See also
Diabetes insipidus
Diabetic ketoacidosis
Diabetes mellitus: Management of unwell children with established diabetes at home
Diabetes mellitus: Management of unwell children with established diabetes in hospital
Diabetes mellitus and surgery
Hyperosmolar hyperglycaemic state
Key points
- This CPG is for children with a new diagnosis of diabetes mellitus who are not in diabetic ketoacidosis (DKA)
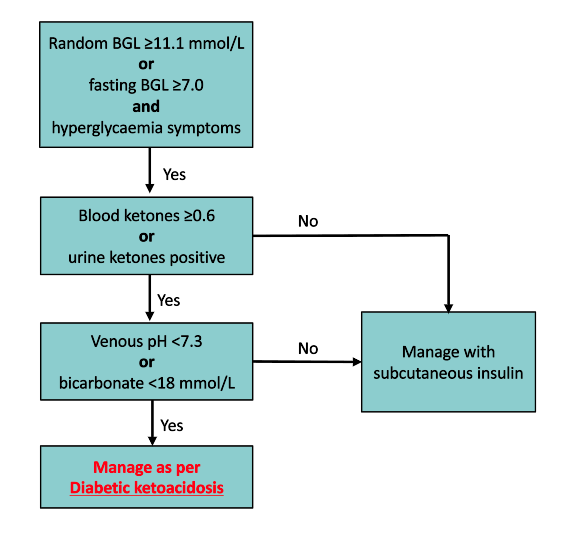
- A blood glucose level (BGL) should be checked in most acutely unwell children, as diabetes can present non-specifically
- Random BGL ≥11.1 mmol/L or fasting BGL ≥7.0 mmol/L, together with symptoms of hyperglycaemia, are diagnostic of diabetes in a child
- A child with a new diagnosis of diabetes mellitus who is not in DKA can be managed with subcutaneous insulin injections
Background
- Classic symptoms of hyperglycaemia that should prompt consideration of diabetes include:
- polydipsia (excessive thirst)
- polyuria (excessive urination)
- new onset nocturnal enuresis (ie in a child who was previously dry overnight)
- unexplained weight loss
- unexplained fatigue
- Other non-specific presentations (which may indicate ketosis/ketoacidosis) include vomiting, respiratory distress, dehydration, abdominal pain, altered consciousness
- A diagnosis of diabetes should not be based on a single BGL reading in the absence of symptoms of hyperglycaemia. If the diagnosis is in doubt additional testing may be required (eg HbA1c, OGTT, continued monitoring of BGLs) in discussion with a
paediatric specialist
- Most cases of diabetes in children are due to Type 1 diabetes mellitus
- The possibility of other types of diabetes should be considered in the following circumstances, when diabetes autoantibodies are negative:
- Type 2 diabetes: obesity, acanthosis nigricans, strong family history
- Monogenic diabetes:
<6 months of age at presentation (neonatal diabetes mellitus), autosomal dominant family history of diabetes (MODY)
- Diabetes can also be secondary to certain medications (eg glucocorticoids, tacrolimus) and other disease processes that can affect the pancreas eg cystic fibrosis, hereditary haemochromatosis
Assessment
History
- Presence and duration of symptoms:
- excessive thirst
- excessive urination
- weight loss
- vomiting
- abdominal pain
- fatigue
- Concurrent illness
- Medications
- Past medical history
- Family history of diabetes and other autoimmune conditions
Examination
- Conscious state (AVPU/GCS)
- Respiratory signs: respiratory rate, increased work of breathing
- Assess hydration status
- Weight
Management
Investigations
- Formal serum blood glucose level
- Point of care blood ketones if random BGL ≥11.1 mmol/L
- urine ketones may be used for initial assessment if blood ketones are unavailable
- Venous blood gas
If pH <7.3 or bicarbonate <18 mmol/L, manage as per Diabetic ketoacidosis
Other investigations
- UEC
- Diabetes autoantibodies: anti-GAD, insulin autoantibodies (IAA), insulinoma-associated-2 autoantibodies (anti-IA2), zinc transporter 8 (ZnT8)
- Coeliac serology (transglutaminase IgA and total IgA)
- TSH, FT4
- Additional investigations may be required as part of diagnostic workup, or for associated conditions
- C-peptide
- Insulin level
- Thyroid autoantibodies: thyroid peroxidase, thyroglobulin
- Coeliac screen
- Lipid profile
- Liver function tests
Treatment
Intravenous fluids if required for dehydration. See Intravenous fluids
Choice of insulin therapy
Note: some centres use different management guidelines, see local protocols
Subcutaneous insulin (for children not in DKA)
If ketones are elevated (≥0.6) insulin should be started as soon as possible to prevent DKA
The two most common regimens for insulin dosing are fixed multiple daily injection (MDI) and flexible insulin dosing
- MDI insulin dosing (also called basal-bolus insulin):
- Calculate total daily insulin (TDD), see guide below. Give 40% as long-acting basal insulin (daily) and 60% as rapid-acting insulin divided into 3 x boluses with meals ie 20% TDD rapid-acting insulin with each meal
- Flexible insulin dosing:
- The dose of rapid-acting insulin is calculated before each meal (or snack) based on pre-meal BGL and the amount of carbohydrates being consumed
- In addition, rapid acting insulin is given to correct hyperglycaemia before and between meals
- The insulin carbohydrate ratio (ICR) is the number of grams of carbohydrate that require 1 unit of insulin to be administered, and is used to determine the rapid-acting insulin dose for a quantity of carbohydrates
- The insulin correction factor (CF) is the expected BGL decrease (in mmol/L) with 1 unit of insulin administered, and is used to determine the rapid-acting insulin dose to correct hyperglycaemia
Note: the CF is also called the
insulin sensitivity factor (ISF) - Long-acting insulin is given daily, typically in the evening
Note: twice daily (BD dosing) injections are rarely used as a standard regimen and are limited to extremely rare circumstances where more precise dosing cannot be achieved in extraneous circumstances
A guide to initial insulin doses is given below. Insulin regimens will need to be individualised to the child's needs as indicated by BGL levels
- Where possible, discuss ongoing insulin dosing with a paediatric endocrinologist or paediatrician with experience in paediatric diabetes and always consult local guidelines where available
- Pre-meal BGL target is 4-8 mmol/L. If BGL >8 mmol/L use CF to determine dose of rapid-acting insulin to return BGL to 6 mmol/L (unless insulin has already been given in preceding 2 hours)
- Pre-meal rapid-acting insulin should be given 15 minutes prior to the meal (except Fiasp®, which can be given at the time of the meal due to faster onset)
Suggested dosing for initiation of subcutaneous insulin therapy
| Multiple daily injections (MDI) |
Insulin type
and frequency |
Long-acting (basal) insulin once daily (typically at night)
and
Pre-meal injections of rapid-acting insulin |
| Finger prick blood glucose monitoring* |
Pre-meals (breakfast, lunch, dinner)
2 am (during initial stabilisation/admission)
Whenever hypoglycaemia is suspected
Note:
more frequent BGL monitoring may be required on initial administration eg 2 hours following first insulin dose and 4-hourly overnight, especially if child is ketotic |
Initial total daily dose
(TDD) |
For children
<1 year consult paediatric endocrinologist
1-5 years: 0.5 units/kg/day 5-10 years: 0.7 units/kg/day >10 years: 0.7-1.0 units/kg/day |
| Dosing |
- Calculate total daily dose as above
- Give 40% of TDD as long-acting insulin in the evening
- Divide remaining 60% into 3 doses of rapid-acting insulin and give pre-meal at breakfast, lunch and dinner ie ~0.1 - 0.2
units/kg before each main meal
|
| Comments |
If commencing first dose rapid-acting insulin >2 hours before mealtime, consider giving stat 0.2 units/kg of insulin; then begin regular rapid-acting insulin with meals as above Children presenting during the day may need slightly
higher pre-meal doses (eg 0.25 units/kg) until basal insulin is given that evening Round insulin dose down to nearest 0.5 unit |
| Flexible insulin dosing |
Insulin type
and frequency |
Long-acting (basal) insulin once daily (typically evening)
Rapid-acting insulin is given: - pre-meals (breakfast, lunch dinner)
- with snacks containing >15 grams of carbohydrate
- if BGL >8 mmol/L and taken >2 hours after
last insulin during the day dose, or BGL >15 mmol/L overnight
|
| Finger prick blood glucose monitoring* |
Pre-breakfast Pre-lunch
Pre-afternoon tea (>2 hours following lunchtime insulin)
Pre-dinner
Pre-bed (>2 hours following dinner)
2 am (during initial stabilisation/admission)
Whenever
hypoglycaemia is suspected
Note: some centres also check BGL at morning tea and 4-hourly overnight on initiating insulin |
| Long-acting insulin dosing |
Daily long-acting insulin given in the evening (see table below for dosing guide) |
| Rapid-acting insulin dosing |
Insulin dose =
1) Insulin needed to correct BGL (child's BGL minus target BGL 6 mmol/L, then divide by correction factor)
plus
2) Insulin needed to cover carbohydrate being eaten (grams of carbohydrate
divided by insulin:carbohydrate ratio)
eg pre-lunch BGL 16, eating 20 g carb, child has CF 2 and ICR 5
1) Insulin required to correct BGL = 16 (child's BGL) - 6 (target BGL) = 10 mmol/L 10
mmol/L ÷ 2 (CF) = 5 units
2) Insulin to cover carbohydrates being eaten (ICR) =
20 grams ÷ 5 (ICR) = 4 units
3) Give insulin 5 + 4 = 9 units
If giving insulin to correct BGL but child is not eating or eating
<15 grams carbohydrate, calculate insulin dose using CF only
ie step 1 only
If giving insulin with food and BGL 4-8 mmol/L, use step 2 only |
| Initial ICR and CF |
Please see Appendix 1 and 2 for suggest initial ICR and CF ratios.
ICR and CF ratios will change based on BGLs following initiation of insulin. This document provides a guide for initiation only |
| Comments |
Round insulin dose down to nearest 0.5 unit |
*Note: many children will be started on a continuous glucose monitor (CGM) early in their admission. Finger prick BGL may vary in this instance. Please see CGM
Ketone monitoring
- If ketones are present at diagnosis, continue to measure with each BGL every 2 hours until ketones
<0.6
- As part of ongoing management, ketones should be checked whenever
BGL ≥15 or child is unwell
Consider consultation with local paediatric team
- For all new presentations of diabetes in children. In most centres these children need to be admitted for initiation of insulin therapy and diabetes education
- In some tertiary centres, hospital in the home (HITH)/ambulatory care programs may be considered in appropriate cases; discuss with paediatric endocrinology team first
Consider transfer when
Child requiring care beyond the level of comfort of the treating hospital
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
- Child tolerating oral intake
- Child linked in with local diabetes care team and contact information provided
- Initial diabetes education completed, usually involves input from diabetes nurse educator, dietician, social work
- Family competent in monitoring BGLs and administering insulin and treating hypoglycaemia
Parent information
Kids Health Information: Diabetes
Diabetes Australia
RCH-specific info
Appendix 1: Initial recommended insulin:carbohydrate ratio (ICR), correction factor (CF) and long-acting insulin
| Initial ICR and CF and long-acting insulin dose |
| Weight |
ICR |
CF |
Long-acting insulin |
| 10 kg |
30 |
10 mmol/L |
2 units |
| 15 kg |
20 |
6.5 mmol/L |
3 units |
| 20 kg |
20 |
5 mmol/L |
4-6 units |
| 25 kg |
20 |
4 mmol/L |
5-7 units |
| 30 kg |
17 |
3.5 mmol/L |
6-10 units |
| 35 kg |
14 |
3 mmol/L |
8-14 units |
| 40 kg |
12.5 |
2.5 mmol/L |
10-16 units |
| 45 kg |
11 |
2 mmol/L |
12-18 units |
| 50 kg |
10 |
2 mmol/L |
14-20 units |
| 55 kg |
9 |
2 mmol/L |
16-22 units |
| 60 kg |
8 |
1.5 mmol/L |
18-24 units |
| >60 kg |
8 |
1.5 mmol/L |
20-25 units |
Appendix 2: Flexible dosing insulin with variable ICR throughout the day
Takes into account insulin sensitivity variation throughout the day
| Child's weight |
ICR at breakfast
(grams of carbohydrate per 1 unit short-acting insulin) |
ICR at lunch
(grams of carbohydrate per 1 unit short-acting insulin) |
ICR at afternoon tea
(grams of carbohydrate per 1 unit short-acting insulin) |
ICR at dinner
(grams of carbohydrate per 1 unit short-acting insulin) |
Correction factor for BGL >6
(mmol/L BGL drops with 1 unit insulin) |
Long acting insulin
eg Detemir or glargine
(units) |
| 10 kg |
15 |
20 |
30 |
30 |
10 |
2.5 |
| 11-13 kg |
10 |
12 |
30 |
30 |
8 |
3 |
| 14-16 kg |
10 |
12 |
20 |
20 |
6.5 |
3.5 |
| 17-20 kg |
8 |
10 |
20 |
20 |
5.5 |
4 |
| 21-25 kg |
7 |
10 |
20 |
20 |
4 |
5.5 |
| 26-30 kg |
6 |
8 |
15 |
15 |
3.5 |
6.5 |
| 31-35 kg |
6 |
7 |
15 |
15 |
3 |
8 |
| 36-40 kg |
6 |
7 |
15 |
15 |
2.5 |
9 |
| 41-45 kg |
5 |
6 |
12 |
12 |
2 |
10 |
| 46-50 kg |
5 |
6 |
12 |
12 |
2 |
11 |
| 51-55 kg |
4 |
5 |
10 |
10 |
2 |
12 |
| 56-60 kg |
4 |
5 |
10 |
10 |
1.5 |
14 |
| >60 kg |
3 |
4 |
8 |
8 |
1.5 |
18 |
Last updated July 2025
Reference List
- Anderson, K., Scott, F., Kenneady, A., O'Brien, J., Van Roon, S., Sharp, A., Pearce, H., Virgona, M. Paediatric management of a newly diagnosed child with T1DM without DKA -- Guide for hospital staff. Retrieved from PROMPT, Barwon Health (viewed
2022)
- Beckles, Z. L., Edge, J. A., Mugglestone, M. A., Murphy, M. S., & Wales, J. K. Diagnosis and management of diabetes in children and young people: summary of updated NICE guidance. Bmj. 2016. 352.
- Cengiz, E., Danne, T., Ahmad, T., Ayyavoo, A., Beran, D., Ehtisham, S., Fairchild, J., Jarosz-Chobot, P., Ng, S. M., Paterson, M., Codner, E. ISPAD Clinical Practice Consensus Guidelines 2022: Insulin treatment in children and adolescents
with diabetes. Pediatr Diabetes. 2022. 23(8), 1277-1296.
- Craig, M. E., Twigg, S. M., Donaghue, K. A., Cheung, N., Cameron, F., Conn, J., & Silink, M. National evidence-based clinical care guidelines for type 1 diabetes in children, adolescents and adults. 2011. Australian Government Department of
Health and Ageing. Canberra.
- Mayer-Davis, E. J., Kahkoska, A. R., Jefferies, C., Dabelea, D., Balde, N., Gong, C. X., & Craig, M. E. ISPAD Clinical Practice Consensus Guidelines 2018: Definition, epidemiology, and classification of diabetes in children and adolescents.
Pediatric diabetes. 2018. 19(Suppl 27), 7-19.