See also
Vulval ulcers
Sexually transmitted infections
Adolescent gynaecology - lower abdominal pain
Adolescent gynaecology - heavy menstrual bleeding
Key Points
- Vulvovaginitis is common and will usually resolve with simple measures
- Pinworms should be considered when pre-pubertal children present with distressing nocturnal vaginal or perineal pain and/or itch
- Children with recurrent urinary tract infection symptoms but negative cultures should be assessed for vulvodynia
- Do not perform an internal vaginal examination or take internal vaginal swabs in prepubescent children
Background
Normal anatomy and development
- Genitalia will change in appearance between infancy, prepuberty and puberty due to the hormonal environment
- Newborns are affected by maternal oestrogens crossing the placenta. It is common to have breast buds, mucoid white vaginal discharge, small volume vaginal blood loss and/or hymenal skin tags
- From 3 months of age until puberty, vaginal discharge is usually minimal
- Menarche usually occurs 2-3 years after thelarche
Vulval and vaginal pain
Vulval and vaginal pain is common in prepubertal children and many conditions affecting the vulva can be painful including
- Vulvovaginitis
- Vaginal foreign body
- Trauma, including
straddle injuries or
sexual abuse
- Vulvodynia
- Persistent pain in vulval area for ≥3 months without an identifiable cause
- Candida infection (unusual in children from 2 years to puberty)
- Systemic conditions eg eczema, psoriasis
Vaginal bleeding
Vaginal bleeding in the first week of life can be caused by the normal withdrawal of maternal oestrogens (requires no investigation or treatment)
Abnormal vaginal bleeding in children may be caused by
- Vaginal foreign body (toilet paper, small toys or money)
- Excoriation due to moderate-to-severe vulvovaginitis, lichen sclerosus et atrophicus or pinworms
- Trauma, including
straddle injuries or
sexual abuse
- Precocious puberty (consider when secondary sexual characteristics
<8 yo)
- Urethral prolapse (an inflamed “doughnut” of vascular tissue is visible at the urethral meatus)
- Tumour (rare)
Consider causes of non-vaginal bleeding eg
Haematuria
For menstrual bleeding see
Adolescent gynaecology - heavy menstrual bleeding
Assessment and management
Be aware of signs of sexual abuse based on history or examination
History
- Quality, location and triggers of pain
- Burning, stinging, unusual sensation or raw discomfort
- Shooting vaginal or perineal pain at night
- Inability to insert tampons due to pain
- Itch
- Bleeding
- Discharge
- Dysuria and urinary frequency (also see
urinary tract infection)
- Bowel habit to exclude
constipation
- Pubertal stage (to assess for precocious puberty:
Tanner staging)
- Sexual history (including superficial dyspareunia in sexually active adolescents)
Examination
If relevant, examine non-genital areas first eg for evidence of systemic skin conditions
Perineal examination
Carefully consider the purpose / need for a perineal examination
- Discuss with a senior clinician
- If perineal examination is necessary, it should only be performed once, by the most suitable clinician
- Senior clinician should be present to supervise and/or chaperone along with the parent
- Provide explanation to the child and parent of the purpose of the examination and obtain consent
- Ensure privacy is maintained and discomfort and distress minimized
The perineum is best examined with the child supine (or semi-supine in a parent’s lap) in a frog-leg position: heels together, knees flexed and hips abducted; or lying on their side with knees drawn up to the chest
The child can assist with separating their labia if they prefer
Do not perform an internal vaginal examination or take internal vaginal swabs in prepubescent children. Discuss with senior clinician if felt necessary
Assess the perineum for
- Anatomy: labial adhesion, urethral prolapse, integrity of hymen and introitus (vaginal entrance)
- Colour: erythema (it is normal for prepubertal children to have mild erythema of the vulva), pale atrophic patches (lichen sclerosis), bruising
- Swelling, dryness, excoriation
- Discharge
- Bleeding
- Pain: using a cotton bud, gently touch the vulval skin, start laterally (away from the labia), moving towards peri-hymenal area. Altered sensation or pain whilst progressively approaching the peri-hymenal area is suggestive of vulvodynia
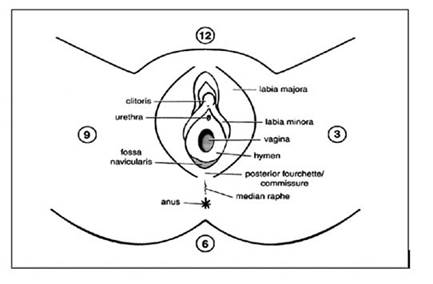
Carefully document examination findings (describe appearance rather than interpreting findings). Using a clock face diagram can be useful to describe the location (see figure above)
Offensive vaginal discharge and bleeding in pre-menstrual children may be suggestive of foreign body in vagina
|

|

|

|
|
Labial adhesion
|
Urethral prolapse
|
Lichen sclerosis
|
Investigations
- Investigations should be directed to the underlying cause
- If the cause is not clear or if there is concern for a vaginal foreign body, discuss with gynaecologist
- Consider urine MCS
- If profuse / offensive discharge: take a swab for MCS at the introitus (vaginal entrance), do not take internal vaginal swabs. See
Sexually transmitted infections to guide other possible investigations
Vulvovaginitis
- Clinical features: vulval discomfort, itch, dysuria, discharge and redness
- Causal factors:
- Normal prepubescent development
- Thin vaginal mucosa (secondary to lack of oestrogen)
- More alkaline pH (pH 7)
- Environmental
- Moisture (synthetic fibre underwear, tight clothing, wet swimming costumes, obesity)
- Poor hygiene
- Irritants (soap residue, bubble baths, fabric softeners, antiseptics etc)
- Infection:
- Foreign body
- In most cases no investigations are required
- Treatment
- Explanation / reassurance
- Avoid / address environmental causal factors above
- Encourage good hygiene and vulval care (See
Vulval skin care for children and
Vulval skin care for teenagers)
- Vinegar baths (add ½ cup white vinegar to a shallow bath and soak)
- Low dose steroid cream can be considered for severe itch/excoriation
- Pinworms
- Nocturnal vaginal shooting pain or itch
- Treat with mebendazole 50mg (> 6 months and ≤10 kg) or 100mg (>10 kg) oral single dose and repeat after 2 weeks
- Precautions to minimise spread including treatment of all household contacts (see
Worms)
- Bacterial overgrowth
- Significant erythema and pain caused by respiratory or enteric flora eg group A streptococci or E. coli
- Considertreatment with cefalexin. See
Local antimicrobial guidelines
-
Sexual abuse occasionally presents as vulvovaginitis and should be considered
- If persistent, recurrent or multiple presentations, discuss with gynaecology
Labial adhesions (labial fusion)
- Normal variant which develops from 3 months (not present at birth) and resolves spontaneously by 6 to 8 years old when oestrogen levels increase at puberty
- Occur when the medial edges of the labia minora become adherent due to a combination of thin vaginal mucosa (normal prepubescent state) and minor irritation
- Usually asymptomatic, rarely may present with urinary frequency and postvoid dribbling if urinary outflow obstruction
- Treatment
- Provided the child is able to void easily, no treatment is needed
- Majority resolve spontaneously, provide reassurance
- Other treatment options such as oestrogen creams or manual separation of adhesions (distressing and painful) have a high risk of recurrence, and are not recommended
- If there is urinary outflow obstruction, a short course of oestrogen cream may be considered, discuss with gynaecology
Lichen sclerosus et atrophicus
- Onset 5-7 years old, painless itch, bleeding or discharge; may be asymptomatic. Usually persists with episodic symptoms
- Pale atrophic patches on labia and perineum, which may be confluent and extensive
- Scratching and other minor trauma may lead to further inflammation and purpuric haemorrhage into the skin. Occasionally this is mistaken for sexual abuse
- Treatment
- Provide reassurance
- Avoid irritants eg soap residue, bubble baths, antiseptics
- Treat secondary
constipation
- Barrier ointments (eg paraffin, zinc paste) may help as a short-term measure
- Course of high potency (then medium potency) topical steroids is often required. Recommend specialist consultation
- Most cases resolve before puberty, but some may continue with problems into adult life
Vulvodynia
- May be generalised (involving the whole vulva) or localised to part of the vulva or perihymenal area
- May be provoked (caused by touch or any specific stimulus) or spontaneous (occurring without touch as a trigger)
- Management
-
Vulval care is key
- Pelvic floor physiotherapy can be effective
- Psychologist input if associated anxiety or depression
- Ensure any constipation is appropriately managed
- Medications
- Topical creams with local anaesthetic agent for short term relief only
- Consult specialist (gynaecology or pain) for advice on suitability of agents for neuropathic pain eg amitriptyline, gabapentin or pregabalin
- Complementary therapies such as acupuncture and hypnosis may also be helpful in some children
Urethral prolapse
- Chronic onset, bleeding, pain, dysuria, constant need to strain
- Treat precipitant eg cough, constipation
- Refer to gynaecology for assessment and consideration of topical oestrogen cream
Consider consultation with local paediatric team when
Consider consultation with local gynaecology team when
- Diagnosis unclear
- Further management advice needed
- Removal of suspected foreign body
If sexual assault is suspected, please refer to local guidelines. Early consultation with specialist services is vital
Consider transfer when
Concern for vaginal foreign body and local services unable to perform examination under anaesthetic
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
Diagnosis made and any required community follow-up is in place
Parent information
Vulval skin care for children
Vulval skin care for teenagers
Vulvovaginitis
Labial fusion
Vulval lichen sclerosus
Worms
Mott Children’s Hospital - vulvodynia
Additional notes
Prepubertal hymenal variations: Australian Family Physician 2011
Last updated November 2022