See also
Acute scrotal pain or swelling
Key points
- Most injuries are minor
- Consider analgesia +/- procedural sedation early for examination
- Although infrequently associated with non-accidental injury, if suspected, consult a senior doctor and consider advice from the forensic paediatric medical service
Background
Although most straddle injuries are minor, genital injuries in children often cause great anxiety because of the location and concern for future gynaecological and sexual development. The unoestrogenised pre-pubertal female genital tissues are friable (with excellent blood flow) and lack distensibility. Therefore, even minor trauma can cause injury and bleeding which may appear extensive.
Urogenital trauma frequently raises the question of non-accidental injury, however it is uncommonly associated with it. It is important to be able to correlate the history of the injury with physical findings on examination. Thorough documentation and appropriate referral of cases suspicious for abuse is a priority of care.
Assessment
History
- Mechanism of injury
- Timing and setting of injury
- First aid provided
- Inability to pass urine and faeces
- Other injuries
- Witnesses
- Consider if injury is consistent with history, is there a suspicion of non-accidental injury?
Examination
General assessment of the child looking for evidence of other injuries
Examination should be performed only once, therefore consider early involvement of a senior clinician. If suspicious of non-accidental injury contact the local forensic paediatric medical service (see contact details below)
Examination is usually performed in the supine frog-legged position. Explanation and gentle handling of the child is important. Consider analgesia +/- procedural sedation
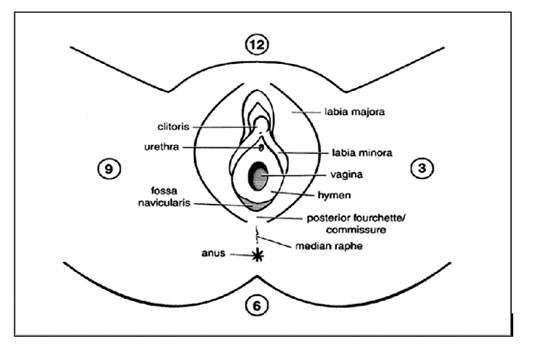
Document a detailed description of the injury. A clock face can often be used to describe the location of the injury (see diagram below)
Features to consider on examination
- Can the posterior or upper limit of the wound be seen? If not, examination under anaesthaesia should be considered
- Is there an expanding haematoma?
- Is there any anal or rectal involvement?
Management
General principles of care
- If suspicious of non-accidental injury contact the local forensic paediatric medical service (contact details below)
- Compression of bleeding with a clean dressing pad
- If there is significant vaginal bleeding in older adolescents, the vagina can be packed with a tampon or gauze
- Use ice packs to reduce bleeding and swelling (avoid directly overlying the clitoris)
- Irrigate the area with warm water
- Review tetanus status
Severity of Injury |
Treatment |
Follow up / Consultation |
Minor
Bleeding is minor or has stopped and the child can void spontaneously |
Salt water baths for comfort
Topical anaesthetic cream or barrier cream to reduce local pain on micturition
Reduction in strenuous activity for 24 hours to prevent re-injury
Simple analgesia |
GP |
Non-minor
Ongoing bleeding, laceration borders not visualised, labia minora tear, unable to void, clinician concern |
Management as above
Consider urethral catheter if unable to void eg in the presence of a large vulval hematoma |
Local paediatric team
Local gynaecology or surgical service |
Consider consultation with local paediatric team when
- Child has non-minor injury
- Child unable to pass urine
- Suspected non-accidental injury for forensic examination
Consider transfer when
Child requiring care beyond the comfort level of the local hospital
For emergency advice and paediatric or neonatal ICU transfers information, see Retrieval Services
Consider discharge when
Minor injury and able to pass urine
Parent information
Straddle injuries
Forensic Paediatric Medical Services
NSW The Child Protection Helpline 132 111
Child Protection Units:
- The Children’s Hospital at Westmead 02 9845 2434 / AH 02 9845 0000
- Sydney Children’s Hospital, Randwick 02 9382 1412 / AH 02 9382 1111
Queensland’s Child Protection and Forensic Medical Service
07 3068 2659 or 07 3068 2660 / AH 07 3068 1111
Victorian Forensic Paediatric Medical Service (VFPMS) 1300 66 11 42
Last Updated May 2020