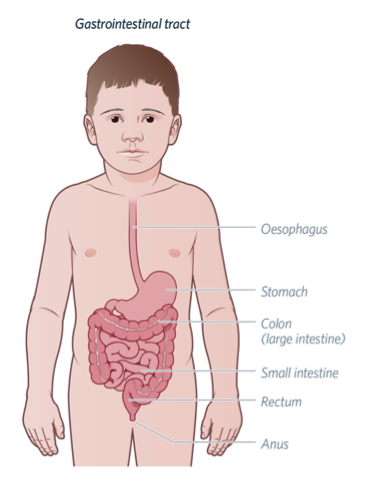
The digestive system carries food through the body after it is eaten. The last parts of the bowel, where stool (poo) exits the body, are called the rectum and anus. The muscles and nerves of the rectum and anus need to work together to control bowel movements (poos). Usually, these muscles are contracted (closed) to prevent soiling (incontinence). When a person has a bowel movement, the muscles must relax together to allow the stool to exit the body.
The function of the muscles in the anus and rectum may be measured using a technique called anorectal manometry. This technique records the pressure waves when the muscles of the rectum and anus contract (squeeze) and relax.
 What is an anorectal manometry study?
What is an anorectal manometry study?
In some children, the muscles of the anus and rectum do not function as they should. This may lead to problems such as constipation or soiling. Anorectal manometry may give us an understanding of how the muscles and nerves are working together.
An anorectal manometry may be performed to help understand the cause of your child’s symptoms, including constipation or soiling. It may also be done before or after surgery.
How is anorectal manometry performed?
To perform an anorectal manometry, a thin, flexible tube (catheter) is placed into your child’s bottom. The tube is filled with water, which drips out of small holes along the side of the tube. A machine measures the changes in pressure of the water leaving the tube. This provides a picture of the patterns of contraction and relaxation of the muscles in the anus and rectum.
A small balloon is attached to the end of the manometry catheter. This may be inflated with different amounts of air to mimic stool in the rectum. The pressures in the anus and rectum are measured as the amount of air in the balloon is changed.
Preparing for an anorectal manometry
- Special bowel preparation, such as an enema (a small tablet or liquid placed into your child's rectum), may be required to empty stool from the rectum. However, the preparation may be different for each child. Details about your child’s bowel preparation will be discussed with you in the lead up to their procedure.
- If your child usually uses any rectal therapies (such as bowel washouts), please bring the equipment with you to hospital. Your child may prefer this as an alternative to an enema.
- Some children may feel anxious about the idea of a balloon being inflated in their rectum. It is important to remind your child that the balloon is very small – it may be better called a “bubble”. Remind your child that they will be in control of the procedure. If it becomes uncomfortable, the balloon can be deflated immediately.
- Bring something to help keep your child distracted during the study. Their favourite toy, book and/or movie may all help keep them relaxed and still during the procedure.
What to expect on the day of an anorectal manometry
- The study is usually done while your child is awake. If this is the case, your child may continue to eat and drink normally before the study.
- You will be able to stay with your child throughout the procedure.
- You and your child will be brought to the room where the study is done. Your child will be positioned lying on their left side, with their knees tucked towards their chest.
- The procedure will take about 30 – 45 minutes.
Performing the manometry study
A lubricating gel will be put on your child’s bottom. It may feel cold. The doctor may perform a rectal examination to make sure the rectum is empty. The doctor or nurse will insert the flexible tube (catheter) into the rectum. The manometry tube will be connected to a machine, which measures the changes in pressure in the anus and rectum.
The doctor or nurse will perform some special tests. These tests may include:
- asking your child to cough
- asking your child to squeeze their bottom
- the doctor or nurse slowly inflating and deflating the balloon
- asking your child to tell the doctor or nurse when they can feel the balloon
- asking your child to push like they are doing a poo
The machine will record the changes in pressure as each test is done to measure how the muscles and nerves are working. After the study, a doctor or nurse will remove the tube from their bottom.
Your child will need to remain in bed during the procedure. Please bring any activities they enjoy, such as games, books and/or electronic devices. This will help them remain still and distracted during the procedure.
Manometry under anaesthesia
- In some cases, your child may require a general anaesthetic for their manometry. This involves a medicine being given through a drip into a vein (intravenous or IV therapy). If this is the case, your child’s doctor will discuss this with you.
- Your child’s team will discuss fasting for the procedure with you. Your child must not eat (no food, milk, lollies or chewing gum) after the time advised by the team. Your child may continue clear fluids (water, clear apple juice) until the time of their admission.
- An anaesthetic doctor will meet with you and your child before their procedure.
- You will be able to stay with your child until right before their procedure, when they go to sleep in the anaesthetic bay.
- After the procedure, your child will be taken to Recovery, where they will slowly wake up from their anaesthetic. You will be able to join them when they are awake.
- The procedure will take about 30 – 45 minutes.
In some cases, your child’s doctor may also recommend other manometry studies (such as colonic manometry) to look at how the rest of your child’s bowel is functioning. If recommended, they will discuss this with you.
For more information, see our fact sheet on
Colonic Manometry .
After the manometry study
If your child did not receive an anaesthetic, they will be able to head home after the test and resume their usual activities.
After an anaesthetic, your child will usually be discharged home on the day of the study. Your child must be feeling well, eating and drinking normally, and have no further tests planned for their admission before they are discharged.
The results will be discussed with you and your child at their next outpatient appointment.
When to seek medical assistance
Call the hospital if your child has:
- a bowel action with more than half a teaspoon of bright red blood
- severe pain
- a high temperature (above 38ºC)
- vomited more than three times over an eight-hour period
Key points to remember
- Anorectal manometry may be used to measure the function of the muscles of the anus and rectum.
- The manometry study requires some cooperation from your child. If they are unable to lie still and/or follow instructions, their manometry may be cancelled or rescheduled. In some cases, your child may require a general anaesthetic. If this is recommended, your child’s doctor will discuss this with you.
- Your child can usually go home soon after after the manometry study.
- Contact the hospital if your child is unwell after their manometry study.
For more information
-
Kids Health Info fact sheet:
Constipation
- Kids Health Info fact sheet:
Colonic Manometry
- The Royal Children’s Hospital Department of Anaesthesia and Pain Management:
Parent Information
- Talk to your GP, gastroenterologist or paediatric surgeon.
Common questions our doctors are asked
What are the risks of the manometry study?
- Your child may experience some pain or irritation around their bottom after the study. Occasionally, they may experience a small amount of rectal bleeding (bleeding from their bottom).
- There is a very small risk the manometry tube may damage the anus and/or rectum. However, this is very rare.
- If there is too much stool (poo) in the rectum, the test may not be performed.
- This test requires some cooperation from your child. If your child is unable to tolerate the study, it may need to be stopped early.
- If your child requires an anaesthetic for the manometry study, they may feel unwell (nausea, vomiting) after the anaesthetic. This usually resolves without any additional treatment.
- Occasionally, the test may need to be repeated.
Please speak to your doctor if you have any questions or concerns about the study.
Developed by Departments of Gastroenterology and Paediatric Surgery at The Royal Children's Hospital, Melbourne. We acknowledge the input of RCH consumers and carers.
Reviewed December 2020.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit
www.rchfoundation.org.au