See also
Asthma
Dehydration
High flow nasal prong therapy
Oxygen delivery
Key points
- Bronchiolitis is a clinical diagnosis. Investigations are not indicated
- The goal of management is to maintain hydration and oxygenation. Medication beyond simple analgesia is not indicated
- Infants with a history of prematurity or cardiopulmonary disease are at higher risk of deterioration and are more likely to require admission
- Use nasal prong oxygen for persistent SpO2
<90%. High flow nasal prong (HFNP) therapy should be reserved for failure of nasal prong supplemental oxygen
Background
- Bronchiolitis is a viral lower respiratory tract infection, generally affecting children
<12 months of age
- It is a clinical diagnosis, based on typical history and examination findings
- Peak severity is usually at around day 2-3 from the onset of increased work of breathing, with resolution over 7-10 days, but disease course may vary
- It is self-limiting, usually requiring no treatment or intervention
- A cough may persist for weeks
Assessment
History
Bronchiolitis typically begins with a coryzal prodrome followed by onset of one or more of:
- Cough
- Fever
- Difficulty feeding
- Apnoeic episodes
- Unsettledness/irritability
Risk factors for more serious illness
Consider hospital admission for these children, even if presenting early in illness with mild symptoms
- Chronic lung disease
- Congenital heart disease
- Chronic neurological conditions
- Gestational age
<37 weeks, or chronological age at presentation <10 weeks
- Growth restriction
- Indigenous ethnicity
- Immunodeficiency
- Exposure to cigarette smoke
- Trisomy 21
Examination
Management
Investigations
In most children with bronchiolitis, no investigations are required or recommended
Investigations should only be undertaken when there is deterioration or diagnostic uncertainty (eg cardiac murmur with signs of congestive cardiac failure)
- Chest X-ray (CXR) is not indicated and may lead to unnecessary treatment with antibiotics. CXRs cannot discriminate between viral and bacterial infections and are poorly reproducible in this age group
- Blood tests are not indicated (including blood gas, FBE, blood cultures)
- Virological testing (nasopharyngeal swab or aspirate) is not indicated in the management of individual children and should not be used to guide treatment
Treatment
The main treatment of bronchiolitis is supportive. This involves ensuring appropriate oxygenation and fluid intake, and
minimal handling
Some young infants with risk factors (see above) or apnoeas (absence of breathing for >15 seconds, often associated with bradycardia and/or oxygen desaturation) may benefit from a period of hospital observation, even if they do not require fluid or supplemental oxygen therapy.
Bronchiolitis management approach
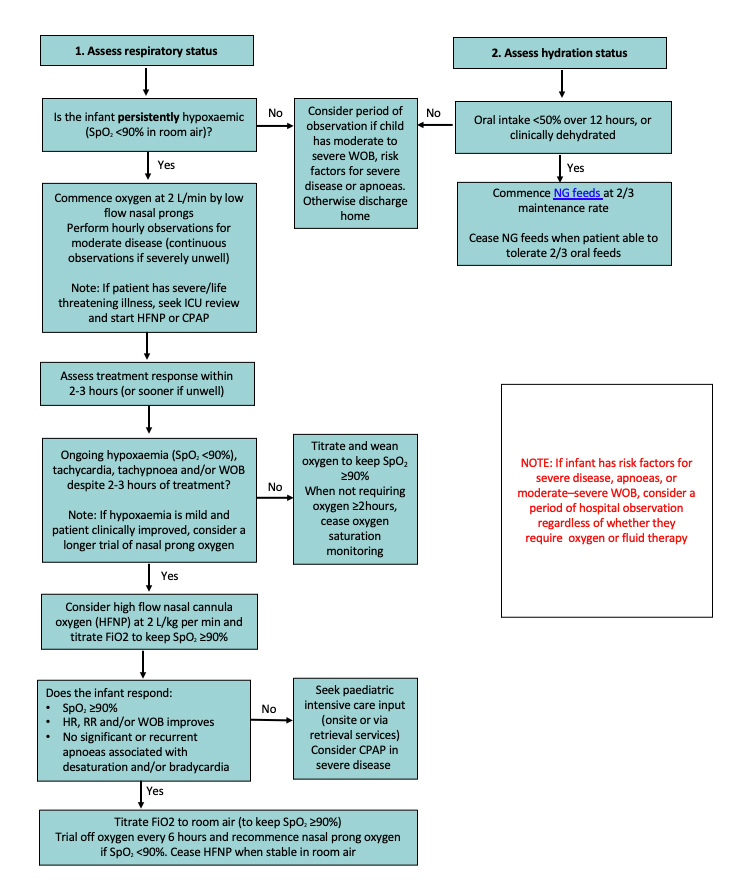
Supplemental Oxygen
- Target SpO2 is 90%, unless the child has an underlying cardiopulmonary disease with specific SpO2 targets
- Infants with bronchiolitis will have brief episodes of mild/moderate desaturations
<90%. These brief desaturations are not a reason to commence supplemental oxygen
- Nasal prong oxygen should only be instituted when oxygen saturations are persistently
<90%. If oxygen saturations remain persistently <90% and there is no improvement in respiratory state despite 2 hours of low flow oxygen, consider HFNP
- HFNP is not recommended in children with SpO2 consistently ≥90%
- Titrate oxygen down to achieve target SpO2 ≥90%. Aim to use minimum supplemental oxygen. It is unnecessary to aim for SpO2 in mid-high 90’s
- Trial off supplemental oxygen (nasal prong or HFNP) every 6 hours. Recommence nasal prong oxygen if SpO2 remains
<90%
- Once no longer requiring supplemental oxygen for 2 hours, discontinue oxygen saturation monitoring. Continue observations 2-4 hourly and reinstate intermittent oxygen monitoring if clinically deteriorating
Hydration/nutrition
- Children are often more settled if comfort oral feeds are continued
- When non-oral hydration is required, nasogastric (NG) hydration is the route of choice and can be safely used in children on respiratory support
- NG bolus feeding is safe and should be commenced at two-thirds maintenance rate because of
potential for increased ADH secretion
- IV hydration should be reserved for children in whom NG feeding is not possible. If IV fluid is used it should be isotonic with added glucose. See
IV fluids
Medication
- Beyond simple analgesia, medications are not routinely indicated
- Chloral hydrate may be used to reduce agitation in children with worsening respiratory distress, regardless of need for respiratory support. It is most effective in children <2years and <15kg
- Dose 0-2 years: 10mg/kg initial dose, every 4-6 hours
May increase to 15mg/kg and then up to 20mg/kg every 4-6 hourly if required, but recommend increased monitoring and senior clinician involvement is required outside of critical care areas - Adverse effects: excess sedation, respiratory depression, hypotension, paradoxical agitation
- Caution in patients with renal or hepatic impairment
- There is insufficient evidence for the use of caffeine in prevention of bronchiolitis-associated apnoea
Do not administer
- Beta-2 agonists, including in infants with a personal or family history of atopy
- Corticosteroids (nebulised, oral, intramuscular or intravenous)
- Adrenaline (nebulised, intramuscular or intravenous) except in peri-arrest or arrest situation
- Nebulised hypertonic saline
- Antibiotics, including azithromycin
- Antivirals
- Caffeine
Nasal suction
- Deep nasal suction beyond the nasopharynx is not recommended. Superficial nasal suction may be considered in those with moderate disease to assist feeding
- Nasal saline drops may be considered at time of feeding
Chest physiotherapy
Consider consultation with local paediatric team when
- Child has specific risk factors (detailed in assessment section)
- Requiring supplemental oxygen
- Less than half normal oral intake and clinically dehydrated
- Respiratory status assessed as
moderate or severe
Consider transfer when
-
Severe bronchiolitis (see above)
- Risk factors for more severe illness
- Child requiring care above the level of comfort of the local hospital
- Child has oxygen requirement on HFNP with FiO2 >50%
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Considerations for discharge
- Infants can be discharged when SpO2 ≥90% and feeding is adequate
- Infants
<8 weeks of age are at increased risk of representation
- Transfer to Hospital in the Home (HITH) on home oxygen can be considered after a period of observation in selected infants as per local policies
- Parents should be educated about the illness, the expected progression and when and where to seek further advice
Parent information
RCH Kids Info
Bronchiolitis
Last updated November 2023