Introduction
Tonsillectomy +/- adenoidectomy is a surgical procedure commonly performed at The Royal Children’s Hospital.
Surgery is most commonly performed for children who have Obstructive Sleep Apnoea, Sleep Disordered Breathing and recurrent tonsillitis.
Aim
To provide nursing staff with a guideline for the postoperative management of children who undergo tonsillectomy +/- adenoidectomy so that care can be standardised across all inpatient wards, Day of Surgery and Wallaby.
Definition of Terms
- Adenoidectomy: The surgical removal of the adenoids
- Desaturation: Oxygen saturations level below 90%
- Failed Downloadable Oximetry: A child who has had breathing issues and/or desaturations during spO2 monitoring overnight.
- Obstructive Sleep Apnoea: Complete or partial obstruction of the upper airway which presents as snoring with pauses in breathing while asleep. For most young children this is often from large tonsils and adenoids but can also be due to the relaxation of the tongue and airway muscles.
- Passed Downloadable Oximetry: A child who has passed overnight oximetry will have been spO2 monitored overnight and not had any oxygen desaturations.
- Tonsillectomy: The surgical removal of the tonsils
- Tonsillectomy and Adenoidectomy T & A: surgical removal of tonsils and adenoids for reasons of obstruction or infection
Assessment
- Routine Post Anaesthetic Observations are required for all patients post tonsillectomy. Please refer to RCH Nursing Guideline: Routine Post Anaesthetic Observation.
- All children should have continuous oximetry when they are asleep.
- All children who are admitted to an inpatient unit should be placed on a Nellcor™ downloadable oximeter overnight, an order should be placed in EMR for overnight oximetry.
- The low SpO2 alarm limit should be set to 90%. Ensure heart rate parameters are set to age-appropriate limits.
- The oximetry report is downloaded and printed in the morning if the child has had desaturations or if the nurse was concerned about the patient’s breathing. The printed report must be reviewed by the treating team (usually the ENT Registrar) on the morning ward round.
- Regular pain assessments, please refer to the RCH Nursing Guideline: Pain Assessment and Measurement.
- All patients should continue on 4 hourly observations until discharge, for more information please refer to RCH Nursing Guideline: Nursing Assessment.
Management
Early management
- Tonsillectomy (+/- Adenoidectomy) patients going home via day surgery should be observed for minimum 3 hours prior to discharging home or transferring to
Wallaby.
- Adenoidectomy patients going home via day surgery should be observed for a minimum of 2 hours prior to discharge.
- Diet should be introduced as soon as possible, there are no restrictions on what children can eat however they may prefer a soft and cool diet.
Analgesia Regimen:
Please note this is a plan specific for patients who have undergone surgery at RCH, it relates to both inpatients admitted overnight at RCH and/or Wallaby. Education should be provided about the analgesia regimen to parents/carers on discharge.
First line of pain management post operatively:
Medication Name |
Type of Medication |
Frequency/ Special Instructions |
|
Paracetamol |
Simple Analgesic |
Given strictly every 6 hours including overnight for a minimum of 7 days. Continue to administer as required up to 10-14 days.
|
AND |
| Ibuprofen |
Nonselective NSAID |
Given 3 times a day, 8 hrs apart for a minimum of 7 days.
NOT to be given with other NSAIDS (e.g. Celecoxib).
|
OR |
|
Celecoxib |
An oral COX-2 inhibitor
|
The recommended dose at RCH for patient’s post T & A is 4mg/kg up to a maximum of 200mg BD, given regularly for 7 days. To be commenced day 1 post operatively.
NOT to be given with other NSAID (e.g. Ibuprofen) |
Ibuprofen is safe to use in patients post Tonsillectomy +/- Adenoidectomy, however this should not be administered with other NSAIDS (e.g. Celecoxib).
Second line of pain management post operatively, or “break though pain”:
Medication Name |
Type of Medication |
Frequency/ Special Instructions |
| Oxycodone |
Narcotic analgesic for severe pain |
Caution should be taken with children who have OSA. |
|
OR |
| Tramadol |
Synthetic opioid like analgesic for moderate to severe pain |
Given only for breakthrough pain relief.
RCH does not recommend the prescription of tramadol drops, instead tramadol capsules are ordered, and nursing staff are to disperse in water and give the recommended dosage.
|
Overnight oximetry
- Children with OSA who are yet to pass a night on overnight oximetry should be placed on continuous monitoring while they sleep.
- Overnight downloadable oximetry should be repeated if the patient failed to pass the first night.
- Patients who are placed on overnight oximetry should have a well-documented sleep diary to correlate with the printed oximetry report.
- A sleep diary can be written in the patient’s progress notes and should include the following important information:
- Time of connection/disconnection of oximetry including, start time, end time, toilet breaks, probe disconnection
- Time of disruption in sleep such as, patient woken for pain medication
- Time of desaturation
- Sp02 at time of desaturation
- How long the desaturation lasted
- If the desaturation was self-resolving, if so how? (e.g. Did the patient reposition themselves or did they cough and clear obstruction?)
- Respiratory effort, use of accessory muscles, colour changes, respiratory sounds-without stethoscope (stridor, snore, wheeze or grunt etc.)
- Did staff have to reposition/intervene to assist in correcting the desaturation/obstruction?
- Sp02 after desaturation resolved
- Note if the trace on the machine was good or poor at time of desaturation (to rule out artifact)
Example of a sleep diary progress note:
2200: settled to sleep, commenced overnight oximetry (trend data cleared). Nil noisy breathing.
0130: brief desaturation to 89% on RA, lasting less than 2 seconds. Self-resolving, patient sleeping on their side, patient then coughed and stirred in his sleep. Sp02 back up to 95% on RA.
0205: desaturation
<83% on RA- poor trace, moving around in bed. Artifact. Probe checked. Once patient settled, good trace sp02 at 97% on RA.
0400: desaturation 86% and dropping to 81% over 5 seconds, not self-resolving. Loud obstructive snore, tracheal tug noted. Nursing staff repositioned patient onto their side as patient laying on their back. Sp02 returned to 96% after repositioning.
0525: probe disconnect as patient went to bathroom
0530: reconnected probe
0700: oximetry turned off & report downloaded for review.
Ongoing management
Maintain IV access until the day of discharge, for more information please refer to RCH Nursing Guideline: Peripheral Intravenous IV Device Management.
Management a patient with oxygen desaturations following T's +/- A's
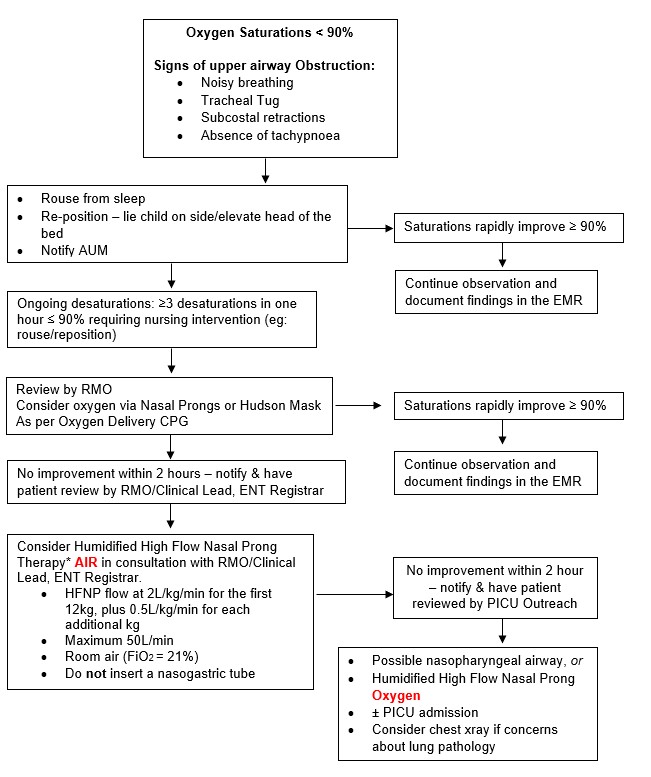
For further information regarding management of oxygen delivery, please review
RCH Nursing Guideline: Oxygen delivery
*If starting Humidified High Flow Nasal Therapy Air
- Inform Medical Lead 52748 (After Hours)
- Notify ENT Registrar (via switch)
If no improvement with Humidified High Flow Nasal Air - notify PICU Outreach
- 0800-1800 PICU Outreach Nurse 52305
- 1000-2200 PICU Outreach Registrar 52327
- General PICU Registrar -24 hours 52326
For further information regarding management of HFNP therapy, please review RCH Nursing Guideline: High Flow Nasal Prong (HFNP) Therapy.
The use of High Flow Nasal Prong Air for the management of children who have oxygen desaturations after T&A has been approved by the Royal Children’s Hospital New Technology and Clinical Practice Committee. In the protocol it has also been approved that insertion of a nasogastric tube is not needed due the potential to cause trauma and bleeding post tonsillectomy & adenoidectomy.
A patient whose oxygen saturations are 90-93% in room air falls within the orange zone on the ViCTOR chart. In line with the RCH Policies and Procedures: Medical Emergency Response, These patients require a clinical review. A nursing review with the bedside nurse and ANUM is required, a documentation of the rationale and plan of care should be carried out and discussed with the family.
Remember that you can request a Rapid Review or a MET call at any time.
Managing Post-Operative Bleeding
- Post tonsillectomy bleeding is uncommon (5% of patients), but can potentially be a serious event. The main difficulties arise from aspiration of blood and hypovolaemic shock
- Primary bleeding (not common) – occurs within 24 hours of surgery, will likely need to return to theatre
- Secondary bleeding – occurs most commonly at day 5 to 10 post surgery, usually self-limiting and does not require return to theatre
- It usually requires observation in hospital as there may be a subsequent bleed
- Report any bleeding to the ENT Registrar on call and the ANUM.
- Keep the patient nil by mouth. Consider antiemetic if patient nauseated.
- Insert/maintain IV access
- STAT IV/O Tranexamic Acid (15mg/kg) unless contraindicated (see
AMH Children's Dosing Companion for dosing).
- Record estimated amount of blood loss (note that bleeding may be haemoptysis or haematemesis as children often swallow blood).
- Allow patient to sit upright, leaning forward to assist in keeping blood out of airway.
- Monitor for signs and symptoms of hypovolemic shock. Consider the need for continuous cardiac monitoring.
- If no active bleeding, keep patient nil by mouth for 6 hours or until review in the morning.
If airway, breathing or circulation is compromised call a MET or Resus Team
- If active bleeding continues or concern of hypovolemic shock
- Set up for insertion of 2 IV Cannulas (large bore) and prepare for FBE, Coagulation Screen, Group and Hold, Cross Match
- Consider the need for
- Manage child’s fluid status as per signs of hypovolemic shock, for more information please refer to RCH Nursing Guideline: Adrenaline and fluid bolus administration in resuscitation.
- Additional agents to consider include Tranexamic Acid (IV), Adrenaline 1:10000 for topical use, further information can be found via
Medicines Information.
Discharge Home or Transfer to Wallaby
- Most children can be placed on a
Criteria Led Discharge (see RCH policies and procedures: Criteria Led Discharge) for the next morning post-operatively
- Patient must be tolerating diet and fluids
- Pain controlled
- Tonsil bed inspection by a registered nurse when clinically indicated and concerns for post-operative bleeding (excessive swallowing or blood around the mouth).
- If applicable, downloadable oximetry reviewed by ENT Registrar
- Afebrile and other observations within age-appropriate limits
- Family state that they understand the care at home
- Patients who met a set criteria may be transferred to Wallaby from day surgery see Transfer to Wallaby (Day Case Tonsillectomy +/- Adenoidectomy) below for more information.
Parent/Carer Education
- All patients should be given the Tonsillectomy and adenoidectomy (T&A) – discharge care Kids Health Info factsheet along with the Tramadol Pharmacy factsheet and the Celecoxib Kids health info factsheet (if prescribed these medications).
- In depth education regarding analgesia, diet and oral intake, activity at should take place with the family prior to discharge from RCH
- If patient is discharged home with Celecoxib or Tramadol, please ensure the script is filled at the RCH pharmacy, these medications may be difficult to obtain from external pharmacies.
- Family understand the medications including dosage, timing of administration and how to make up appropriate dosage when using capsules. To access a pain management plan for the family please
click here. - Risk of secondary bleeding should be discussed with the parents/carer prior to discharge/transfer this includes the risk of spitting, coughing, or vomiting blood
- All patients with bleeding of more than a tablespoon or 50 cent piece size should present to RCH emergency department or their local ED if closer (if suitable management can be delivered there) for further assessment. A list of appropriate hospitals can be
found here . If bleeding is significant, active /ongoing OR patient has an altered level of consciousness/is unresponsive or having difficulties breathing then an ambulance should be called.
Discharge Follow up
- All patients are encouraged to be signed up to the
RCH patient portal.
- Follow up for patients involves families receiving a symptom questionnaire via the patient portal on days 1, 3, 5, 7, 9 post operatively.
- The questionnaire will ask about pain management, intake/output, bleeding, nausea and any further concerns will be flagged to the treating team. The questionnaire results are monitored by the ENT CNC Monday-Friday & ENT Reg on weekends/after hours.
Transfer to Wallaby (Day Case Tonsillectomy +/- Adenoidectomy)
Please note the following refers to patients admitted to RCH only
Day case tonsillectomy +/- adenoidectomy patients can be discharged home with CNC Portal support, or with transfer to Wallaby (Hospital-in-the-home) for ongoing support for some low-risk patients.
Current patient eligibility criteria (see flow chart below):
- Children seen in the preoperative ENT clinic with symptoms of OSA or recurrent tonsillitis are considered for day case surgery and Wallaby transfer post T’s +/- A’s, according to the following eligibility criteria:
- Age greater than or equal to 3 years
- Weight greater than or equal to 15kg
- No significant co-morbidities or syndromes that may increase risk of post-operative complications
- Living within 60 km of the hospital
- Parents have car, phone and are consenting
- A preoperative overnight oximetry study (normal/inconclusive, inconclusive, significant OSA with a Nadir over 85%, or at the discretion of the ENT team)
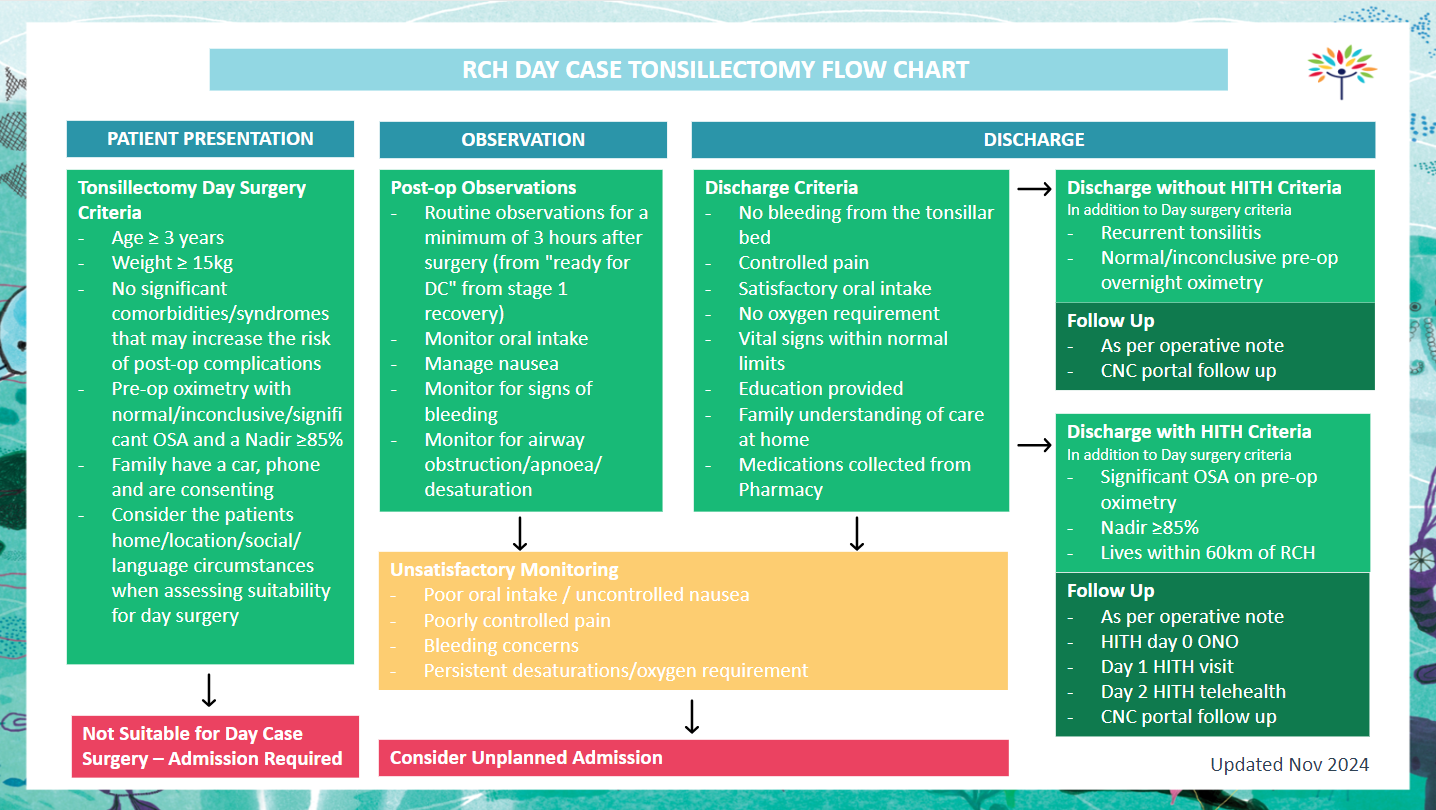
Day of Surgery
Patient completes up to 3 hours postoperative observation in recovery/day surgery and may then discharge if:
- Patient completes up to 3 hours postoperative observation in recovery/day surgery and may then discharge if:
- No upper airway obstruction/apnoea in recovery or prolonged recovery stay
- If desaturations have occurred during the patients stay in day surgery, a review from the ENT team must occur to determine patients ongoing suitability for day case verses overnight stay.
- No primary bleeding from tonsillar bed (i.e., spitting, vomiting, or coughing up blood)
- No nausea or vomiting and tolerating oral intake (e.g., icy pole or apple juice)
- Parents have collected medications from pharmacy to go home (paracetamol, ibuprofen or celecoxib, and script for oxycodone) and are confident with administration
- Postoperative T&A education completed
- ENT CNC or Wallaby CNC (if applicable) has reviewed patient to discuss the protocol.
- If applicable - Family provided with oximeter for first night at home and oximetry education package including the flowsheet for management of overnight desaturation, a patient oximetry record sheet and a food and fluid chart for the families to fill out. (Oximeter alarm limits set: Low SpO2 alarm to be set at 90%, high HR 200, low HR 50)
Companion Documents
Links
- RCH Nursing Guidelines
- RCH Policies and Procedures
Evidence Table
Please remember to
read the disclaimer.
The development of this nursing guideline was coordinated by Bec Marshall and Claire De Simone, CNC, Department of Otolaryngology, and approved by the Nursing Clinical Effectiveness Committee. Revised December 2022.