Midazolam (meh-daz-owe-lam) is a medication that is commonly used as emergency treatment for seizures. It is a benzodiazepine (ben-zo-die-az-eh-peen) medication like diazepam (valium) or clonazepam (clonn-az-eh-pam). Midazolam works more quickly than diazepam but does not last as long. It is also
occasionally used for sedation during medical procedures.
Midazolam can be delivered in three ways:
- buccal: placed on the inside of the cheek (an area called the buccal mucosa)
- intranasal: sprayed or dripped into the nose
- intravenous (IV) or intramuscular (IM): injected into a vein or muscle.
Swallowing midazolam is not recommended as it is not absorbed well through the stomach. Intranasal midazolam may be better than buccal midazolam in children who vomit or produce excessive saliva during seizures.
Buccal or intranasal midazolam may be prescribed for a child with epilepsy who:
- has prolonged seizures
- has a pattern of seizures that happen close together
- lives a long way from emergency services.
Midazolam is not necessary for all children with epilepsy. Your doctor will tell you whether your child might benefit from buccal or intranasal midazolam.
Giving buccal or intranasal midazolam for seizures
If your child has a seizure, follow the correct first aid procedures before giving any medication. See our fact sheet
Seizures – safety issues and how to help.
The following information describes how midazolam can be given by parents or carers if a child is having a seizure. It may be different from the information in the manufacturer's consumer information.
It is very important to follow your doctor's advice on when and how to give midazolam and when to take your child to hospital.
Specific details for giving your child midazolam should be documented in an Emergency Medication Management Plan and your child's general Epilepsy Management Plan.
Unless your doctor gives you different instructions, call
000 for an ambulance BEFORE giving midazolam. Don't wait for the ambulance to
arrive before giving the midazolam.
Use only 1 mL plastic ampoules containing 5 mg of midazolam. Although the plastic ampoules are labelled 'for slow IV or IM injection', they can be used for buccal and intranasal use. Do not use midazolam in glass ampoules, or plastic ampoules of
other sizes or strengths.
Buccal midazolam can be given by either:
- drops squeezed directly from the ampoule (ampoule method)
- drops trickled from a syringe into which the midazolam has been drawn up (syringe method).
Each ampoule delivers about 18 drops (the volume can vary slightly from 16–20 drops, but this is OK).
Buccal
midazolam
Intranasal midazolam
| Intranasal
midazolam – using a mucosal atomization device (e.g. MAD300) |
| Step 1: Open the plastic ampoule of midazolam by twisting off the top. |
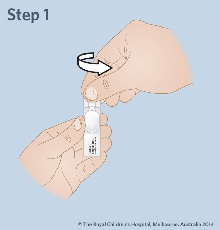 |
| Step
2: Insert the syringe into the ampoule and hold the ampoule and syringe upright with the ampoule higher. Withdraw the required dose as prescribed by your doctor into a 1mL syringe. Push out any big air bubbles and check the amount of midazolam in the syringe. Pull the ampoule and the syringe apart. |
 |
| Step
3: Attach the syringe to the mucosal atomization device. |
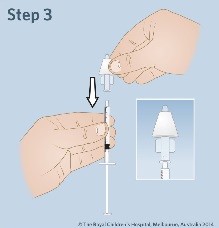
|
| Step
4: Lay your child on their side (recovery position) or in the best position to allow easy administration of intranasal midazolam. Insert the mucosal atomization device loosely into a nostril and press the plunger quickly to give half of the dose. Remove the device and insert into the other nostril to give the
remaining dose. |
 |
| Step
5: Watch your child's breathing and seizure activity while they remain lying on their side in the first aid position. |
|
| Step
6: Write down the time that the seizure started, when the midazolam was given and when the seizure stopped. |
|
Are there any side effects of midazolam?
Midazolam has a sedative effect, and your child may be sleepy for some time afterwards. Headache, nausea (feeling sick), vomiting, coughing and hiccups may also happen. In rare cases, your child may become agitated, hostile or aggressive after having midazolam.
If your child has shallow or slow breathing, call an
ambulance immediately.
Key points to remember
- Buccal midazolam is absorbed directly into the blood stream through the lining of the inside of the cheek.
- It can be given by ampoule or syringe.
- Use the plastic ampoules containing 5 mg midazolam in 1 mL, not glass ampoules or plastic ampoules of other sizes or strengths.
- Keep a record of your child's seizures and use of midazolam.
- Midazolam has some side effects. If your child has shallow
or slow breathing after being given midazolam, call an ambulance.
For more information
Common questions our doctors are asked
Why is the information that comes with the midazolam so
different to this fact sheet's instructions?
The manufacturer's information may refer to midazolam for use in a different way, for instance when it is given as IV or IM injection. It is important to follow your doctor's instructions as outlined in your child's Emergency Medication Management Plan.
Developed by The Royal Children's Hospital Children's Neuroscience Centre and Pharmacy. We acknowledge the input of RCH consumers and carers.
Reviewed May 2018.
This information is awaiting routine review. Please always seek the most recent advice from a registered and practising clinician.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit
www.rchfoundation.org.au.