Introduction
Aim
Definition of Terms
Indications for insertion of NPA (Medical Patients)
Indications for insertion of NPA (Surgical Patients)
Contraindications for insertion
Assessment
Management
Insertion / Re-insertion of a NPA (ward setting only)
Insertion and Securing of NPA
Securement of a NPA (all settings)
Ongoing Assessment and Management
Documentation
Removal of NPA
Discharge Planning for patients requiring an NPA at home
Complications associated with NPA insertion
Special Considerations
Evidence Table
Introduction
A nasopharyngeal airway (NPA) is a thin, clear, flexible tube that is inserted into a patient’s nostril. The purpose of the NPA is to bypass upper airway obstruction at the level of the nose, nasopharynx or base of the tongue. It also prevents the tongue falling backward on the pharyngeal wall to prevent
obstruction. NPA’s maintain airway patency in patients who are conscious or semi-conscious, they can be used in neonates to adults.
Aim
The aim of this Clinical Guideline (CG) is to provide a framework for the insertion and management of NPA’s to relieve airway obstruction, in a self-ventilating patient within a medical ward setting and/or for surgical patients postoperatively in the Post Anaesthetic Care Unit (PACU)
and surgical ward.
Definition of Terms
NPA: Nasopharyngeal airway; is a soft, anatomically designed airway adjunct inserted into the nasal passageway to provide airway patency.
Upper Airway Obstruction: Upper airway obstruction above the level of the larynx results in a failure of airflow into the lungs, despite adequate inspiratory effort. Increasing respiratory effort can worsen the obstruction, as increased intra-thoracic pressure collapses the soft tissue structures inwards.
OSA: Obstructive Sleep Apnoea
PACU:
Post Anaesthetic Care Unit
OT: Operating Theatre
EMR:
Electronic Medical Record
ENT: Ear, Nose, Throat
Micrognathia: is a condition in which the jaw is undersized. It is a symptom of a variety of craniofacial conditions. Sometimes called mandibular hypoplasia
Glossoptosis: An abnormal posterior placement of the tongue, which may occlude the airway
WOB: work of breathing
PPE: Personal Protective Equipment
Stertor: noisy, snoring-like breathing resulting from obstruction in the naso- or oropharynx
Indications for insertion of NPA (Medical Patients)
MEDICAL PATIENTS:
A patient’s bed card team should determine whether a NPA is required and order accordingly, ensuring the appropriate size and length are included.
Common indications for patient’s in a ward setting:
- Respiratory distress from upper airway obstructions and increased WOB
- Airway obstruction/obstructive episodes noted by medical, nursing, or allied health staff
- Airway complications with episodes of mild stertor, causing a decrease in Sp02
- Significant respiratory distress, further evidenced by hypercapnia on blood gas results
Indications for insertion of NPA (Surgical Patients)
Elective
Nasopharyngeal Airway Insertion:
NPA’s are inserted at the end of surgery when the patient is anaesthetised. This enables the NPA to be inserted under direct vision to the correct length.
NPA’s are commonly inserted electively at the end of surgery to prevent problems with postoperative airway obstruction, including:
- Micrognathia associated with congenital syndromes ie. Pierre Robin sequence, Treacher Collins, Stickler Syndrome
- Children with muscular dystrophy or other syndromes affecting the airway (ie. Velocardiofacial syndrome, Stickler syndrome, Treacher Collins Syndrome, CHARGE association, Trisomy 21)
- Children who have pre-existing OSA and children post operatively where upper airway structures are expected to become swollen (ie. Adenotonsillectomy, palate repair, pharyngoplasty, tongue surgery)
- Children who required a NPA to maintain airway patency at any point prior to their surgery
- Children who develop airway obstruction with loss of pharyngeal tone following induction of anaesthesia
Children who have a NPA inserted intra/postoperatively, generally only require it for the first postoperative night. It is then removed the next day as directed by the bed card team.
Insertion
postoperatively in PACU:
- Airway complications postoperatively from episodes of mild stertor, causing a decrease in Sp02, requiring intervention
- Obstructive episodes noted by medical, nursing, or allied health staff
- Significant respiratory distress and work of breathing, further evidenced by hypercapnia on blood gas results
If an NPA is accidentally removed, reinsertion should only be done after consultation with surgical team, to avoid damaging the operative site.
Contraindications for insertion:
(ward setting only, does not inc
lude NPA’s inserted in surgical patients in OT/Recovery)
- Bleeding disorders
- Nasal or cranial trauma (ie. recent palatal surgery – risk of damage to surgical site(s)
- Newborn septal deviation
- Nasal polyps
- Craniofacial abnormality
Assessment
- Ensure necessary equipment is setup at patient bedside
- Functioning suction equipment
- Yankeur sucker
- Appropriate sized suction catheters
- Oxygen and correct size face mask
- Record patient’s NPA size
- Suction catheter size
- Suction depth measured and recorded (ruler for depth of suctioning required at bedside to enable easy measurement of suction catheter when suctioning)
- Spare NPA (of the same size insitu and one size smaller)
- Brown Leukoplast rigid tape, 25mm
-
Check patency
of NPA 1-4/24
according to clinical judgement
- NPA’s inserted on the ward - Planning of ongoing assessment can be made for patients according to their condition and disease
- Ensure NPA is secure
- Assess integrity of surrounding skin & regularly check tapes
- If the nares are white, the tube needs to re-taped promptly to reduce pressure on the nostril, or assessment for requirement of a smaller sized NPA
- Please refer to
Management
Insertion / Re-insertion of a NPA (ward setting only)
A patient’s bed card team should determine whether a NPA is required and order accordingly, ensuring the appropriate size and length are included.
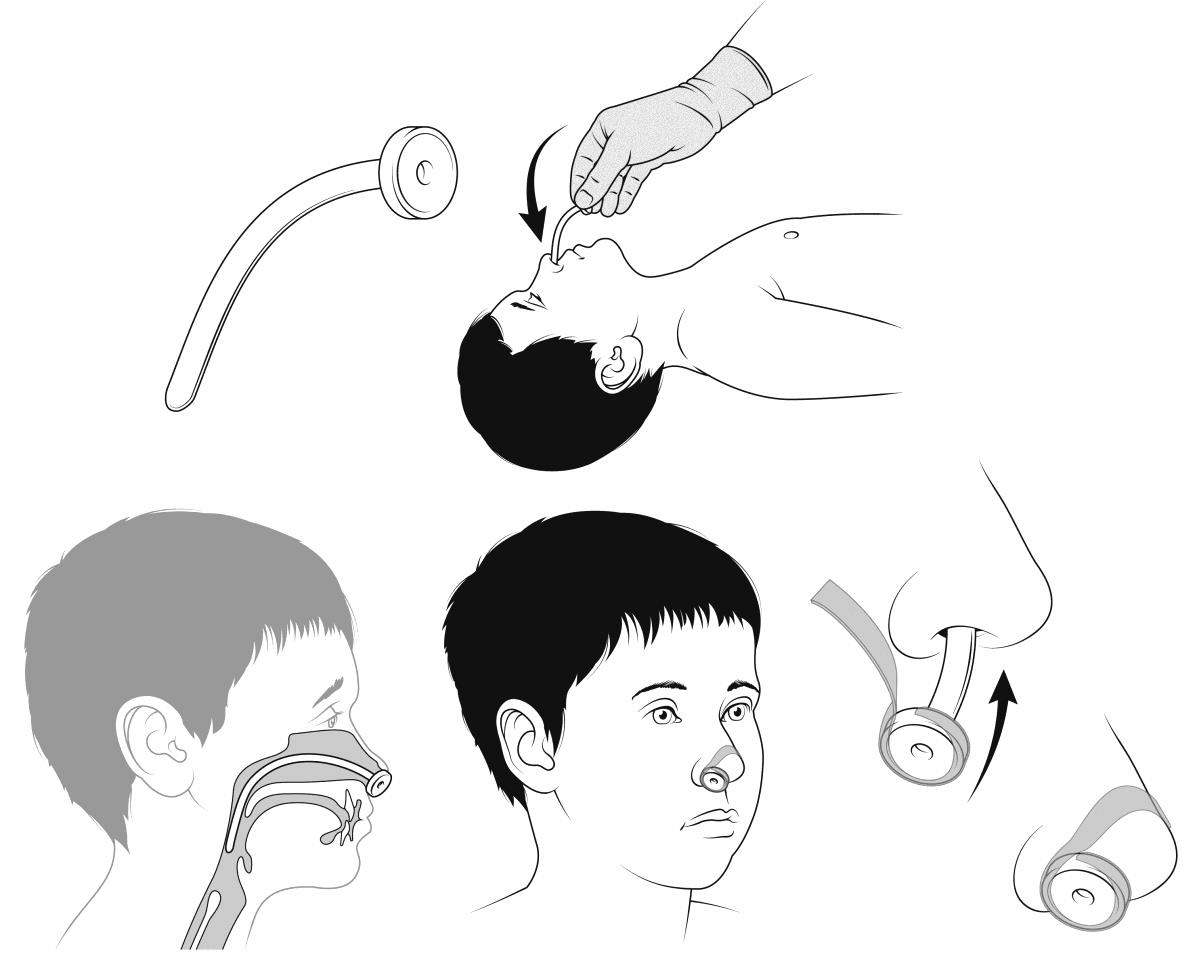
Insertion and Securing of NPA :
- Perform
Hand Hygiene (See RCH Policies and Procedure: Hand Hygiene)
- Clean trolley / work surface with Tuffie wipes
- Identify and gather all equipment for procedure, ensure variable suction equipment is functioning, leave sterile suction catheter attached but within protective cover
- Select appropriate size of NP tube
- A guide of measurement is from the lateral aspect of the nares to the tragus of the ear on the same side
- Size is chosen largely based on length rather than diameter, correct length ensures the tip sits just above the epiglottis
- Prior to insertion, measure the suction depth of the NPA
- Perform Hand Hygiene (See RCH Policies and Procedure: Hand Hygiene)
- Don appropriate PPE, including goggles (See RCH Policies and Procedure: Transmission Based Precautions)
- Ensure appropriate positioning
Comfort Kids Positioning Poster and consider therapeutic techniques (see also RCH Nursing Guideline: Procedure Management)
- Prepare patient and caregiver, including obtaining consent where possible
- Ensure the patient’s nostrils are clear of secretions, suction if necessary
- Moisten the tip of the NPA tube with sterile water or water-based lubricant to ease insertion
- With the tube tip facing downward, gently insert the tube into a nostril, using a curving motion to follow the natural path of the floor of the nose.
The tube should pass to just below the level of the soft palate and should be checked with a light and tongue depressor - in case it is too long (causes gagging) or too short (may not bypass the obstruction). If you are unable to insert the NPA, STOP,
do not force, and escalate to medical/senior nursing team for assistance.
- Secure the NPA - see Securement of a NPA below
- Complete documentation on patient EMR in ‘flowsheets’ tab under LDA Assessment– see documentation section
Securement of a NPA (all settings)
- NPA’s need to be secured with tapes, as it is deemed a critical airway. Comfeeltm or similar (Hydracolloid or similar (Hydrocolloid Polyurethane film dressing) is recommended to be used on the patient’s cheeks, to ensure skin integrity is
maintained.
- Secure by applying brown Leukoplast rigid tape (25mm)/cotton ties around the exposed end of the NP tube and then across the bridge of the nose and onto the closest cheek/s see figure 1
Figure 1:
Ongoing
Assessment and Management:
Initially after insertion of the NPA the child may need to be suctioned more than normal, as there will be mucus in the nose and pharynx. This should settle, if it does not seek medical review.
- Regular cleaning of nares with water or saline
- Suctioning:
Suctioning of the NPA tube is necessary to remove excess mucous, secretions (and blood for postoperative patients) to maintain a patent airway and avoid tube blockage.
- It is important that the lowest effective suction pressure (80-120mmHg / 10-16kpa) is used
- Only suction to the end of the tube and no further – measurements should be documented in EMR & kept at patient bedside as outlined above.
- If an NPA is inserted on the ward - The frequency of required suctioning is based on individual patient assessment
- NPA’s inserted postoperatively should be suctioned at regular intervals 1-2 hourly, as directed by treating team, or when clinically indicated.
Additional Indications for
suctioning:
- Audible or visual signs of secretions in the tube
- Signs of respiratory distress and dysfunction
- Suspicion of a blocked or partially blocked tube, escalate accordingly to bedcard team
- Vomiting
- Desaturation on pulse oximetry
- Requested by patient (older patient)
* follow local medical emergency response procedure, if clinically indicated (signs of respiratory distress).
For further assessment information please see the RCH Nursing Guideline: Nursing Assessment.
Documentation
- Document all assessments and interventions on patient’s LDA Assessment on EMR including:
- Secretion type and colour
- Secretion amount
- Respiratory difficulty
- Tube patency (patent, semi obstructed, obstructed)
- Suction catheter ease of passage
- Site assessment (nose)
- Securement method
- NPA change
- Reason for change
Removal of NPA
Prior to removing NPA assess and document vital signs including a full respiratory assessment
Respiratory Assessment in the RCH Nursing Guideline Nursing Assessment.
A patient who has had an NPA inserted postoperatively will require a surgical team review prior to removal.
- Post NPA removal perform vital signs/observations and respiratory assessment and ensure line of sight nursing for 5 minutes. Observations should then be assessed after 30 minutes, followed by hourly for 2 hours. Observations should include:
- Heart rate
- Respiratory rate and sounds
- WOB
- SpO2 monitoring
- A patient who has had a NPA inserted postoperatively, may require continuous SpO2 when asleep for 24 hours post NPA removal.
Discharge Planning for patients requiring an NPA at home
- Training of parent/caregivers
- Supplies of consumables and suction equipment
- Emergency management and complex care referral
Table 1: Recommended suction catheter sizes:
| NPA tube
size (in mm) |
2.5 |
3.0 |
3.5 |
4.0 |
4.5 |
5.0 |
5.5 |
6.0 |
6.5 |
7.0 |
7.5 |
| NPA
length (cm) |
6.5 |
7.5 |
8.5 |
10.5 |
11.0 |
11.5 |
12.5 |
13.0 |
14.0 |
15.5 |
16.5 |
| Recommended
suction catheter size (Fr) |
6 |
6 |
6 |
7 |
7 |
8 |
8 |
10 |
10 |
12 |
12 |
Complications
associated with NPA insertion:
|
Complication
|
Management
|
| Accidental dislodgement/displacement/blockage of the NPA |
Clean and reinsert
/replace NPA (in consultation with treating team)
- *do not re-insert in patients where surgical site can be damaged
|
| Upper airway trauma |
The nostrils have a large blood supply and will bleed if traumatised, if any blood appears in the mouth or nose after insertion, suction to gently remove any blood and monitor patient |
| Anxiety and fear |
RCH Nursing Guideline: Procedure Management |
|
Discomfort |
Discuss use of local anaesthetic with treating team |
| Skin infection/altered skin integrity |
May indicate need to alternate nostrils to enable skin to heal.
RCH Nursing Guideline: Pressure injury prevention and management
|
Special Considerations
- Nasal passage mucosal damage may be caused by suctioning. This can be minimised by using the appropriately sized suction catheter or using a short connector on the outside of the nose; appropriate suction pressures should be used and suctioning within the NPA tube only. The
depth of insertion of the suction catheter needs to be determined prior to suctioning
- Measure the length of the NPA using a suction catheter prior to insertion, or refer to the NPA size chart
- Option for use of a spare NPA tube of the same type and size and insert the suction catheter to accurately measure the length of the NPA tube
- Use pre-measured suction catheters (where available)
- It is recommended that any single episode of suctioning (including passing the catheter and suctioning the NPA tube) is completed within 5-10 seconds
- Children can often feed with the tube in place; however some children experience problems with fluid or food coming into the tube and causing obstruction.
- Residual anaesthetic, opioids and blood, or secretions can contribute to upper airway obstruction.
Evidence Table
The evidence table for this guideline can be viewed here.
Please remember to read the disclaimer.
The development of this nursing guideline was coordinated by Lauren Jorgensen, CNS, and Casey Clarke, CSN, Sugar Glider, and approved by the Nursing Clinical Effectiveness Committee. First published August 2022.