* Approved by CPG Committee; PIC endorsement pending
See also
Diabetic ketoacidosis
Diabetes mellitus and surgery
Hypoglycaemia
Glucagon for severe hypoglycaemia
Diabetes mellitus: management of unwell children with established diabetes in hospital
Diabetes mellitus: new presentation
Key points
- Always request a ketone check in unwell children with established diabetes (ketone levels may be raised even in normoglycaemia)
- Never advise omission of basal or background insulin in children with diabetes, even when unwell, fasting or hypoglycaemic
- Consider nausea/vomiting as a sign of insulin deficiency in a child with established diabetes until proven otherwise
- Children with diabetes and ketones >3, especially if vomiting, are at high risk of diabetic ketoacidosis and likely require hospitalisation
- Issues with regular insulin regimens or longer-term glycaemic control should be referred to the child's usual diabetes care team during business hours
Background
- Clinicians commonly receive phone calls from parents/carers of children with diabetes with concerns and questions, especially out of business hours
- Most issues can be safely managed with the child at home using their usual insulin plan, but hospital presentation (+/- ambulance involvement) may be necessary
- Children with diabetes may become unwell due to an intercurrent illness, or in the setting of hyperglycaemia, hypoglycaemia and/or ketosis
- Insulin requirements may increase, leading to hyperglycaemia, if doses are not adjusted:
- in acute illnesses
- following surgical procedures
- during treatment with corticosteroids
- Insulin requirements may decrease, leading to hypoglycaemia, if there is
- limited oral intake
- increased losses eg gastroenteritis
- Hyperglycaemia, fever, excessive glycosuria and ketonuria all contribute to increased fluid losses, leading to risk of dehydration
Definitions
BGL and ketone interpretation in type 1 diabetes
|
BGL |
Ketones |
| Hypoglycaemia |
≤3.9 mmol/L |
|
| Normal pre-meals |
4-7 mmol/L |
<0.6 mmol/L |
| Normal post-meals |
4-10 mmol/L |
<0.6 mmol/L |
| High |
>11 mmol/L |
≥0.6 mmol/L |
| Very High |
>15 mmol/L
(check ketones) |
>1 mmol/L
(insulin required) |
Assessment
History over the phone
- Child's age
- Reason for call eg hypoglycaemia, hyperglycaemia, elevated ketones, illness etc
- Duration of type 1 diabetes mellitus (T1DM), how long since diagnosis
- Current insulin brand, dosage and insulin regimen eg fixed versus flexible
- Typical total daily dose (TDD) of insulin
- Weight
- Blood glucose level (BGL) and blood ketone levels over the previous 1-2 days
- Nature of illness and symptoms
- Consider other precipitants for
- Hypoglycaemia
- excessive insulin dosing/recent dose increase
- missed meals
- exercise
- alcohol ingestion
- Hyperglycaemia
- insulin omission/recent dose decrease
- poor insulin adherence
- dietary factors
- new medications eg steroids
- problems with injection method
- problems with injection site (lipoatrophy/lipohypertrophy)
- Ability to tolerate oral fluids/food
- Usual sick day management plan: families will have centre-specific resources on management of their diabetes. Always encourage families to review this information in the first instance
- Distance from hospital
Management
Home management of unwell child with established diabetes
Note: some centres use different management guidelines, see local protocols
- Suggest increased monitoring of BGL
- Confirm any continuous glucose monitoring (CGM) readings with finger prick BGL, especially if BGL
<4 mmol/L or>10 mmol/L
- Use finger prick BGL measurements to direct management steps
- At least 2-4 hourly finger prick BGL for children without CGM, including overnight
- BGL 1-2 hourly if more unwell
- Advise on treatment of hypoglycaemia or hyperglycaemia. See flowchart below
- Check ketones; extra insulin may be required if ketones are elevated
- Provide advice for managing the underlying illness at home eg fever, viral illness, gastroenteritis
- Encourage maintaining hydration
- If BGL
<14: encourage sugar-containing fluids eg diluted juice, electrolyte drinks
- If BGL ≥14: encourage sugar-free fluids
- Plan follow up
- Continue 2-4 hourly BGL and ketone checks and respond accordingly
- Advise parent/carer to contact the child's usual diabetes care team during business hours, or to present to ED if ketones are rising, ongoing hypoglycaemia or uncontrolled hyperglycaemia despite treatment
Home management of unwell child with T1DM on multi-daily injections
.png)
Home management of hypoglycaemia in the unwell child with diabetes
- Do not advise to omit insulin, even in the setting of hypoglycaemia/illness
- Always check ketones in an unwell child with diabetes. Hypoglycaemia with ketones >0.6 mmol/L suggest insulin and carbohydrate deficiency and warrants urgent medical attention
- Children on an insulin pump may require a temporary (lower) basal rate to 70% of their normal rate. See child's individual management plan in the first instance
- See Additional notes for glucagon and minidose glucagon dosing
Home management of hypoglycaemia in the unwell child with diabetes
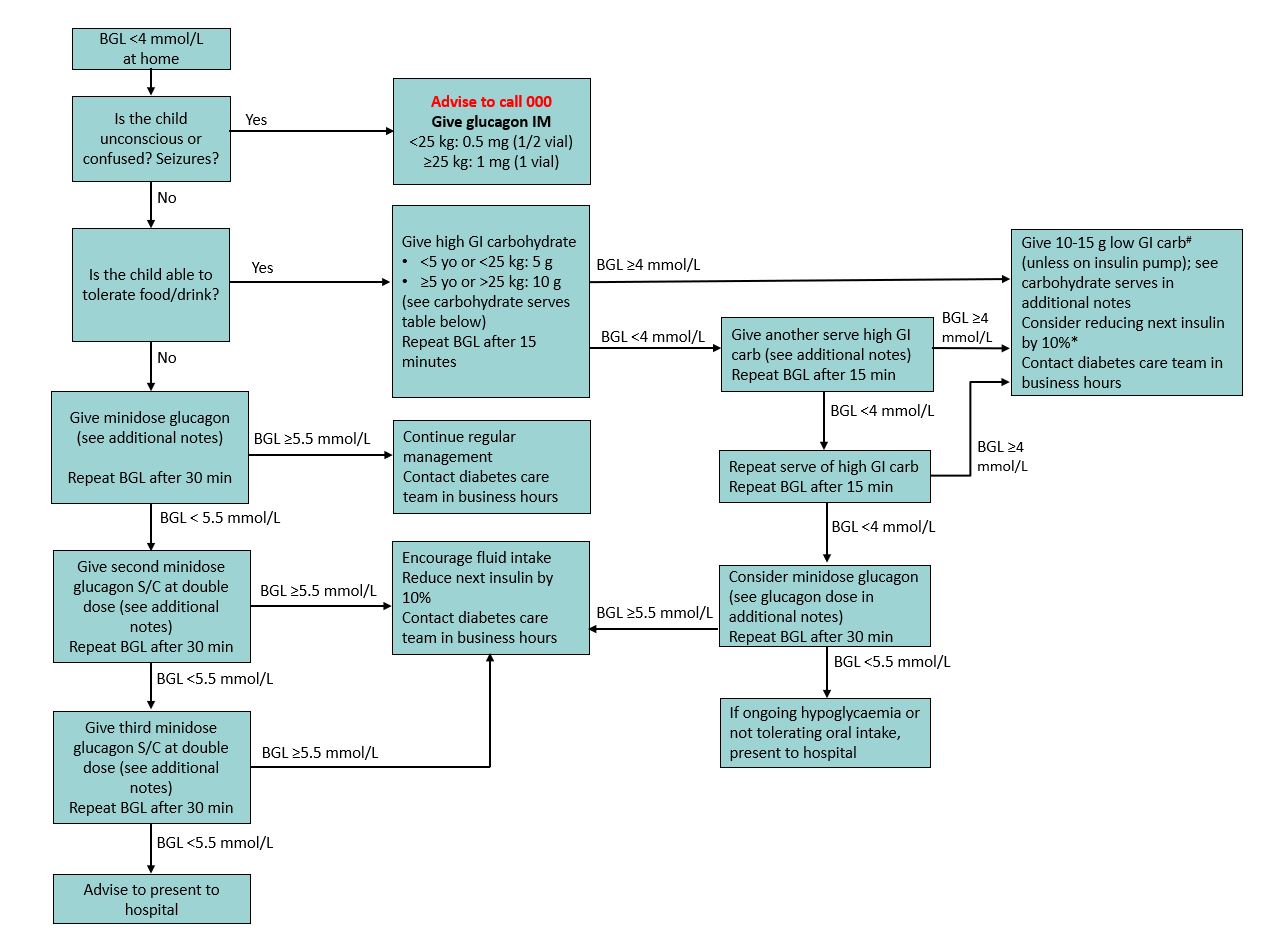
# If hypoglycaemia occurs and is treated directly before/at mealtime, encourage regular meal with regular insulin (instead of 10-15 g carbohydrate), unless child having recurrent hypoglycaemic episodes. Do not count carbohydrates given for hypoglycaemia
treatment immediately prior to a meal in the meal-time carbohydrate count.
*Reduce next dose insulin by 10% if BGL
<4 on more than one occasion
Home management of ketonaemia in the unwell child with diabetes
Hyperglycaemia with ketones <0.6
- Treat as per the child's usual insulin treatment plan
- Most children should be advised to give an insulin correction with their next rapid-acting insulin dose eg mealtime
Hyperglycaemia with ketones ≥0.6
- Indicates insulin deficiency
- Treat with additional insulin bolus as per the flowchart below
- Concerning signs that the child requires urgent medical review for DKA include:
- Ketones >3, especially with vomiting and/or abdominal pain
- Rapid breathing
- Drowsiness or altered conscious state
- Rising ketones (especially if >1.5) despite additional insulin boluses
Hypoglycaemia with ketones ≥0.6
- Suggests both carbohydrate and insulin deficiency
- Commence hypoglycaemia treatment as above
- Requires hospital presentation for fluid and insulin treatment
Home management of hyperglycaemia and ketonaemia in the unwell child on insulin injections
.png)
*TDD = total daily dose, based on typical daily dosing schedule. If family unaware/unsure of usual doses, estimate TDD using 1 unit/kg based on most recent weight
¹For insulin pump users, additional bolus insulin should be given via subcut injection, and their pump resited
Advice for children on insulin pumps
- Please see child's individual management plan in the first instance
- Children on pumps receive only rapid-acting insulin and are therefore at high risk of DKA if the pump fails or is disconnected
- If BGL persistently elevated or ketones ≥0.6
- Check for problems with the pump or delivery system (eg kink in catheter, air in infusion line, disconnection at insertion site, insertion site irritation)
- Change the catheter, tubing and insulin reservoir
- If BGL >15, treat as pump failure
- Give supplemental insulin as a subcutaneous injection, see below.
- Following an insulin bolus, ketones may increase for 1-2 hours but are then expected to decrease if treated correctly
- For persisting hypoglycaemia whilst unwell, a temporary basal rate of 70% of normal may be required, with ketone monitoring
Home management for unwell child with hyperglycaemia on insulin pump
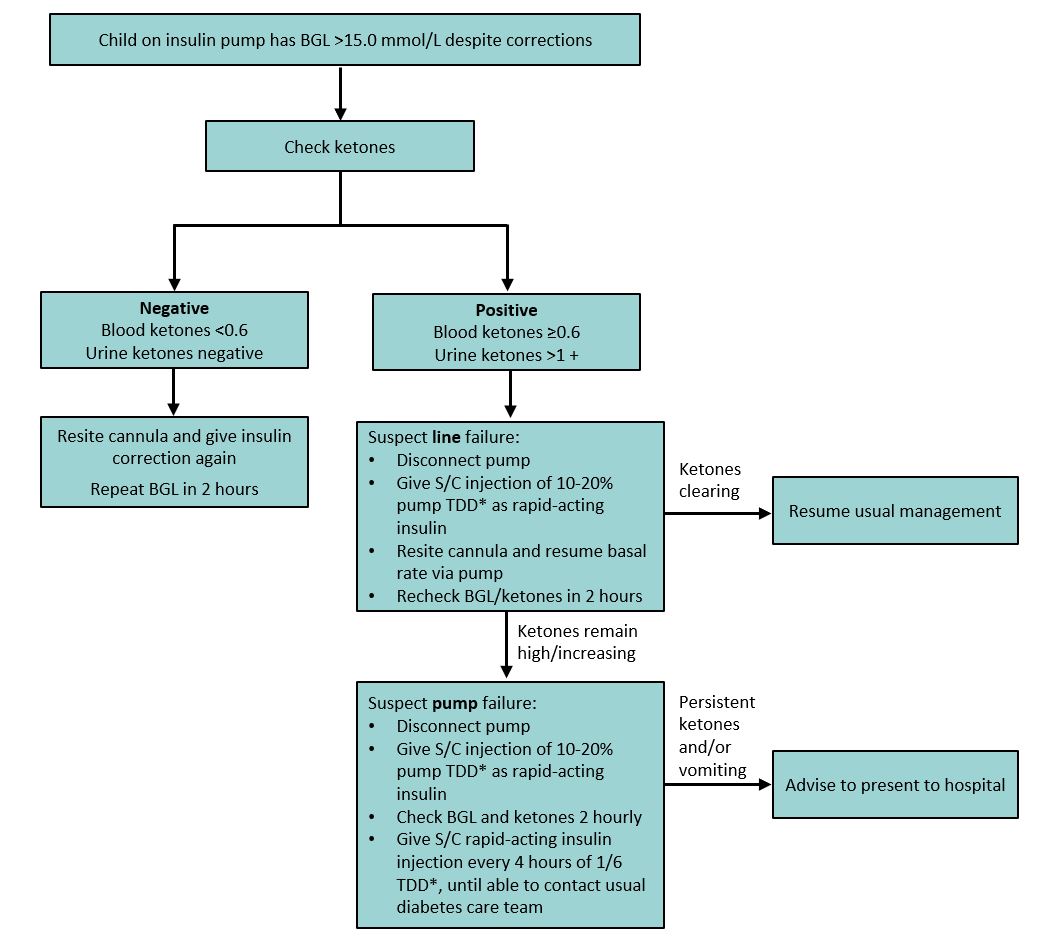
*TDD = total daily dose, based on typical daily dosing schedule. If family unaware/unsure of usual doses, estimate TDD using 1 unit/kg based on most recent weight
Advise presentation to the nearest emergency department when
- Inability to maintain BGL >4 mmol/L despite treatment as per hypoglycaemia flow chart
- BGL remains
<5.5 mmol/L despite 3 minidoses of glucagon
- Ketones persist >0.6 mmol/L and child is vomiting/unable to tolerate oral intake
- Ketones >3 mmol/L at any time
- Inability to maintain hydration at home eg limited oral intake, ongoing losses
- Child is confused, lethargic, suffering severe abdominal pain
- The child deteriorates or their underlying condition is unclear
Troubleshooting other common diabetes concerns over the phone
| Concern |
Advice |
Action |
| 'I've run out of insulin' |
Never advise skipping a dose of insulin |
See GP for script, or send script to local pharmacy or hospital for parent to fill |
| 'I've given my child the wrong dose' |
Provide reassurance |
- If too much, give extra serve of carbohydrates and recheck BGL
- If too little, check BGL and ketones, and monitor. Extra insulin may be required
|
| 'I'm not sure I injected all the insulin' |
Provide reassurance |
Check BGL and ketones |
| 'My child is having a seizure' |
- Give glucagon IM
- Call '000' for an ambulance
- Check BGL
|
Glucagon dose
-
<25 kg: 0.5 mg (½ vial)
- >25 kg: 1 mg (1 vial)
|
| 'My child just had a seizure' |
- Call '000' for an ambulance
- Check BGL
|
Follow hypoglycaemia flowchart if applicable |
| 'I think my insulin pump line is blocked' |
Follow line failure advice |
- Check BGL and ketones
- See advice for children on insulin pumps above
|
| 'I think my insulin pump is faulty' |
Disconnect pump
Check BGL and ketones |
- If within normal range, give 1/6 total daily dose by rapid-acting insulin injection every 4 hours until review by diabetes care team
- If elevated, see Advice for child with hyperglycaemia on insulin pump flowchart above
|
| 'I'm wearing a continuous glucose monitor and it's beeping or has dislodged' |
Remove and return on next working day |
Monitor finger prick BGLs |
| 'My child has diabetes and has just been drinking or taken drugs' |
Ensure food and water intake before bedtime |
Check BGLs more frequently overnight |
Additional notes
Calculating total daily dose (TDD) Insulin
This is all the insulin (rapid and long-acting) that a child has in a day.
For example: Background glargine 20 units at night, breakfast short-acting bolus typically 8 units, lunch bolus 12 units, dinner bolus 18 units, snack bolus 2 units.
Therefore, TDD = 20+8+12+18+2 = 60 units
If the child uses flexible dosing strategies or family are unaware/unsure of usual doses, estimate TDD using 1 unit/kg based on most recent weight
| Total daily dose (TDD) |
Sick day dose
(rapid-acting insulin in addition to usual doses) |
|
10% |
20% |
| 1-10 units |
1 unit |
2 units |
| 10-15 units |
1.5 units |
3 units |
| 15-20 units |
2 units |
4 units |
| 20-25 units |
2.5 units |
5 units |
| 25-30 units |
3 units |
6 units |
| 30-35 units |
3.5 units |
7 units |
| 35-40 units |
4 units |
8 units |
| 40-45 units |
4.5 units |
9 units |
| 45-50 units |
5 units |
10 units |
| 50-55 units |
5.5 units |
11 units |
| 55-60 units |
6 units |
12 units |
| 60-65 units |
6.5 units |
13 units |
| 65-70 units |
7 units |
14 units |
| 70-75 units |
7.5 units |
15 units |
| 75-80 units |
8 units |
16 units |
Carbohydrate serves in treatment of hypoglycaemia
| High GI carbohydrate serves |
Low GI carbohydrate serves |
5 grams
If
<5 yo or <25 kg |
10 grams
If >5 yo or >25 kg |
10-15 grams |
Glucose tablets (1 TRUEplus or 3 Glucodin)
50 mL lemonade
100 mL cordial
1 teaspoon honey
2 jellybeans
60 mL juice |
Glucose tablets (3 TRUEplus or 6 Glucodin)
100 mL lemonade
200 mL cordial
2 teaspoon honey
3 jellybeans
120 mL juice |
4-6 savoy biscuits
7-10 rice crackers
1 slice of bread
200-250 mL plain milk
½ cup fruit yoghurt
1 apple
1 small banana |
Intramuscular glucagon dosing for severe hypoglycaemiaIf child confused, unconscious or having a seizure
- Inject 1 mL of H2O into the vial containing glucagon 1 mg, gently agitate to dissolve
- Use a syringe to draw up the entire solution (1 mL) from the vial and administer dose depending on weight
-
<25 kg: give 0.5 mg (half of vial, 0.5 mL)
- >25 kg: give 1 mg (full vial, 1 mL)
- See Glucagon for severe hypoglycaemia
|
Subcutaneous minidose glucagon for rescue hypoglycaemia
- Minidose glucagon is used to manage hypoglycaemia (BGL
<4 mmol/L) in a child with diabetes, when usual oral treatments have been unsuccessful or cannot be tolerated, but the child does not have CNS impairment
- Minidose glucagon avoids the side effects of larger doses of glucagon such as nausea and vomiting
- This can allow the child time to recover sufficiently to tolerate sips of sugar-containing fluid and avoid ED presentation/hospital admission
Minidose glucagon administration
- Make up glucagon as directed
- Re-constitute the full 1 mg vial in 1 mL of sterile water and then use an insulin syringe to draw up to the 1 'unit' mark on the insulin syringe.
- 1 unit = 10 microg of reconstituted glucagon solution
Minidose glucagon - initial doses for subcutaneous administration
| Age (years) |
Dose of glucagon |
Mark on insulin syringe |
|
<2 |
20 microg (0.02 mg) |
2 unit mark |
| 2-15 |
10 microg per year of age |
1 unit per year of age |
| >15 |
150 microg (0.15 mg) |
15 unit mark |
Minidose glucagon ongoing management
- Check BGL at 30 minutes
- If ≥5.5 mmol/L, check BGL hourly, reduce next insulin by 10%
- If
<5.5 mmol/L, give 2nd minidose of glucagon at double initial dose (eg if 5 units initially, give 10 units for second dose)
- Check BGL again after 30 minutes
- If
<5.5 mmol/L, give 3rd minidose of glucagon at double initial dose
- If BGL remains
<5.5 mmol/L after 3rd dose, advise to present to hospital
- After glucagon is reconstituted, keep in refrigerator and discard after 24 hours
Note: If the child remains unwell and oral intake is reduced, subsequent doses of insulin may also need to be adjusted as per sick day plan
Parent information
Diabetes at the RCH : Type 1 diabetes toolkit
National Diabetes Services Scheme: sick days
Last updated July 2025
Reference List
- Beckles, Z. L., Edge, J. A., Mugglestone, M. A., Murphy, M. S., & Wales, J. K. Diagnosis and management of diabetes in children and young people: summary of updated NICE guidance. Bmj. 2016. 352.
- Craig, M. E., Twigg, S. M., Donaghue, K. A., Cheung, N., Cameron, F., Conn, J., & Silink, M. National evidence-based clinical care guidelines for type 1 diabetes in children, adolescents and adults. 2011. Australian Government Department
of Health and Ageing. Canberra.
- Mayer-Davis, E. J., Kahkoska, A. R., Jefferies, C., Dabelea, D., Balde, N., Gong, C. X., & Craig, M. E. ISPAD Clinical Practice Consensus Guidelines 2018: Definition, epidemiology, and classification of diabetes in children and adolescents.
Pediatric diabetes. 2018. 19(Suppl 27), 7-19.
- Phelan, H., Hanas, R., Hofer, S. E., et al. Sick day management in children and adolescents with diabetes. Pediatr Diabetes. 2022. 23(7), 912-925. doi:10.1111/pedi.13415.
- RCH. Diabetes at the RCH: How to treat low blood glucose levels. Retrieved from https://www.rch.org.au/diabetes/type-1-diabetes-toolkit/How_to_treat_low_blood_glucose_levels/ (viewed 25 November 2022).
- Tauschmann, M., Forlenza, G., Hood, K., Cardona-Hernandez, R., Giani, E., Hendrieckx, C., DeSalvo, D. J., Laffel