See also
Intravenous fluids
Dehydration
Gastroenteritis
Enteral feeding and medication administration (RCH nursing guideline)
Key points
- Whenever possible the enteral route (oral or nasogastric) should be used for fluids
- Shocked children require Intravenous (IV) resuscitation – see
Resuscitation: care of the seriously unwell child
- Serial weights are the best measure of acute changes in fluid status
- Rehydration treats dehydration, not the underlying cause. Careful and regular clinical review is required
Background
- Nasogastric (NG) fluids are a safe and effective method of maintaining hydration and correcting dehydration in most children, and are generally well tolerated in pre-school age children
- Advantages over IV fluids include safety (less risk of electrolyte derangement), more rapid recovery from gastroenteritis, and the option to give nutritional fluids eg expressed breast milk (EBM) or formula
- Neonates have specific fluid requirements, which are not covered by this guideline
- This guideline only applies to rehydration or maintenance fluids for short periods of time – for long term nasogastric feeding please seek specialist guidance
Assessment
Indications for nasogastric fluids
- Rehydration in the setting of gastrointestinal losses, or a period of sustained inadequate intake (see
Dehydration to assess degree of dehydration)
- Maintenance fluids where acute illness interferes with usual intake eg bronchiolitis, gingivostomatitis, viral infection
- Replacement of ongoing losses
Contraindications for nasogastric fluids
- Child who is 'nil by mouth' or fasting
- Shock
- Possible bowel obstruction: Bilious vomiting, severe abdominal distension, ileus
- Altered conscious state, or the critically unwell child
- Facial trauma, suspected base of skull fracture
Red flags
Children with the following features should be discussed with a senior clinician
- Very young (<6 months)
- Severe dehydration, electrolyte abnormalities or hypoglycaemia
- High risk of increased anti-diuretic hormone secretion - especially acute CNS and pulmonary conditions - although any unwell child is at risk
- Short gut or other chronic gastrointestinal disorder
- Situations where specialised fluid management is required, eg diabetes, cardiac, metabolic and renal conditions
- Craniofacial abnormalities
Management
Investigations
- Usually no investigations are needed, unless required for the underlying condition
- Consider glucose and electrolyte monitoring in young infants, and those with ongoing significant losses or nasogastric fluid support requirement beyond the initial 4-6 hour rehydration phase. Oral rehydration solution (ORS, eg GastrolyteTM, HYDRAlyteTM, PedialyteTM) is hypotonic and hyponatraemia can occasionally occur
Treatment
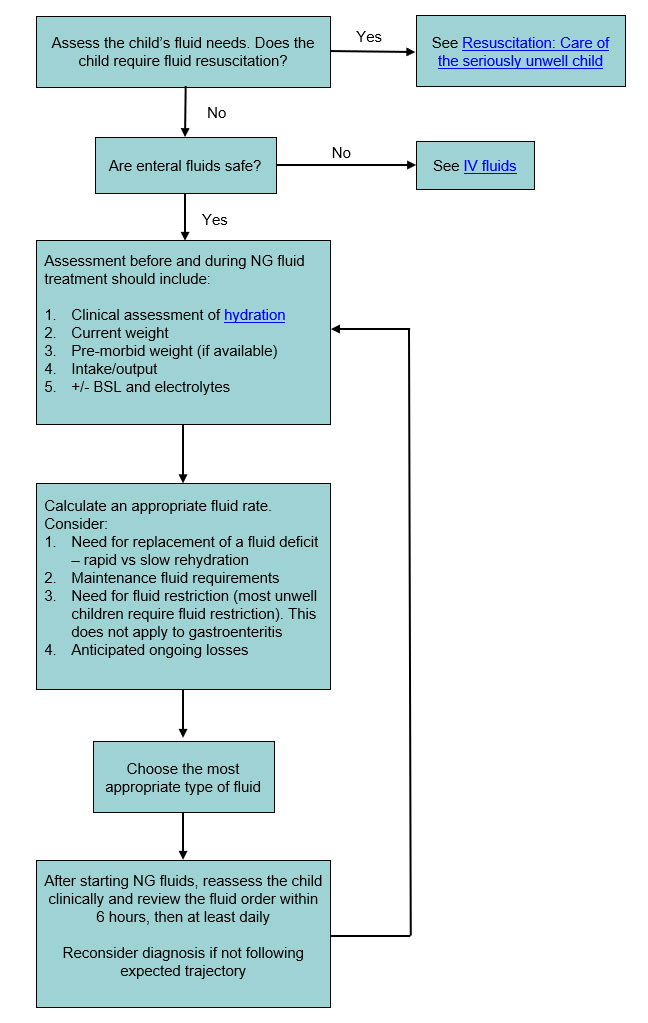
See Flowchart for
approach to prescribing NG fluids
1. NG Tube (NGT) insertion
(see RCH nursing guideline)
- NGT position is confirmed by an acidic gastric aspirate (pH 1-5): NGT should NOT be used if this is not achieved
- CXR is only required if there is uncertainty about placement
2. Choice of fluid
Rehydration
- ORS should be used for rehydration in all children over 1 month of age
- While electrolyte content and palatability may differ, there is no clinically significant difference between available ORS
Maintenance
- An infant who is milk fed should resume their usual feed type (EBM or formula) for maintenance hydration once rehydration is complete, orally or via NGT if unable to drink.
- Cease any fortification (eg concentrated formula or additives) in gastrointestinal illness as higher osmotic load may lead to increased diarrhoeal losses. Consider risk of electrolyte derangement if fortified feeds continued in other illnesses
-
Older children should also transition from ORS to age-appropriate nutrition as soon as possible. ORS can be used as a short-term maintenance fluid if a child is not tolerating oral intake
- If Specialised fluids or longer-termenteral nutrition are required consult with relevant specialty team or dietetics
3. Calculation of volume and rate
Fluid restriction
Two-thirds maintenance is appropriate for most unwell children requiring hydration support, particularly in respiratory and CNS infections.
Full maintenance
Full maintenance fluids may be appropriate for children who are not drinking adequately (eg acute viral infections), and in the maintenance phase of gastroenteritis
- The calculation of maintenance fluid requirements by the '4, 2, 1 rule' (see maintenance fluid requirements table below) provides adequate enteral hydration, but may be substantially less than the usual feeds that a well infant takes
- Younger babies need a higher volume of enteral milk (150–200 mL/kg/day –
see table below flowchart) to meet nutritional and growth requirements, but this higher volume should not be used as a basis for maintenance fluid prescribing in unwell children
- Infants can return to their usual feed volumes in mild illness or in the recovery phase
Maintenance fluid requirements calculated by the '4,2,1 rule'. Most unwell children require approximately 2/3 this amount
Weight (kg) |
Full Maintenance mL/day |
mL/hour |
|
3 to 10 |
100 x weight |
4 x weight |
|
10 - 20 |
1000 plus 50 x (weight-10) |
40 plus 2 x (weight-10) |
|
20 – 60 |
1500 plus 20 x (weight-20) |
60 plus 1 x (weight-20) |
|
>60 |
2400 mL/day is the normal maximum amount |
100 mL/hour |
4. Replacement of deficit based on
hydration assessment
Administration
NG fluids can be run continuously (rapid or slow) or as bolus feeds, depending on the clinical scenario
- Continuous feeds may be better tolerated where there is respiratory distress, vomiting or diarrhoea
- Bolus feeds at age and condition-appropriate intervals are often well tolerated and can provide comfort (eg 3 hourly feeds in mild-moderate bronchiolitis, or in recovery phase)
- Breast feeding can usually continue during both rapid and slow rehydration
Rapid Nasogastric Rehydration
Used to correct moderate dehydration in common illnesses where the goal is to expedite clinical improvement for discharge to home care (eg gastroenteritis).
- Not suitable for children with dehydration from respiratory illnesses, meningitis or significant electrolyte abnormalities
- Not suitable if
<6 months, significant comorbidities present, or abdominal pain. See slow nasogastric rehydration section below
- Children with severe dehydration need IV fluid resuscitation
- Use ORS at 10-25 mL/kg/hr for 4 hours (See hourly rate range table below).
- There is limited evidence regarding the rate of rapid nasogastric rehydration that is both safe and effective
- A range is provided as local practices and protocols regarding maximum rehydration rate vary
- Use clinical judgment (see
dehydration) and seek senior clinician support if unsure
Hourly rate range for rapid nasogastric rehydration (Not IV)
|
Weight on Admission |
10 mL/kg/hr
(replace 4% deficit) |
25 mL/kg/hr
(replace 10% deficit) |
Total infusion time |
|
7 kg |
70 mL/hr |
175 mL/hr |
4 hrs |
|
8 kg |
80 mL/hr |
200 mL/hr |
4 hrs |
|
9 kg |
90 mL/hr |
225 mL/hr |
4 hrs |
|
10 kg |
100 mL/hr |
250 mL/hr |
4 hrs |
|
12 kg |
120 mL/hr |
300 mL/hr |
4 hrs |
|
14 kg |
140 mL/hr |
300 mL/hr* |
4 - 4.5hrs* |
|
16 kg |
160 mL/hr |
300 mL/hr* |
4 - 5.5 hrs* |
|
18 kg |
180 mL/hr |
300 mL/hr* |
4 - 6 hrs* |
|
20 kg |
200 mL/hr |
300 mL/hr* |
4 - 6.5 hrs* |
* Maximum rate of many NG pumps is 300 mL/hr. If rate exceeds pump maximum rate, then divide target volume of fluid by 300 mL eg for 18kg child, if aim is 450 mL/hr for 4 hours (1800 mL), then this can be given as 300 mL/hr for 6 hrs
Slow Nasogastric Rehydration
- Preferred in children with moderate dehydration and conditions where high/rapid fluid volumes are not appropriate
- In the first 24hrs: replace 5% fluid deficit over the first 6 hours. Clinically reassess, and if ongoing hydration support is required give daily maintenance volume over the next 18 hours. To calculate rate, see Slow Nasogastric Rehydration table below.
- Subsequent 24 hrs: Replace remaining deficit if still indicated, in addition to daily maintenance volume
Recommended hourly rate for slow nasogastric rehydration
|
Weight on Admission |
Rate of slower NG rehydration
(Moderate dehydration – replaces 5% deficit plus maintenance) |
|
Weight |
mL/hr
0 – 6 hrs
(Deficit replacement – based on 5% deficit) |
mL/hr
7 – 24 hrs
(Full 24-hour maintenance volume, over remaining 18 hours) |
|
3 kg |
25 |
15 |
|
4 kg |
35 |
20 |
|
5 kg |
40 |
25 |
|
6 kg |
50 |
30 |
|
7 kg |
60 |
40 |
|
8 kg |
70 |
45 |
|
9 kg |
75 |
50 |
|
10 kg |
85 |
55 |
|
12 kg |
100 |
60 |
|
15 kg |
125 |
70 |
|
20 kg |
165 |
80 |
|
30 kg |
250 |
95 |
After Rehydration
- Aim for a rapid return to age appropriate fluids and nutrition. Breast-feeding should continue
- There is no benefit to gradual reintroduction of milk after rehydration, nor to giving dilute milk or formula
- Usually no dietary restrictions are required. If increased diarrhoeal losses after lactose-containing or high fructose fluid and foods, consider a 1-2 week period of lactose free milk / formula and avoidance of fruits/juice
Replacement of ongoing losses:
- In addition to maintenance rates, consider the need for replacement of ongoing losses including diarrhoea, vomiting, drain output
- Losses can be replaced mL for mL with ORS. Calculations may be based on each previous hour or each 4 hour period, depending on the situation eg 200 mL of diarrhoea over 4 hours can be replaced with ORS at 50 mL/hr over the next 4 hour period
5. Fluid balance
- Assessment of hydration status at least daily is required to titrate nasogastric fluid requirements
- Repeated weights are the best measure of fluid status. Weight should be taken at the start of treatment and then at least daily. In addition, document inputs and ongoing losses (including urine output), with at least 12 hourly subtotals
- If vomiting occurs, slow fluids temporarily and consider ondansetron if ≥6 months age (see
Vomiting)
- If significant abdominal pain or ongoing vomiting seek senior clinician review
Consider consultation with local paediatric team when
- Severe dehydration
- Electrolyte or glucose abnormalities
Consider transfer when
Children requiring care above the level of comfort of the local hospital.
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services.
Additional notes
Approach to prescribing nasogastric fluids
Standard enteral fluid volumes to meet nutritional and growth requirements (should NOT be given to most unwell children)
|
Age (months) |
mL/kg/day |
|
0-3 months |
150-200 |
|
4-6 months |
130-150 |
|
7-9 months |
120-150 |
|
10-12 months |
90-100 |
Last updated February 2021