Anaphylaxis
See also
Key points
- The World Allergy Organization Anaphylaxis Committee definition of anaphylaxis is:
A serious systemic hypersensitivity reaction that is usually rapid in onset and may cause death
Severe anaphylaxis is characterised by potentially life-threatening compromise in:
- Airway, breathing and/or circulation
- May occur without typical skin features or circulatory shock being present
- Initial treatment is to remove the allergen if possible and give IM adrenaline
- In children with possible anaphylaxis and known asthma, always give adrenaline first, then asthma medications
- Position is important. Lay child flat or sitting with legs extended – do NOT allow to stand or walk for at least 1 hour after symptoms have resolved

(This image has been reproduced with permission from the ASCIA website)
Background
- As anaphylaxis is a clinical diagnosis, emergency treatment should be guided by clinician judgement rather than a precise definition
- Respiratory symptoms predominate in children, and may resolve prior to any treatment or hospital arrival, but should still be recognised to avoid missed diagnosis
- Gastrointestinal symptoms (eg abdominal pain) are not always due to anaphylaxis, but when severe, consider the diagnosis to avoid treatment delay
Assessment
Clinical features of anaphylaxis
| Assessment |
Signs and symptoms |
| Airway |
Difficult or noisy breathing
Tongue (not lip) swelling
Throat swelling or tightness
Hoarse voice or change in character of cry
Drooling (infants)
|
Breathing
(most common in children) |
Difficulty talking
Wheeze
Persistent (usually sudden onset) cough
|
| Circulation |
Pale and floppy (infant)
Persistent dizziness
Sudden drowsiness
Collapse with or without unconsciousness
Hypotension, tachycardia, bradycardia
Cardiac arrest
|
| Gastrointestinal (trigger is relevant when considering GI symptoms) |
Severe/persistent GI symptoms (abdominal pain and/or vomiting) are a sign of anaphylaxis of any cause
Mild GI symptoms (abdominal pain and/or vomiting) are a sign of anaphylaxis when caused by insect stings or parenteral medications
Mild GI symptoms (abdominal pain and/or vomiting) are not a sign of anaphylaxis when caused by food
|
| Skin signs (including facial angioedema, widespread hives) alone do not indicate anaphylaxis (skin signs absent in 10-20%) |
|
Management
Investigations
None in the majority; anaphylaxis is a clinical diagnosis. In special circumstances consider tryptase (see below)
Initial anaphylaxis management
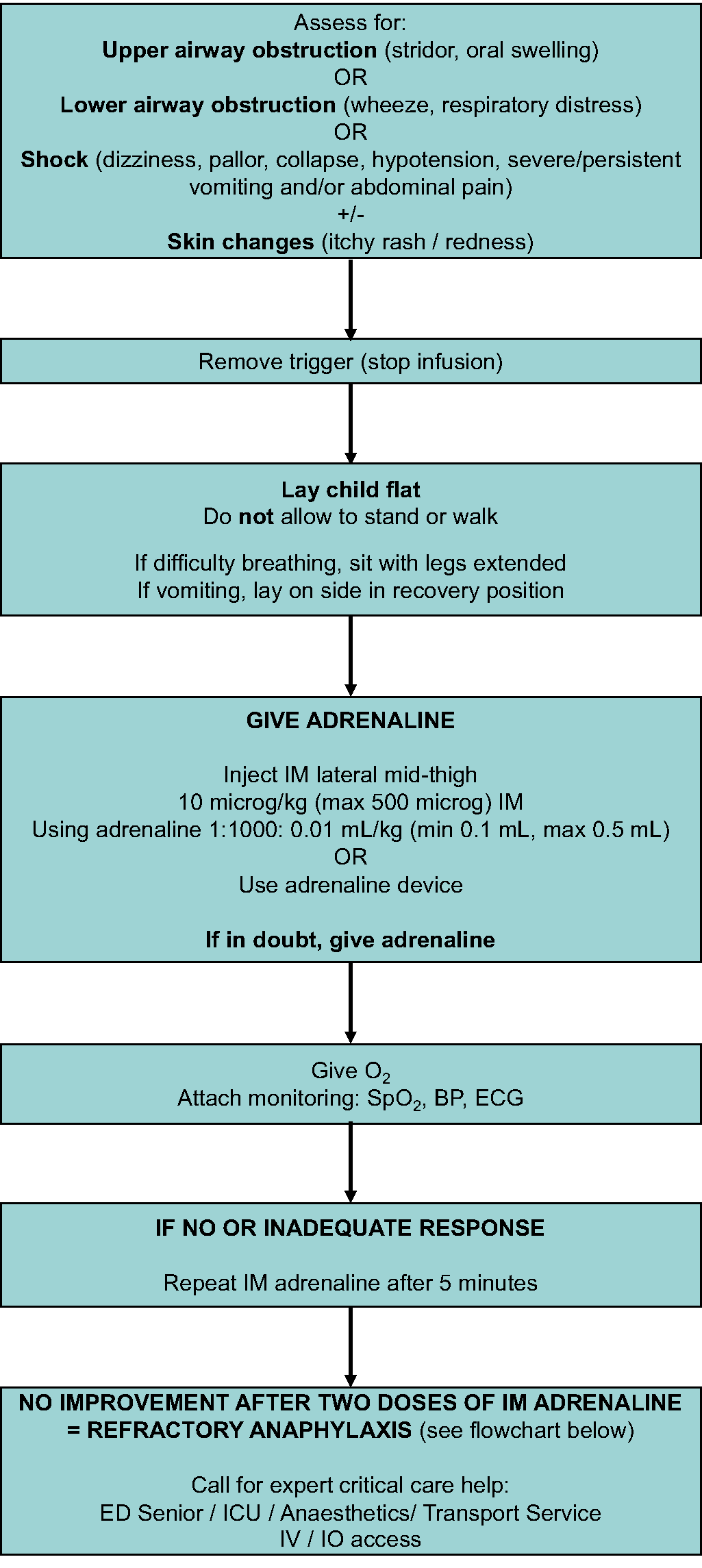
Adrenaline (epinephrine) doses
| Adrenaline dose chart |
| Age (years) |
Weight (kg) |
Volume (mL) of adrenaline 1:1000 |
Adrenaline devices (for use instead of ampoules) |
| <1 |
<7.5 |
0.1 |
Not available |
| 1-2 |
10 |
0.1 |
7.5-20 kg (<5 yrs):
150 microg |
| 2-4 |
15 |
0.15 |
| 4-5 |
20 |
0.2 |
| 5-10 |
30 |
0.3 |
| 10-12 |
40 |
0.4 |
>20 kg (≥5 yrs):
300 microg |
| >12 |
>50 |
0.5 |
>50 kg (>12 yrs):
500 microg or 300 microg |
Adrenaline devices
| Brand name and dose |
Weight (approx age) |
Image |
EpiPen® Jr
(150 microg / 0.15 mg) |
7.5-20 kg (<5 years) |
(Green) |
EpiPen®
(300 microg / 0.3 mg) |
>20 kg (≥5 years) |

(Yellow) |
Anapen®
(500 microg / 0.5 mg) |
>50 kg (>12 years) |

(Purple) |
Refractory anaphylaxis management
Refractory anaphylaxis is anaphylaxis requiring ongoing treatment (due to persisting respiratory or cardiovascular symptoms) despite 2 appropriate doses of IM adrenaline
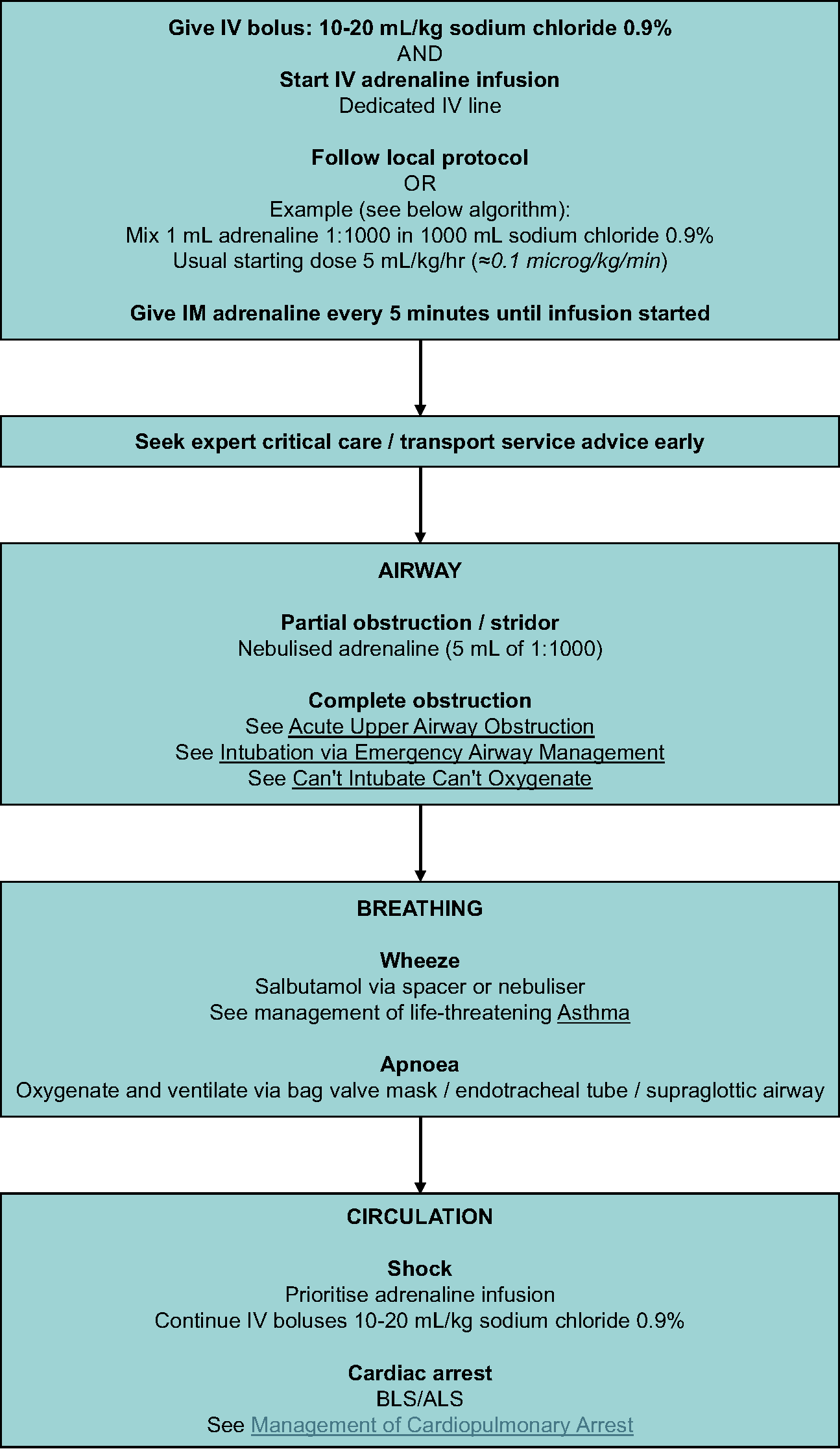
Escalation of management in anaphylaxis refractory to adrenaline infusion:
Peripheral IV adrenaline infusion
Follow local infusion guidelines
In non-tertiary hospital settings, the infusion guideline below can be used in consultation with a senior clinician and paediatric transport services:
- Mix 1 mL of 1:1000 adrenaline in 1000 mL of sodium chloride 0.9% (approx 1 microg/mL)
- Start infusion at 5 mL/kg/hr (approx 0.1 microg/kg/min)
- A dedicated line, infusion pump and anti-reflux valves should be used when possible
- Titrate dose according to response and side effects
- Avoid high infusion rates for more than 2 hours as this may cause fluid overload
- Monitor continuously (all vital signs, 12-lead ECG and conscious state)
Other considerations
- Do not use subcutaneous adrenaline, as absorption is less reliable and can be delayed compared to IM
- Antihistamines, corticosteroids and leukotriene antagonists should not be given in anaphylaxis
- Serum tryptase has no role in acute management of anaphylaxis. It should only be ordered in situations where significant diagnostic doubt exists (eg idiopathic, co-existing anxiety) or after consultation with a paediatric allergy specialist in special circumstances (eg insect stings, diagnostic agents, perioperative reactions)
Observation and admission
All children with anaphylaxis should be observed in a setting equipped to manage deterioration, for at least 4 hours:
- After last dose of adrenaline
- After onset of symptoms if no adrenaline is given
Admission overnight for observation is recommended if:
- >2 adrenaline doses, adrenaline infusion, IV fluid resuscitation, circulatory involvement
- History of biphasic reaction, more severe initial reaction
- Poorly controlled asthma
- Lives in an isolated location with delay to emergency services
- Presents for medical care late in the evening
- Anaphylaxis to monoclonal antibody therapy
Consider consultation with local paediatric and/or allergy/immunology team when
- High risk of fatal anaphylaxis (see additional notes)
- >1 dose of adrenaline
- First diagnosis of anaphylaxis
- Anaphylaxis to monoclonal antibody therapy
Consider transfer when
- >2 doses of adrenaline (refractory anaphylaxis)
- Adrenaline infusion
- A child requiring care beyond the comfort level of the hospital
Consider discharge when
Clinically stable and not requiring adrenaline for at least 4 hours
Prior to discharge all children and their families should receive education, resources and follow up options outlined in the following checklist:
- Update the medical record identifying suspected allergen to avoid where possible
- Individualised ASCIA Action Plan for Anaphylaxis (red) for Medication Allergy (dark green)
- 2 EpiPen®/ EpiPen® Jr/ Anapen® supplied or prescribed, if unable to access script due to pharmacy closure (eg overnight) then consider keeping until morning
- Training in correct use with trainer device of prescribed brand and appropriate positioning (eg not standing or walking during anaphylaxis)
- Children with medication (drug) anaphylaxis are generally not prescribed an adrenaline device
- Consider MedicAlert bracelet
- Provide general information regarding allergies and anaphylaxis (see Allergy & Anaphylaxis Australia and ASCIA Anaphylaxis Resources)
- Referral to paediatrician or paediatric allergy/immunology specialist for review as soon as possible
- Optimise asthma management including diagnosis, asthma action plan and preventers (see Asthma)
- Consider reporting as per local requirements
EpiPen® / EpiPen® Jr / Anapen® are available on PBS for all children with a history of anaphylaxis. See ASCIA Guidelines for Adrenaline Injector Prescription for more information. They require authority prescription or can be purchased without prescription at full cost. See PBS authority indications
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Parent information
Additional notes
According to the World Allergy Organisation Anaphylaxis Committee, anaphylaxis is highly likely when any one of the following two criteria are fulfilled:
- Acute onset of an illness (minutes to several hours) with simultaneous involvement of the skin, mucosal tissue, or both (eg generalized hives, pruritus or flushing, swollen lips-tongue-uvula), and at least one of the following:
- Respiratory compromise (eg dyspnoea, wheeze-bronchospasm, stridor, reduced peak expiratory flow, hypoxaemia)
- Reduced blood pressure or associated symptoms of end-organ dysfunction (eg hypotonia (collapse), syncope, incontinence)
- Severe gastrointestinal symptoms (eg severe crampy abdominal pain, repetitive vomiting), especially after exposure to non-food allergens
- Acute onset of hypotension or bronchospasm or laryngeal involvement after exposure to a known or highly probable allergen for that patient (minutes to several hours), even in the absence of typical skin involvement
Timing
- Timing of reactions is dependent on the trigger, most develop quickly over minutes
- Allergens given by parenteral route (eg IV medication, IM injection, insect sting) often cause symptoms in 5-15 minutes
- Ingested food allergens cause symptoms typically by 30 minutes
- Oral medication (drug) allergy are slower usually occurring in 1-6 hours
Fatal anaphylaxis
- Prevalence: rare in Australia, approximately 1 per million/population
- Mainly triggered by food in children
- Cardiorespiratory arrest more than 4 hours after initial allergen exposure is rare
- Risk factors
- Delay to administration of adrenaline or emergency response services
- Upright posture
- Poorly controlled asthma (see Asthma)
- Allergy to peanut, tree nuts and seafood
- Adolescence
- Pre-existing cardiac and respiratory conditions
- Severity of previous reactions does not predict future risk
- Proper diagnosis and safe discharge management are essential to minimise risk on discharge
Last updated October 2025