See also
Acute asthma
Engaging with and assessing the adolescent patient
Key points
- Any adolescent with asthma should be on a treatment regimen that includes an ICS. Prescribing SABA treatment (ie salbutamol) alone is no longer recommended
- For most adolescents with asthma, treatment can be started with as-needed (reliever) combination of an ICS and a LABA
- Adolescents well controlled on traditional treatment with SABA and inhaled ICS, should not be changed without consulting the adolescent’s care team or a senior clinician
- Treatment can be stepped up and down according to response. Never cease an adolescent’s ICS completely
- Always check inhaler technique, compliance and contributing factors before dose adjustment
Background
- Asthma medications and delivery devices include:
- Inhaled corticosteroid (ICS)
- Short-acting β-agonist (SABA)
- Long-acting β-agonist (LABA)
- Metered Dose Inhaler (MDI)
- Dry Power Inhaler (DPI), including the Turbuhaler®
- High use of SABA alone (>3 MDI canisters per year) and low use of preventer/anti-inflammatory is associated with more severe asthma exacerbation and death
- Combination treatment with ICS/LABA ensures use of anti-inflammatory with every reliever dose
- This is termed an anti-inflammatory reliever-based regimen
- At present budesonide/formoterol is the only combination that can be prescribed as a reliever. Other combination inhalers (eg Seretide) should not be used
- Traditional management with daily inhaled corticosteroid (ICS) as a preventer and SABA as needed is also effective. It may be preferred for those already on a regimen that is working or if there are difficulties with DPI/Turbuhaler® technique
- The risk of fatal anaphylaxis is higher in adolescents with poorly controlled asthma
- MDI
have a large carbon footprint. The best way to decrease the impact is to achieve
good asthma control to reduce need for SABA and/or switch to DPI when possible. Other measures include:
- prescribing 1 puff of a stronger dose preventer instead of 2 puffs of a weaker
dose, particularly if dose is stable and unlikely to be reduced in the short
term (also reduces cost)
- dose tracking
- See Additional resources below
for more information on green prescribing
Assessment
History
Assessment of asthma control:
- Daytime symptoms
- Need for reliever (doses per week)
- Limitation of activities
- Symptoms at night or on waking
Examination
- Review inhaler technique
- Look for signs of comorbidity, including allergic rhinitis and eczema
Management
Investigations
- In most adolescents, the diagnosis can be made clinically based on symptoms and response to treatment
- Investigations should only be performed if other diagnoses are being considered, or if treatment is to be stepped up beyond Step 3 (see management below). Consider consultation with a respiratory physician
- Spirometry should be performed in a respiratory function laboratory accredited to test adolescents. It should include bronchodilator response and may include exercise or other challenge tests if required
1. Initiating treatment
The decision to commence an anti-inflammatory reliever-based regimen can be made either following an acute presentation (eg on discharge from emergency), or on routine review in an outpatient setting
Most adolescents will start at step one, based on the stepladder approaches shown below
- If an adolescent is already established on a traditional reliever plus preventer regimen, it is more appropriate to discuss with their long-term care provider
Anti-inflammatory reliever-based regimen (budesonide/formoterol 200 mcg/6 mcg)
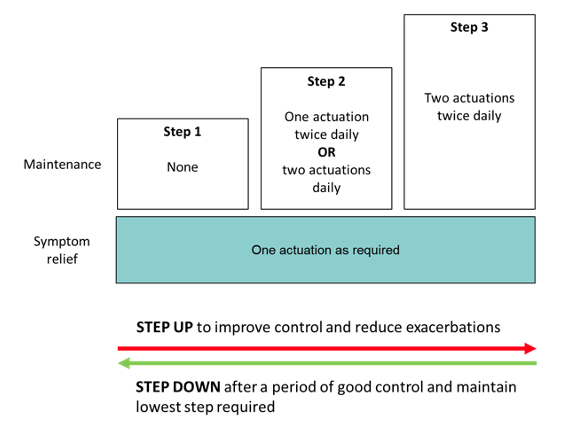
Adapted from Beasely R, et al2 and GINA Pocket Handbook 20214
Traditional SABA as reliever plus ICS as preventer-based regimen
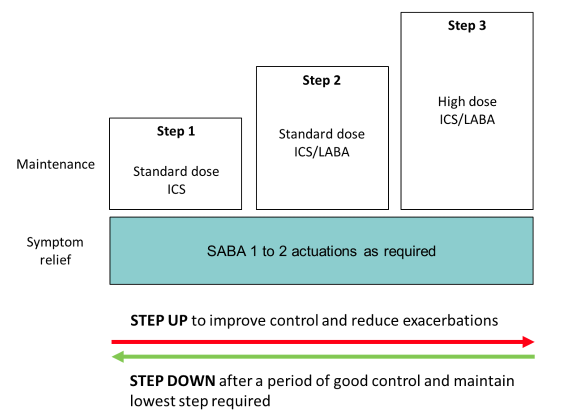
Adapted from Beasely R, et al2 and GINA Pocket Handbook 20214
2. Stepping up or down according to response
The degree of symptom control, irrespective of the current regimen, informs whether changes need to be made to the preventer treatment
|
Good control
(All of) |
Partial control
(One or two of) |
Poor control
(Three or more of) |
Daytime symptoms |
≤2 days per week |
>2 days per week |
>2 days per week |
Need for reliever* |
≤2 days per week |
>2 days per week |
>2 days per week |
Limitation to activity |
none |
present |
present |
Night time symptoms (or on waking) |
none |
present |
present |
* Reliever frequency does not include doses taken prophylactically before exercise
- Poor control suggests preventer medication should be stepped up according to the figures above
- Always check correct technique and adherence prior to stepping up. Consider alternate diagnoses
- Good control for a period of approximately 3 months suggest preventer treatment could be stepped down
- Never cease an adolescent's ICS completely
- If stepping down to reliver use only, use combination ICS and LABA as reliever
- If a severe exacerbation occurs, review and consider stepping up
3. When to consider additional treatment
- Adolescents with severe, uncontrolled asthma (step 3 and ongoing poor response to treatment) should be referred to a respiratory physician or specialist asthma service
- Additional treatment that may be considered for this group are:
- Oral prednisolone 1 mg/kg (max 50 mg) daily for 2 weeks
- Tiotropium 2.5 mcg 2 puffs daily
- Montelukast 5 mg daily
4. Other management considerations
DPI (Turbuhaler®) vs MDI Anti-inflammatory Reliever-based treatment
- Turbuhaler® (200/6) has the advantages of being more portable and carrying a lower carbon footprint but requires adequate technique.
- An alternative is to continue using budesonide/formoterol MDI (Rapihaler®) with spacer in 100 mcg/3 mcg dosing. This should be 2 puffs twice daily.
Inhaled corticosteroids (ICS)
The most common ICS are:
- Fluticasone, start at 125 mcg twice daily and increase until total daily dose 500 mcg
- Ciclesonide, start at 80 mcg once daily and increase to 320 mcg as required
Anti-inflammatory Reliever-based Asthma Action Plan
- A written asthma action plan is a core part of asthma management. Specific action plans for anti-inflammatory reliever-based treatment are available
- The written asthma action plan should clearly communicate when medical attention should be sought. This is generally when:
- DPI: a total of 12 actuations of budesonide/formoterol in a day
- MDI: a total of 24 inhalations of budesonide/formoterol in a day
Anti-inflammatory reliever-based treatment: management in hospital
- For exacerbations requiring hospital presentation, treat with SABA as per standard practice (see acute asthma)
- If reliever treatment is needed at home and only SABA is available, this should be used whilst awaiting an ambulance
- On discharge resume budesonide/formoterol for symptom relief
5. Approach to asthma not responding to treatment
- Review if asthma is correct diagnosis
- Review adherence
- Review inhaler technique
- Consider contributing factors
- Allergic rhinitis
- Obesity
- Obstructive sleep apnoea
- Gastro-oesophageal reflux
- Dysfunctional breathing (including vocal cord dysfunction)
- Depression/anxiety (may present as chest tightness without wheeze)
- Smoking and vaping (passive or active)
- Damp, mouldy, cold or crowded housing
- Aeroallergens (in particular house dust mite, cat and dog hair)
- Insufficient income to access healthcare
Consider consultation with respiratory/ specialist asthma service when
- Inadequate asthma control achieved at Step 3
- It is unclear if asthma is the correct diagnosis
For emergency advice and paediatric or neonatal ICU transfers see Retrieval services
Parent information
See Parent resources
Additional resources
National Asthma Council Symbicort (SMART) action plans
Breathe Green Project
Green
prescribing
Last updated September 2022