Fracture Guideline Index
See also: ta
Hip dislocation - Fracture clinics
1. Summary
|
ED management
Hip dislocation in children is rare. It is generally a result of significant trauma.
The key to clinical diagnosis is the abnormal position of the limb, with the inability to move the hip.
All hip dislocations require reduction in theatre and should have prompt orthopedic assessment. |
2. How are they classified?
Hip dislocations can be described by the direction of the dislocation. The femoral head can be dislocated posteriorly (most common), anteriorly or very rarely inferiorly.
Hip dislocations can also be described by presence of associated injuries:
- Dislocation without fracture (most common)
- Dislocation with fracture, e.g. acetabular, femoral head or femoral neck fracture
3. How common are they and how do they occur?
These are rare injuries. In older children, they usually result from significant trauma, such as motor vehicle accidents or falls from height. In younger children (
<5 years) hip dislocation can occur after minor trauma.
4. What do they look like - clinically?
✓ |
The key to clinical diagnosis is the abnormal position of the limb, which the patient is completely unable to move. |
The patient will be uncomfortable and not want to move the affected leg. The affected leg will appear shorter than the non-injured side.
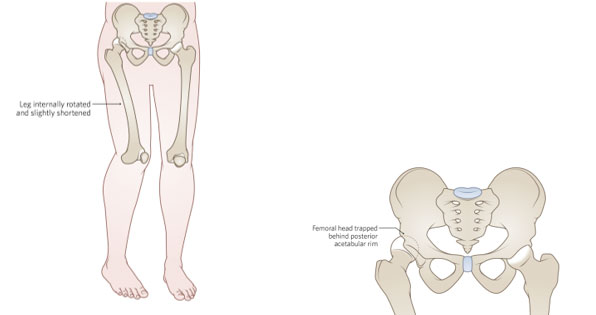
Posterior dislocation - the leg is usually adducted and internally rotated with the hip in a flexed position as above
Anterior dislocation (rare) - the leg is usually abducted and externally rotated.
5. What radiological investigations should be ordered?
Anteroposterior (AP) pelvis x-ray should be obtained to confirm the diagnosis, with another following reduction to confirm success.
A post-reduction MRI should be arranged. MRI is preferable to CT as it is better able to detect loose bodies, cartilage injuries and labral entrapments, particularly in younger children.
6. What do they look like on x-ray?
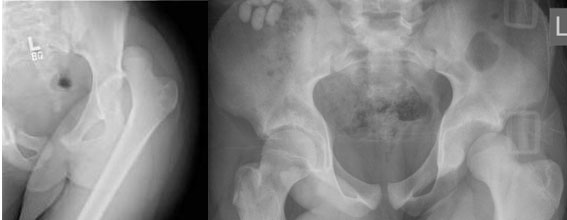
Posterior dislocation of the left hip in two different patients.

Posterior dislocation right hip with fracture of the bony acetabular rim both superiorly (long arrow) and inferiorly (short arrow). Some acetabular labral injuries are purely cartilaginous, hence the recommendation for post-reduction MRI.
7. When is reduction (non-operative and operative) required?
All hip dislocations need urgent reduction. Prolonged dislocation carries a much higher risk of avascular necrosis to the head of femur, as well as being painful for the child.
Reduction should occur in the operating theatre, as the degree of sedation and muscle relaxation which can be obtained there allows for a more controlled relocation of the injury and reducing chance of iatrogenic injury, and attempts at closed reduction are not always successful. Restricted access to an operating theatre may tip the risk:benefit calculation in favour of reduction under procedural sedation in the Emergency Department.
8. Do I need to refer to orthopaedics now?
Yes. All hip dislocations should have rapid orthopedic assessment.
9. What is the usual ED management for this injury?
Ensure that adequate analgesia is provided and screen for any other injuries in a complete trauma secondary survey.
All hip dislocations should have prompt orthopaedic assessment and management.
Management of any associated fracture is covered in a separate guideline
10. What follow-up is required?
Any follow-up should be arranged by the orthopaedic service. This will generally involve long term surveillance to monitor for avascular necrosis.
11. What advice should I give to parents?
The child will be assessed and treated by the nearest orthopaedic on call service. It is important that this be expedited.
There can be complications associated with this injury; the orthopedic team will discuss these with parents. Ongoing orthopaedic care will be required following reduction.
12. What are the potential complications associated with this injury?
Avascular necrosis (AVN) of the femoral head is the most common complication. This can occur due to disruption of the blood supply to the femoral head as a result of the injury. The risk is reported between 3-15%. The risk has been shown to be significantly if the hip is not reduced within 6 hours post-injury.
Other complications are less common, but include
-
nerve injury (2-10%)
-
femoral head over growth (coxa magna)
-
osteoarthritis (those injuries with acetabular fractures)
-
recurrent dislocation
-
growth arrest
See fracture clinics for other potential complications.
References (ED setting)
McCarthy JM, Noonan K. Fractures and traumatic dislocations of the hip in children. In Rockwood and Wilkins' Fractures in Children, 7th Ed. Beaty JH, Kasser JR (Eds). Lippincott Williams & Wilkins, Philadelphia 2010. P.769-96.
Mehlman CT et al. Traumatic hip dislocation in children. Long-term followup of 42 patients. Clin Orthop Relat Res. 2000;(376):68-79
Thanacharoenpanich S, et al MRI is Better than CT Scan for Detection of Structural Pathologies After Traumatic Posterior Hip Dislocations in Children and Adolescents. J Pediatr Orthop. 2020;40(2):86-92.
Vialle R, Odent T, Pannier S, et al. Traumatic hip dislocation in childhood. J Pediat Ortho 2005; 25(2): 138-44.
Last updated November 2020