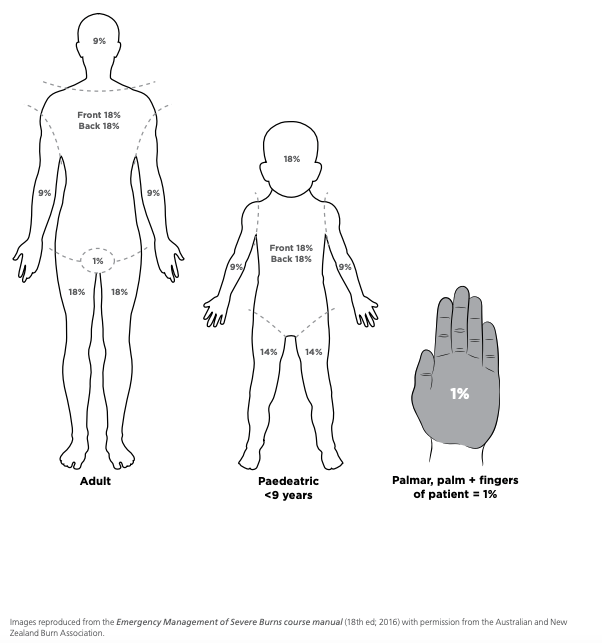
Assessment of TBSA
- Expose whole
body - remove clothing and log roll to visualise posterior surfaces
- Keep patient
warm
- Estimate burn
area with the Lund & Browder Chart
- Do NOT include area with epidermal burn (erythema only)
- TBSA
determines need and volume of fluid resuscitation, hospital admission and
transfer to Paediatric Burns Unit
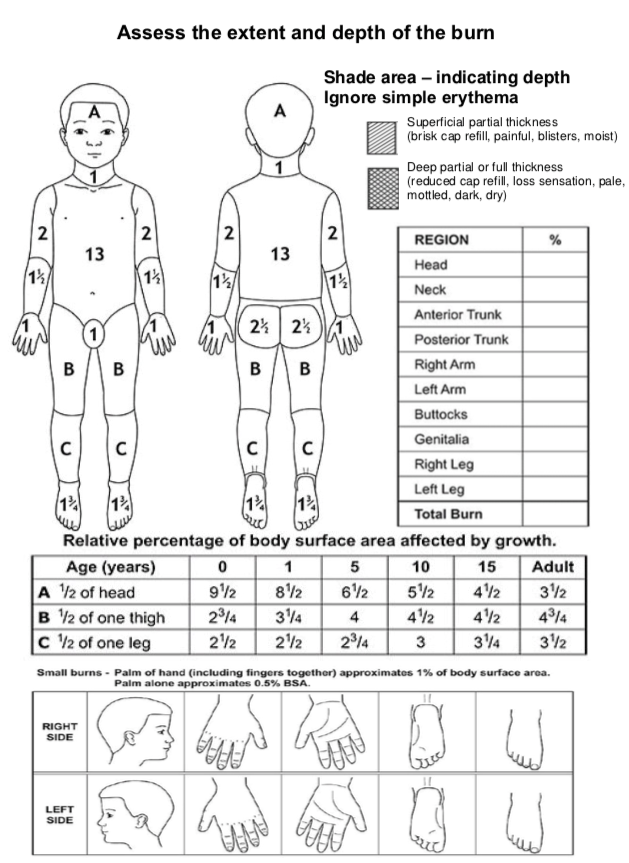
Reproduced
with permission. (Appendix
1. CHQ-GDL-06003
– Management of a paediatric burn patient within the Pegg Leditschke Children’s
Burns Centre. Children’s
Health Queensland Hospital and Health Service[vii]).
Assessment of burn depth
- Burns are
dynamic wounds: it is difficult to accurately estimate the true depth and
extent of the wound in the first 48-72 hours
- Burns are
described as epidermal, dermal (superficial/mid/deep) and full thickness
- Speed of
capillary refill is a good indicator of burn depth, although burn wound
evolution results in increasing depth therefore examination can change over
time
-
Most burn wounds are not a homogenous depth
|
Classification
|
Depth
|
Colour
|
Blisters
|
Capillary Refill
|
Sensation
|
|
SUPERFICIAL
|
Epidermal
|
Red
|
No
|
Brisk
|
Present
|
|
Superficial Dermal
|
Pale Pink
|
Present
|
Brisk
|
Painful
|
|
Mid Dermal
|
Dark Pink
|
Present
|
Sluggish
|
+/-
|
|
DEEP
|
Deep Dermal
|
Blotchy Red
|
+/-
|
Absent
|
Absent
|
|
Full
Thickness
|
White
|
No
|
Absent
|
Absent
|
Assessment: Other considerations
Consider
co-existing injuries
Especially in motor vehicle crashes, blasts/explosions, electrical
injuries or jumps/falls from significant heights.
Consider
alternate diagnosis: scald burn mimics
- Staphylococcal
Scalded Skin Syndrome
- Blistering
distal dactylitis – caused by group A strep
- Stevens
Johnson Syndrome/Toxic Epidermal Necrolysis – follows medication use
- Hair tourniquet – distal erythema and swelling can mimic a
peripheral burn
Consider non-accidental injury (see
below)
Burn Wound Management
Like all traumas paediatric burn injuries require recognition
and management of all injuries following the primary and secondary survey.
Acute
management of superficial burns with
erythema only
- Can be treated without dressing
- Infants who show a tendency to blister or scratch,
a protective, low-adherent dressing with crepe bandage may be helpful.
Acute
management of minor burns (isolated, <10% TBSA)
- Analgesia may be required for assessment and
initial dressings
- Consider sling and splinting for more
extensive upper limb burns
- Dressings that can remain in situ for 3-7 days
are recommended for partial thickness burns
- The depth of a partial thickness burn may only
be declared after 7-10 days
- De-roof/debride if blister is large or
overlying a joint
Acute
Management of major burns (>10% TBSA) or complex burns
FACADE
=
First aid, Analgesia, Clean, Assess, Dress, Elevate
First
aid
- Remove jewelry and clothing in contact with burn source
- Do not remove bitumen stuck to a burn
- Cool affected area as soon as possible
(within 3 hours from time of burn) for a total of 20 minutes with cool running
water
- If cool running water is unavailable,
other options include: frequently changed cold water compresses/towels,
immersion in a basin, irrigation via an open giving set
- Never apply ice and avoid use of
hydrogel burn products
- Do not use butter, sugar, oil,
toothpaste, potato, egg white or other traditional remedies
- Prevent hypothermia: cool the burn not
the child
- Remove wet clothes/dressings after
initial cooling
- Try to keep child otherwise warm
- Cover the wound and the child after
assessment
- When possible, warm the intravenous
fluids and the room
- Cover burn with plastic cling film lengthways
along the burn (do not wrap circumferentially) - this helps maintain burn wound
moisture and protect exposed nerve endings which contributes to pain management
- Do not apply plastic cling film to
face (use paraffin ointment)
- Do not apply plastic cling film to a
chemical burn
- Discuss Chemical burn decontamination
with Poisons Information (Tel: 131126)
- Appropriately consented photos of
burns should accompany a referral if possible
Analgesia
- Burns are painful and often require strong
analgesia: appropriate initial choices include intranasal fentanyl or IV
morphine
- Utilise
multimodal analgesia including cooling, cling film, parental presence/support
to alleviate anxiety and distraction
- Analgesia is required
especially during cooling, dressing and mobilisation
Clean
- Limit debridement to wiping away
clearly loose/blistered skin
- De-roof
blister (with moist gauze or forceps and scissors) if
>5mm or crossing joints
- Clean
burn wound and surrounding surface with saline or water or 0.1% Aqueous
Chlorhexidine on gauze (flannel if no gauze)
- Pat dry
Assess
- Assessment
of burn injury TBSA and depth as above
- Take
photos with appropriate consent
Dress
- Apply appropriate occlusive non-adherent dressing; if these
products are not available, refer to local Burns service for alternative
options
If
there is anticipated delay or time until definitive care, consider use of
multiple layer non-adhesive paraffin antiseptic dressing.
|
Location
|
Depth
|
Dressing
|
|
Facial
and perineal burns
|
Epidermal
or superficial dermal
|
Apply
white soft paraffin twice daily after cleaning face
Chloramphenicol
ointment to eye and ear burns
Perineal
burns are at risk of contamination – after bowel action, area should be
cleaned with soapy solution; consider catheterisation; 4% chlorhexidine skin
wash
|
|
Mid
or deep dermal
|
Consider
silver-impregnated dressing (discuss with Burns service)
|
|
Other
body regions
|
Epidermal
|
May
not require dressing
Consider
covering with protective, low-adherent dressing for comfort
|
|
Mid
or deep dermal
|
Dressing product used depends on the expected
duration required before removal or wound review
In general:
- for small, superficial partial thickness burn
wounds use a low adherent dressing then crepe bandage/tape
- for more extensive or deeper partial thickness
burn wounds use a low adherent silver dressing then crepe bandage.
|
Elevate
- Elevate
burn by positioning and adjuncts (pillows, towels, slings)
- Elevation
aids management of oedema to minimise poor tissue perfusion and improve wound
healing
- Do
not apply tight circumferential bandages
- Elastic
compression is helpful (Tubigrip)
- Encourage
functional activity of effected body part
Operative
management
Superficial
wounds should heal by regeneration within 2 weeks and need only cleaning,
dressing and review to optimise healing. If a burn has not healed within 2
weeks it should be referred for assessment and may require surgery.
Deep
partial thickness or full thickness burns are likely to require operative
management which includes excision of the deep burn and skin grafting within
5-10 days to expedite healing and minimise scarring. Sometimes artificial
dermis is used as a bridge to skin grafting. Skin grafts can be autografts or allografts.
Grafting consists of 4 steps
- The removal of injured tissue
- Selection of a donor site, an area from
which healthy skin is removed and used as cover for the cleaned burned
area
- Harvesting, where the graft is removed
from the donor site
- Placing and securing the skin graft over
the surgically-cleaned wound so it can heal
For large burns multiple operations may be
required to complete the grafting process.
Investigations
|
Major burn
(≥10% TBSA)
|
Haemoglobin,
electrolytes, BGL, group and hold, VBG
|
|
Suspected
inhalation injury
|
ABG for
carbon monoxide, lactate, cyanide level
|
|
Electrical
burn
|
Cardiac
monitoring, urine myoglobin
|
Special considerations
Circumferential
deep burn
(deep dermal or full thickness)
Elevate part of limb distal to
burn to minimise swelling and oedema. Assess and monitor for neurovascular compromise of tissue distal
to the burn; escharotomy may be
required.
Limb
burns
Elevate the limb and monitor perfusion distal to burn.
Hand
burn
Hand burns in children are common
due to the inquisitive nature of children and their developing motor skills.
Assessment and management of hand burns in children are as above. Special priority
must be given to early active rehabilitation to optimise hand function. See
Rehabilitation below.
Treadmill
injury
Exercise equipment is becoming commonplace in homes. Children
should not have access to treadmills at any time: switch off power at wall and
unplug, keep behind closed toddler gate or locked door. A friction injury
caused by a treadmill is a type of burn, which should be assessed and treated
as a burn. Friction injuries from treadmills are commonly on children’s hands
and cause serious burns often requiring surgical intervention and lengthy
rehabilitation.
Head
and neck burns
Nurse head up to reduce swelling and oedema.
Ocular
burns
Signs of ocular burns include
blepharospasm, tearing and conjunctivitis. All facial burns should have
ophthalmological assessment including visual acuity, external ocular exam and Fluorescein
2% eye drops to assess for corneal damage. Full thickness facial burns propose
high risk of ocular damage.
Both thermal and
chemical corneal burns threaten vision; alkalis penetrate deeper and have greater
potential for serious and delayed burns.
Treat all ocular chemical burns with
copious irrigation using 0.9% NaCl as soon as possible. Ensure the
unaffected eye is uppermost during irrigation of effected eye to avoid further
contamination. Use topical anaesthetic on effected eye for
analgesia and to aid tolerance of irrigation.
- Irrigate until all chemical/alkali washed out (test
with pH strip prior and post)
- Up to 1 hour with acidic contamination
- Up to 2 hours with alkaline contamination
Use topical Chloramphenicol to prevent
secondary infection.
Urgent paediatric ophthalmology review is
required to for:
- All
ocular burns
- Full
thickness eye lid burns
- Facial
burns with inability to close eyelids
Electrical
injuries
Degree of injury is related to the voltage of the electrical
source. Electrical injuries can be associated with other injuries: consider
spinal precautions. Electrical injuries can also cause cardiac dysrhythmias -
consider 24 hours ECG monitoring. Monitor and manage elevated CK, urine haemoglobin/myoglobin
and haemochromogen. Monitor for
compartment syndrome.
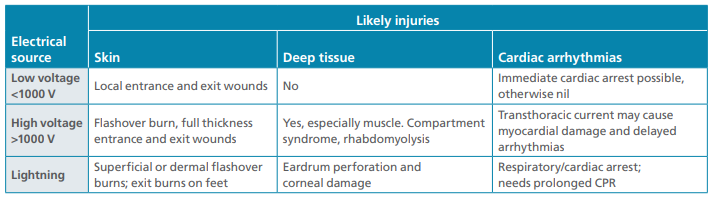
Reproduced
with permission. Clinical Guideline, Statewide
Burn Injury Service – NSW Burns transfer guidelines (4th edition) Page 12
Electrical burns: table Overview of electrical injuries © Copyright -
Agency for Clinical Innovation 2020[viii]
Electrical
injury: labial artery erosion
Children can suck on or chew through power cords, or can chew on
damaged/frayed power cords, resulting in an electrical burn. Even low voltage
electrical burns can be serious causing deep injury with muscle tendon and
vessel involvement. Electrical burns occurring at the edge of the mouth can be
associated with acute or delayed (up to 21 days) labial artery involvement and
significant haemorrhage.
Chemical
burns
Chemical burns are
caused by caustic agents:
- Acids cause coagulative necrosis
of the superficial tissue eg toilet cleaner
- Bases cause liquefactive necrosis
and have a higher capacity for injury, including deep to the initial wound and
ongoing injury process despite removal of base eg laundry detergent
- Organic solutions cause injury by
dissolving the lipid membrane
- Inorganic solutions cause injury
by tissue denaturation
First aid of chemical burns with
irrigation of cool running water is extremely important and is often forgotten. Personal
protective equipment for first aid givers should be worn (gloves, mask, gown,
eye protection. Ensure contaminated clothing is removed and brush any powdered
agent off skin onto a collection sheet to be disposed of appropriately.
Irrigate from the top of the wound down to the floor with
appropriate drainage so contaminated water does not cause further injury.
Consider systemic symptoms from metabolic and electrolyte
disturbance from absorbed agent.
Chemical burn: oesophageal injury
Many harmful
agents are found in everyday households eg toilet cleaner, bathroom cleaner,
hair products, laundry and dishwasher detergents, batteries, drain and oven
cleaners. Ingestion of caustic agents can lead to oesophageal burns, strictures
and perforation. Children with significant injury may have no-mild symptoms
only. Symptoms include dysphagia, drooling, chest/abdominal pain, refusal to
eat, respiratory compromise. The injury tends to worsen over time.
Tetanus
prone wounds
Consider if prophylaxis with vaccination or tetanus immunoglobulin
is required.
Inhalation
injury
These occur with flame burns in
enclosed spaces. Direct inspection of the oropharynx should be performed on
arrival and consideration of early intubation by an experienced airway specialist.
Inhaled smoke is cool upon
reaching the lungs but products of combustion are irritating leading to
bronchospasm, inflammation and swelling. This predisposes an individual to
atelectasis and pneumonia, and can be worse in asthmatics. Patients may require
non-invasive positive pressure ventilation or invasive ventilation and airway
toileting.
Carbon monoxide and cyanide
poisoning
If suspicion of associated Carbon
monoxide (CO) poisoning or cyanide poisoning liaise early with Paediatric Burn
Unit, Critical Care and Poisons Information (Tel: 131126).
Carbon monoxide is a toxic gas
inhaled during a fire, such as a patient enclosed in a house fire. Carbon
monoxide binds very strongly to haemoglobin and intracellular proteins
contributing to intracellular and extracellular hypoxia. Toxicity is dose
dependant involving no or few symptoms through to cardiovascular compromise
with seizures and death[ix].
Symptoms include:
- Gastrointestinal: nausea,
- Respiratory: dyspnoea, respiratory failure
- Cardiac: syncope, cardiovascular compromise
with myocardial ischaemia
- Neurological: dizziness, vertigo, ataxia,
visual disturbances, headache, confusion and decreased conscious, seizures
Pulse oximetry cannot differentiate between haemoglobin and
carboxyhaemaglobin so will not read low even when a patient is hypoxic. Blood
gas will show metabolic acidosis and raised carboxyhaemaglobin. These patients
require 100% oxygen and may require ventilation. Unborn foetus can be affected
by toxicity: specifically discuss care of pregnant women with specialist teams.
Cyanide
is a potentially lethal toxic poison that is produced in gaseous form from burning natural and synthetic fibres such as plastics and
wools such as occurs in in domestic/industrial fires. Cyanide poisoning occurs
from inhalation of this gas and often occurs with carbon monoxide poisoning. Toxicity
is dose dependant and incudes multisystem involvement[ii].
Initial symptoms include:
- Gastrointestinal: nausea, vomiting
- Respiratory: tachypnoea, dyspnoea
- Cardiac: tachycardia, hypertension
- Neurological: headache, decreased conscious
state, seizures
More severe symptoms include end organ damage
form anaerobic metabolism with associated hypotension, bradycardia and
cardiovascular collapse, respiratory depression and reduced GCS.
Blood gas will show metabolic
acidosis with high lactate, serum level cyanide should be taken.
Treatment includes ABC resuscitation, high
flow oxygen and administration of antidote hydroxocobalamin then sodium thiosulfate.
Frostbite
Frostbite is a type of burn
injury to the skin and underlying tissues by freezing. It most commonly effects
the extremities and can be divided into superficial or deep. It can occur
through exposure to cold-weather conditions or direct contact with cold ice,
liquid or metal. Minor frostbite injuries can be managed with simple first aid
involving analgesia and rewarming followed by simple wound care. More serious
injuries may require review with a burns service for more intensive wound care
management.
Non-Accidental Injury
Non-accidental burn injuries can occur in the setting of neglect
or physical abuse. Inflicted burn injuries are under recognised; it is
difficult to estimate the incidence. They effect children of all ages and incur
significant mortality and morbidity[iii].
Concerning
features on history
- Inadequate supervision
- Delayed presentation
- Changing mechanism
- History that is incompatible with
age/development of child and injury
- Mechanism that is incompatible with
injury
Scalds are the most commonly inflicted burn injury. Certain
locations or patterns of burn are more suspicious for an abusive cause:
- Hands
- Feet
- Genitals
- Buttocks
Burns
concerning for inflicted injury
Submersion burns
- Circumferential
- Symmetrical
- Uniform depth
- No splash marks/satellite burns
- Buttocks, perineum, extremities
- Sparing on buttock cheeks “donut sign”
(held down on bath), in flexures (groin, knees) and abdominal creases (as trunk
is flexed forward when child tries to protect them self)
- Glove and stocking distribution for
limb submersion
Contact burn
- Very young child
- Patterned burn >1 lesion
- Cigarette burn: clustered, sharply
demarcated, ~1cm punched out, deep, circular, hands and feet
- Iron
- Lighter – classic “smiley face”
patterned burn
- Trunk or buttock
- Bilateral foot sole burns from being
held on hot pavement
What
to do if you are concerned a burn injury was caused by neglect or abuse
- Take clear photographs with consent
for the patient’s medical record ensuring you capture the edges of all burns
and presence/absence satellite lesions, clearly document age of the burn as
child protection can use burn healing to help ascertain the cause and timing of
the injury (consider image with tape measure if available for sizing)
- Report suspected abuse to Department
of Health and Human Services
- Consider a “scene investigation” – a
formal assessment of the scene of injury performed by Police or Child
Protection to provide valuable information regarding the environment where the
injury occurred
- Carefully assess the child for other
evidence of inflicted injury (bruising, fractures, abusive head trauma,
injuries from shaking/impact)
- Consider referral to local paediatric
forensic service
Consider consultation with local paediatric team when
- Suspected non accidental injury,
self-inflicted burns or assault
- Multiple co-morbidities
- Concern regarding social situation or
dressing compliance
Consider transfer to a Paediatric Burn Unit when
Child requiring care beyond
the comfort level of the hospital
Following burns:
- >10% TBSA
- All full thickness burns
- Special areas: face, ears, eyes, neck,
hands, feet, genitalia, perineum or a major joint, even if <10%
- Circumferential
- Chemical
- Electrical
- Associated with trauma and/or spinal cord
injury
- All inhalation/airway
- Children <12 months
Discharging a patient with a burn wound
Minor burns may be discharged at initial presentation and referred
to outpatient burns follow up of local service with 1-2 visits per week
initially.
Moderate or large burns or patients with multiple injuries will
have required in patient admission or transfer to a Paediatric Burns Unit and
may require Paediatric Intensive Care. As part of acute care – once discharged
will require multiple follow up appointments as an outpatient.
The ability of a family to provide adequate care for a child with
a burn and attend appointments should be taken into account when deciding the
child’s disposition. These include geographical isolation and concern for
social welfare of child; delayed presentation, suspicion of non-accidental
injury or concern family will not care for wound or attend appointments.
Follow up
Burns can
evolve over time. Consider a follow up within 3 days of initial presentation to
reassess depth, monitor healing and determine ongoing management. On
reassessment referral to Paediatric Burn Unit is necessary:
- Depth is unclear after 3 - 5 days
- Slow to heal – poor progression at 5-7 days
Post Acute Care of Burns
The type of care a child requires depends on the type, depth and
extent of burn, involvement of burn in special areas premorbid health,
additional injuries and psychosocial situation (eg concern of neglect or non-accidental
injury). A multidisciplinary team is required.
Burn
Dressings
The burn wound dressing will depend on the type and severity of
the burn wound.
Principles of burn wound management
- Relieve pain
- Maintain a moist wound environment
- Keep wound clean
- Prevent/minimise infection
Daily dressing change is not advised. Timing of dressing changes
depends on the product used. Dressing advice can be obtained from your local
Paediatric Burns Unit.
Many burn dressings are available. Dressing choice will depend on
what is stocked at your local service. Below is an example of a safe and
effective initial dressing.
Primary Dressing/Contact Layer
Application of silver dressing as per local methods. A typical
burn dressing may include 7 day Acticoat (alternatives include 3 day Acticoat,
Mepliex Ag, Aquacell Ag).
Secondary Dressing/Fixation
Provides a final layer to absorb exudate and secure primary
dressing/contact layer in place (Melolin, Hyperfix).
Analgesia
Pain management is an important part of paediatric burn care –
uncontrolled stress and pain contribute to poor healing. All procedures should
be performed with adequate sedation and analgesia. Multimodal analgesia is
often necessary to achieve adequate analgesia. Consult local pain service for
advice or opioid infusions/patient controlled analgesia as required for in
patients with severe burns. For minor burns including those managed in the
community consider nitrous oxide or intranasal fentanyl during burn review and
dressing changes. Consider additional analgesia requirements for children who
have had previous distress during dressing changes or ongoing anxiety.
Utilisation of child life therapy, music therapy teams and non-pharmaceutical
distractions (eg iPad, breast feeding, reading, limiting child’s ability to
watch wound care) should complement chemical analgesia and sedation.
Preventing
Infection
Standard infection control measures apply to children with burn
injuries
- Staff and visitors must perform hand
hygiene
- Staff must wear gloves for dressing
changes
- Visitors who are unwell should not
visit the patient
Burns >10% TBSA require additional infection control measures
which aim to limit child’s exposure to bacteria via isolation and limiting
transmission via contact – follow local Paediatric Burns Unit infection
precautions.
Nutrition
Nutrition is an important part of burns care. Children have an
increased metabolic requirement, and increased nutritional requirement for
growth, limited energy reserve and an increased body surface area to mass ratio
compared to adults.
Children who are unable to drink due to facial burns or other
injuries or medical issues should have a nasogastric tube inserted and commence
enteral feeds. A dietician should be involved to ensure adequate nutrition is
met including an assessment of increased macronutrient and micronutrient
requirement (consider supplementation vitamin A, vitamin C and zinc to promote
wound healing). Regular weight measurements aid assessment of adequate
nutrition.
In burns >15% TBSA NGT feeds should be commenced within 6 hours
of the burn.
Positioning
Burn areas should be elevated to limit oedema (monitor for
compromise of peripheral circulation). When a burn crosses a joint, joint
should be positioned to maintain optimal functional range of movement with
consultation with occupational therapy and physiotherapy team.
Post
Acute Care Complications
Itch
Healing wounds are often itchy. Non sedating antihistamines are a
safe option for symptomatic management.
Oedema
Circumferential burns inhibit lymphatic drainage and venous return
resulting in oedema which may take 1-2 weeks to resolve. Elevation of the area
will limit amount of oedema and accelerate resolution of oedema and minimise
neurovascular compromise.
Fever
Fever is a common reaction to hypermetabolic state and immune
response following a burn injury however the child must be assessed for other
causes. Prophylactic antibiotics are not recommended in burns.
If there is concern the burn wound is infected send a swab for MCS
and treat with empiric antibiotics as per local guidelines.
Toxic shock syndrome (TSS) is a rare complication of an infected
burn and can be life threatening.
Signs/symptoms TSS
- Shock (tachycardia, hypotension)
- Fever >38.9 degrees
- Erythematous rash
- Diarrhoea and vomiting
- Lethargy
- Irritability
Treatment includes active resuscitation with IV fluids, IV antibiotics
and urgent paediatric and burns specialty care.
Psychosocial
care
The consequences of a child sustaining a burn can be profound on
the child and their family’s psychological,
emotional, social and financial wellbeing. Children have evolving development
with different physical, cognitive and emotional abilities. Children are
dependent on carers and of children presenting with burn injuries a significant
portion are vulnerable children. Treating a child with a significant burn
injury can involve multiple invasive frightening procedures, protracted
treatments and regular engagement with a health facility. Treatment compliance
is important to achieve the best outcome possible. Caring for the child includes support for
family members which includes multidisciplinary team approach noting a family’s
needs may change from acute care to rehabilitation and the child’s transition
back to community and school.
Rehabilitation
Depending on the size and site burn injuries can be associated
with a significant risk of limited functioning. Appropriate burn care includes
optimising function after a burn to achieve the best possible outcome.
Some burns may require review by occupational therapy or
physiotherapy team, including:
- Hand burns
- Deep dermal or full thickness burns
crossing flexor surface of a joint (risk of contracture)
- Significant oedema limiting limb
function or vascular integrity (poor capillary return, cool to touch distal to
burn)
- Immobilisation by use of splint may be
required to ensure safe position or integrity of underlying body structures
Ongoing OT requirement may be
necessary to optimise patient function and minimise risk of irreversible complication such as contracture and
deformity
Rehabilitation is a long and
intensive process
and will commence as early as possible (often in hospital) and continue at home
with community supports. Therapy may involve a comprehensive plan including
passive and active exercises as well as resting splints. Patients and their family
are required to take on responsibility for and play an active part in ongoing
rehabilitation.
Scar
management
Pressure dressings are utilised to minimise scarring post burn.
Therapists may tailor pressure garments unique to the patient’s requirements and provide exercises to
optimise a patient’s functional outcome.
Skin is altered after a burn and
requires regular moisturising to prevent cracking and breaking down which can
lead to secondary infection.
Burn
reconstruction
Most burns managed well initially will not require reconstruction.
Sometimes burn reconstruction will be recommended to optimise comfort, function
and appearance. This occurs many months
after the initial burn.
Paediatric Home
Safety Tips to Prevent Burns
- Ensure cups of hot liquid are always
out of reach of children
- Thick soup is more viscous and remains on a
child continuing to burn them – wash soup or hot food off with cool running
water and continue first aid for 20 minutes
- Avoid table clothes as children can
pull hot food/drinks down
- Always ensure handles of pots on the
stove are angled in and out of reach of children
- Ensure cords in kitchen not long or
hanging down into child’s reach (eg kettle/toaster able to be pulled down by
loose cord)
- Install a guard around hot plates on
stove
- Ensure deep fryers are OUT of reach of
children
- Block off entry to kitchen with
childproof gate
- Always check bathwater before putting
child in bath
- Put in cold water first, then add hot
water, temperature should not exceed 50 degrees
- Do not leave children unattended in
bath
- can turn on hot tap directly causing
burn
- can electrocute self in bath with
bathroom electronic equipment (hairdryer, shaver etc)
- Always run some cold water through the
tap last so faucet is not hot
- Ensure smoke alarms installed and
functioning to the Australian Standard, replace batteries each year with
daylight savings
- Always supervise children around any
naked flame (candle, fireplace, BBQ)
- Ensure children cannot access
matches/lighters
- Do not use accelerants on an open fire
(eg petrol, grappa, methylated spirits)
- Ensure secure storage of flammable
material within the home
- Do not set off fireworks/flares
- Do not smoke around children, do not
smoke whilst carrying child in baby carrier (ash and cigarette can burn child’s
face)
- Place guards around heaters and teach
children not to touch or stand too close
- Do not leave power cords plugged in
and accessible to children
- Place safety blocks into unused power
points
- Do not use electric blankets in
children’s bed (risk of overheating, risk of electrocution if wet bed)
- Replace any electrical cords that are
frayed/broken down
- Lock up all cleaning materials and
ensure children have no access
- Do not store cleaning materials or
other home maintenance materials
in old food containers (eg coolant in soft drink bottle, snail bait or
rat poison in ice-cream container)
- Ensure batteries are stored away from
access to children
- Limit use of toys/devices requiring
button batteries and if used ensure safety cap over battery compartment are always
securely screwed in
- Ensure running treadmills are
inaccessible to children
- Electricity switched off at power and
unplugged
- In separate room child cannot get into
- Walled off with child’s playpen
[i] W
https://www.who.int/violence_injury_prevention/child/injury/world_report/Burns_english.pdf
[ii] World Health
Organisation, Burns, 2018.
https://www.who.int/en/news-room/fact-sheets/detail/burns
[iii] Australian
Institute of Health and Welfare, Burns and Scalds.
https://www.aihw.gov.au/reports/injury/burns-scalds/contents/table-of-contents
[iv] AIHW: Pointer S
& Tovell A 2016. Hospitalised burn injuries, Australia, 2013–14. Injury research
and statistics series no. 102. Cat. no. INJCAT 178. Canberra: AIHW.
[v] Hettiaratchy S, Dziewulski P. ABC of burns: pathophysiology and types of burns British Medical Journal. 2004; 328(7453): 1427–1429.
[iv] Rogers AD, Karpelowsky K, Millar AJW, Argent A, Rode H. Fluid Creep in Major Pediatric Burns European Journal of Pediatric Surgery 2010; 20(2): 133-138.
[vii] CHQ-GDL-06003 – Management of a paediatric burn patient within the Pegg Leditschke Children’s Burns Centre. Children’s Health Queensland Hospital and Health Service.
[viii] Clinical Guideline, Statewide Burn Injury Service – NSW Burns transfer guidelines (4th edition). Page 12 Electrical burns: table Overview of electrical injuries
[ix] Life in the Fast Lane. Carbon Monoxide Inhalation [online]. Dr Neil Long, last update August 25, 2019. Viewed 13th May 2020. https://litfl.com/carbon-monoxide-inhalation/
[x] Life in the Fast Lane. Cyanide Poisoning [online]. Dr Chris Nickson, last update April 2, 2019. Viewed 13th May 2020. https://litfl.com/cyanide-poisoning-ccc/
[xi] Victorian Forensic Paediatric Medicine Service. Burns Including Scald Burns [online]. Viewed 20th April 2020. https://www.rch.org.au/vfpms/guidelines/Burns_including_scald_burns/