See also
Emergency airway management
Hospital management of cardiopulmonary arrest
Foreign body inhalation
Key points
- Can’t Intubate Can’t Oxygenate (CICO) situations are life threatening emergencies due to airway obstruction that require immediate Front of Neck Access (FONA) to the trachea
- True CICO emergencies in children are rare. Ensure all reversible causes of airway obstruction such as laryngospasm and upper airway obstruction have been corrected, and the indications for a CICO emergency have been met prior to performing FONA
- Continue attempting oxygenation via facemask with an oropharyngeal airway while the CICO equipment is mobilised and while the FONA is performed
- Equipment required to perform FONA must be pre-prepared in all intubating locations
Background
- Difficult airways in children are rare, and usually anticipated as they are due to obvious congenital airway abnormalities or acute airway pathology. When difficulty is anticipated, expert assistance should be sought prior to initiating airway management if time permits
- Difficult ventilation in children without airway abnormalities is most often due to laryngospasm and upper airway obstruction. These conditions are reversible with appropriate management (see Appendix 1 below) , and should not require FONA
- Emergency FONA is a potentially life saving procedure. However, even with training, it is difficult to perform in small children, infants and neonates. Even when ventilation is severely impaired, sufficient oxygenation may be achievable. In this situation, there should be time to mobilise an ENT surgeon to perform a formal tracheostomy
- If all measures to oxygenate a child are unsuccessful, and an ENT surgeon is not present, a CICO emergency must be declared, and airway doctors must perform emergency FONA
Indications
Criteria for declaring a CICO emergency:
- Child is anaesthetised, and cannot be woken rapidly, or is unconscious with GCS <8
- Unable to intubate
- Unable to oxygenate/ventilate with either an oropharyngeal airway, a laryngeal mask airway, or a two person ventilation technique
- Oxygen saturation is <80% (<50% with cyanotic heart disease) with bradycardia
- Reversible causes have been excluded
- Cricoid pressure, if applied, has been removed
Equipment
A prepared CICO pack containing the equipment necessary to perform FONA should be located in all intubating locations. The contents of the Royal Children’s Hospital Melbourne CICO pack are listed below, and are explained in detail in this video
CICO Pack Contents
- Equipment for cannula cricothyroidotomy
- 16G cannula
- Rapid O2 oxygen insufflator
- 5 mL syringe
- 10 mL saline ampoule
- Content list of equipment necessary to perform cannula cricothyroidotomy
- Equipment for scalpel cricothyroidotomy
- Size 10 scalpel on a handle (disposable)
- “Bougies”. Sizes:
- 5 CH 50cm Portex™ Tracheal Tube Guide
- 8 Fr 35cm Cook Frova™ Intubating Introducer (with stiffening rod removed and 15mm Rapi-Fit™ connector attached)
- 11 Fr 83cm Cook™ Airway Exchange Catheter (with 15mm Rapi-Fit™ connector attached)
- Halyard MicroCuff™ Endotracheal tubes. Sizes: 3.0, 4.0, 5.0
- Lubricant sachet
- Content List of equipment necessary to perform the scalpel bougie technique
Additional CICO equipment
- Cook Melker™ Emergency Cricothyrotomy Sets. Sizes: 3.5, 4.0 uncuffed and 5.0 cuffed. For more information see Additional notes section below
Analgesia, Anaesthesia, Sedation
- Ensure all medications are drawn up and labelled pre-procedure (analgesia, sedatives, hypnotics, muscle relaxants)
- Unless the child is in cardiac arrest, administer hypnotic medications (eg ketamine) before muscle relaxants (eg rocuronium)
- Consider delay between administration of anaesthetic agent and muscle relaxant - at discretion of team leader
- Prioritise avoidance of hypoxia at all times. Continue gentle positive pressure ventilation with positive end-expiratory pressure (PEEP) during the apnoeic period. During laryngoscopy, increase flow to 2 L/kg/minute (max 15 L/min)
Medication dosing |
Induction agent |
- All induction agents can precipitate acute hypotension. See Emergency Resources
- Ketamine (0.5–2 mg/kg) is one medication commonly used for most emergency intubation scenarios
|
Muscle relaxant |
- Higher doses may be required in unwell children to achieve normal onset of action
- Rocuronium (1.2–1.6 mg/kg) is one medication commonly used for emergency intubation
|
Procedure
In the event of a CICO event, progress to either:
- Surgical cricothyroidotomy (>12 years)
- Needle cricothyroidotomy (any age; may be used to gain time before surgical cricothyroidotomy)
Procedure
There is debate in the literature as to what is the safest and most effective technique to perform FONA. Therefore, it is important that a hospital has determined its procedure of choice, and that relevant staff have been trained accordingly. The Royal Children’s Hospital Melbourne algorithm is included below.
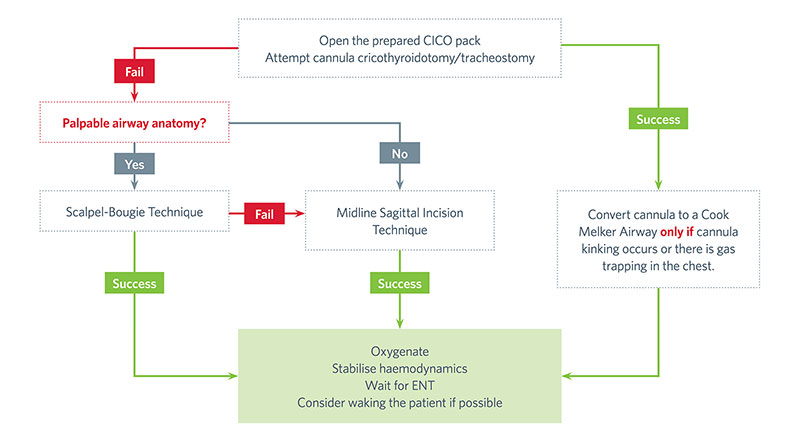
See below for further details regarding the procedures and the algorithm
Cannula cricothyroidotomy
- One staff member continues oxygenation attempts with facemask ventilation, and an oropharyngeal airway. Ensure other staff are checking the femoral pulse and commencing chest compressions if necessary
- Extend head and neck (consider a shoulder roll) to expose front of neck
- Stand on child's left and palpate thyroid and cricoid cartilages with the left hand to locate cricothyroid membrane
- Immobilise trachea between left index finger and thumb
- Attached 5 mL syringe with 2 mL of saline to back of trochar
- Insert cannula at a 45o angle with the right hand staying midline
- Aspirate continuously as soon as cannula is advanced posteriorly and inferiorly
- As soon as air is aspirated, advance cannula forward off the trochar (do not pull trochar back) into trachea with the left hand and hold it there carefully
- Remove trochar and disengage syringe from trochar with the right hand
- Place syringe onto cannula and aspirate air to confirm correct position
- Attach rapid oxygen insufflator to cannula with the right hand ensuring that the left hand is holding cannula securely in trachea at all times
- Have an assistant attach oxygen tubing of insufflator to an oxygen flowmeter, and turn on oxygen flowmeter to 1 L/min/year of age (although minimum flow should be 4 L/min)
- Occlude insufflator hole with thumb of the right hand to insufflate oxygen into trachea. Tactile feedback to the thumb occluding the hole of insufflator will inform whether cannula is kinked
- Insufflate oxygen until chest has expanded and then remove thumb occluding hole in insufflator. Watch neck to see if subcutaneous emphysema develops, indicating incorrect placement of cannula. (NB rise in oxygen saturations will be delayed)
- Do not insufflate oxygen again until chest has returned to its original size or oxygen saturations begin to fall. Attempting regular ventilation will cause dynamic hyperinflation as expiration is limited
- Continue this pattern of oxygenation until ENT available to perform formal tracheostomy
- If there is significant delay until ENT can perform tracheostomy, or if cannula jet oxygenation becomes compromised by blood, secretions or kinking, perform a Melker conversion. Unlike adult practice, converting to Melker catheter is not routinely recommended, as it adds further risk of loss of ability to oxygenate due to increased difficulty of procedure in children (see Additional notes section below)
Scalpel-bougie cricothyroidotomy
Perform this technique if cannula cricothyroidotomy is unsuccessful. The aim of this technique is to place an endotracheal tube into the trachea via the front of the neck. Use appropriate sized equipment for child. See video
- 3.0 ETT with the 5Fr bougie for neonates and infants
- 4.0 ETT with the 8Fr Frova introducer for children
- 5.0 ETT with the 11Fr Airway Exchange Catheter for teenagers
2. Repeat Steps 1–4 above
3. Using the size 10 scalpel blade, make a horizontal incision through the skin and cricothyroid membrane into the trachea. The incision needs to be wide enough to allow the passage of the appropriate ETT
4. Rotate the blade 90o into the sagittal plane and pull the flat of the scalpel blade toward you keeping it vertical. This creates the opening through which the bougie can be placed into the trachea
5. After the bougie is in the trachea, pass the ETT over the bougie into the trachea rotating it to corkscrew it through the skin incision if it is tight
6. Advance the ETT only until the cuff is in the trachea to avoid endobronchial intubation
7. Attach the circuit to the ETT and begin ventilation
a. Note: as opposed to jet oxygenation via a cannula, with this technique standard ventilation is appropriate
Midline sagittal incision cricothyroidotomy
- Midline incision in the sagittal plane - should be performed if:
- failed cannula cricothyroidotomy in situation of impalpable airway anatomy due to obesity or pathology (this precludes scalpel bougie technique described above) OR
- this is your institution’s technique of choice as first line
- Using size 10 scalpel blade, make incision from sternal notch up towards chin. Unlike in adults, in children it is not possible to specify length of incision. However, length of incision should aim to expose the area up to the thyroid cartilage
- Use fingers, to spread the subcutaneous tissues and strap muscles to expose the trachea and cricothyroid membrane
- With the airway anatomy now visible, perform a cannula or scalpel bougie cricothyroidotomy
Post procedure care instructions
- FONA is a temporary emergency airway. These airways should be continuously held by hand until a secure definitive airway has been established. A definitive airway includes conversion to a formal tracheostomy or a flexible fibreoptic or video scope intubation
- Where possible, do not transfer child between (or within) hospitals until definitive airway has been established.
Consult with local retrieval service
Consider consultation with local paediatric team when
Airway staff are unfamiliar or require assistance with paediatric emergency airway management and ventilation
Consider transfer when
No facility to manage a child with a surgical airway is available at the local hospital
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Additional notes
Last updated March 2021
Appendix 1: Management of laryngospasm
Laryngospasm is complete or partial sustained adduction of the vocal cords. Signs include: paradoxical chest movement or a rigid abdominal muscles, high pitched stridor, and destauration. Partial laryngospasm will allow some movement of air/oxygen and the stridor is usually loud. Complete laryngospasm is silent. With emergency intubations, the routine use of muscle paralysis will mean that laryngospasm should not occur. It is therefore more likely in elective general anaesthesia, with the administration of procedural
sedation, or in partially unconscious patients who have maintained some airway reflexes
Management should progress quickly through these steps:
- Stop any procedures or stimulating procedures
- Call for senior help
- Administer 100% oxygen via a facemask, perform a chin lift, and administer continuous positive airway pressure (CPAP)
- Medications
- Propofol 0.5-1 mg/kg may be used to treat persisting partial laryngospsm
- Suxamethonium 1 mg/kg (full paralysis is not required to break laryngospasm)
- Intubation.
Note: if laryngospasm relieved with CPAP alone or single dose of propofol, intubation may not be necessary
Suctioning the oropharynx, jaw thrust, and placement of an oropharyngeal airway should be considered with caution. Suctioning may be required in the presence of excessive secretions or regurgitation. Just thrust and placement of an oropharyngeal airway may be required if there is also upper airway obstruction from the tongue and soft palate. However, these procedures are also stimulating and could exacerbate the situation by turning partial laryngospasm into complete. If the patient is not responding to the initial measures then treat upper airway obstruction as well
Appendix 2: Potential complications
- Unsuccessful FONA
- Complications from cannula cricothyroidotomy
- Posterior wall perforation
- Barotrauma and volutrauma from jet oxygenation
- Subcutaneous emphysema in the neck
- Complications from scalpel techniques
- Damage to surrounding structures
- Bleeding