Table of contents will be automatically generated here...
Introduction
Establishing a patent airway that allows adequate oxygenation is a key priority in the management of trauma patients. This chapter will cover how to assess and manage airway problems in the infant or child trauma patient.
How are children different?
(see how children are different section)
Apart from their obvious smaller size and the growing process, children have important anatomical and physiological differences, relative to adults, which are significant in airway management:
- Narrower airways- they are more easily obstructed by oedema, blood foreign bodies and external compression. Even mild narrowing can lead to rapid increases in airway resistance and subsequent work of breathing.
- Larger tongue and adenoids - increased risk of obstruction, along with increased difficulty of laryngoscopy and visualising the vocal cords.
- The soft structures of the paediatric upper airway are also more prone to injury from multiple attempts at intubation.
- Longer floppy epiglottis - as such in infants a straight blade laryngoscope may be preferred for intubation.
- Higher anterior larynx.
- Shorter trachea. Chest film is required to confirm ETT position
- Larger occiput - this results in the neck being flexed when a child is lying supine on a flat surface - contributing to airway occlusion
- Increased metabolic requirements and reduced functional residual capacity lead to rapid desaturation
Who manages the airway in paediatric trauma?
At the Royal Children's Hospital, once the trauma team has been activated, a senior anaesthetist should typically be allocated the role of airway doctor. This role however, may also be filled by a PICU or ED registrar / consultant, depending on the mix of staff
available, and the particular needs of the patient. The assumption is always that the person best suited to the role, and ensuring the best outcome for the patient, is allocated this role. Even in the severely injured child, intubation is rarely required immediately. The primary
importance of securing the airway is to allow for oxygenation of the patient. The airway often can, and should, be opened and kept patent through appropriate positioning, simple airway manoevres (such as a jaw thrust) and adjuncts (such as an oropharyngeal airway). These techniques combined
with the application of high flow oxygen will in most cases allow sufficient time for the arrival of an appropriately skilled intubator, and adherence to an intubation checklist / plan.
It is recommended that only an experienced clinician should attempt to intubate a child - unless the procedure is immediately required to save a life.
Primary survey
The life threat to identify and manage when assessing the airway is actual or impending airway obstruction
Mechanisms of airway obstruction
- Direct trauma to the airway or surrounding structures. This may include:
- Maxillo-facial / laryngeal / tracheal injury or compression due to anterior neck haematoma
- Burn-associated oedema of mouth, pharynx, larynx.
- Contamination of the airway due to debris - for example with vomitus / blood / teeth or other foreign bodies
- Loss of pharygeal tone - due to head injury or intoxication with drugs/alcohol
- Incorrect positioning - hyperflexion of the infant due to their large occiput
Airway Assessment
The airway doctor should assess the upper airway and the anterior neck looking for signs of airway obstruction.
Signs of airway obstruction
- Respiratory distress which may be characterised by:
- An increase in respiratory rate
- Paradoxical movement of the chest and abdomen
- Use of accessory muscles with sternal, intercostal and subcostal recession
- Intrathoracic obstruction (of trachea or bronchi) may present with wheeze or prolonged expiration
- Extrathoracic obstruction may present with:
- stridor / hoarseness or voice change (laryngeal or upper tracheal injury injury),
- gurgling (contamination of the oro-pharynx) or
- snoring (loss of pharyngeal tone due to reduced level of consciousness leading to occlusion of airway)
- Cyanosis / Low SpO2
- Visible swelling of the tongue, pharynx or neck
- External signs of injury to face, mouth, mandible or neck
- Non specific effects on other organ systems - tachycardia / decreased conscious state / restlessness
Examination of the anterior neck
The airway doctor is also responsible for examining the anterior neck. The goal is to seek signs of impending or actual airway obstruction at the laryngeal or tracheal level, or signs of thoracic life threats such as a tension pneumothorax / cardiac tamponade. The signs to look for can be remembered using the mnemonic TWELVE-C, as below:
- Tracheal deviation - may be caused by a tension pneumothorax or a massive haemothorax (with tension)
- Wounds - blunt or penetrating wounds to the neck may directly injure the airway, or lead to swelling that will progressively obstruct it
- Emphysema (subcutaneous) - indicates a pneumothorax or pneumomediastinum has occured
- Laryngeal tenderness / crepitus - may suggest a laryngeal fracture or other injury (typically occurs with a "clothes-line" type injury to the neck
- Venous distension - associated with obstructive shock secondary to a tension pneumothorax or cardiac tamponade
- oEsophageal injury (unlikely if able to swallow easily) - not an immediate life-threat but perforation is associated with a high mortality
- Carotid haematoma / bruits / swelling - a rapidly expanding haematoma may lead to airway obstruction, carotid injury is also associated with subsequent increased stroke risk
Airway management
Immobilise the cervical spine - manual in-line stabilisation
(see cervial spine assessement clinical practice quideline)
Maintain head in neutral position
- Children have relatively large heads when compared to adults. As a result when laid on a flat surface they tend to flex their neck, which may compromise both their airway and their cervical spine. A neutral position can be obtained by raising the child's thorax by placing towels or a specialised device under their shoulders and back.
- At RCH, this is achieved through the use of the Thoracic Elevation Device (TED). This is used for children less than 8 years old. It should be available and placed on the ED trolley prior to arrival of the patient. It is folded to full thickness (four layers) for children aged 0-6 months, and to half thickness (two layers) for children aged 6 months to 8 years (see also
Thoracic elevation device - Airway pad CPG)
- If the Thoracic Elevation Device is not available, a neutral position can be achieved in infants (up to one year old) by placing 1-2 folded towels under the trunk, from buttocks to shoulders. This allows the occiput to be 1-2 cm lower than the back, and allows the head to rest in a neutral position. A rolled towel can be placed under the shoulders of older children to achieve a neutral position of the head and neck.
Open the airway
- In trauma, always use jaw thrust. (Not head tilt or chin lift) (Place fingers behind the angles of the mandible and push anteriorly (towards the tip of the nose)
Jaw thrust

Clear the airway
- If you hear gurgling noises due to fluid in the airway, gently suction the pharynx via a soft 10 FG suction catheter (infants) or a Yankauer sucker (older children) under direct vision, using a laryngoscope or a tongue depressor. Try not to touch the mucosa, as
this may cause bleeding or laryngospasm.
If an obstruction persists
- Optimise the head position, and reopen the airway using a jaw thrust.
- Rapidly examine the mouth with a laryngoscope.
- Remove any visible foreign body using Magill forceps or Yankauer sucker.
- If the airway is adequate during laryngoscopy but inadequate at other times, insert an oropharyngeal airway.
Oropharngeal Airway (OPA)
- An airway of the right size reaches from the central incisors to the angle of the child's mandible
Sizing of OPA

Guedel airways

Insertion
- Insert under direct vision, concave side down, using a tongue depressor.
- If the airway remains inadequate: consider tracheal intubation if the facilities are available to do this safely and quickly.
If you are unable to intubate the
child whose airway is inadequate:
- Send urgently for expert help - ICU Registrar/ENT surgeon/ anaesthetic registrar.
- Use jaw thrust and gentle oropharyngeal suction to clear the airway using airway adjuncts, such as Guedel.
- Give OXYGEN via facemask and monitor.
- If the child has inhaled a foreign body, or has a partly transected trachea or larynx, and is breathing adequately while partly obstructed, don't try to intubate but give O2 by mask. Reassure the child and family and stay with the child until expert
help arrives.
Intubation
Indications for Intubation
- Airway obstruction persists despite oropharyngeal (Guedel) airway.
- Inadequate oxygenation despite supplemental oxygen
- Hypoventilation
- Deteriorating GCS
- Needs prolonged ventilation;
- Anticipated airway obstruction - for example due to inhalational burn injury
- Management of agitation or severe distress
- To facilitate safe transport
Preparation for Endotracheal intubation -
(see also
Emergency airway management CPG)
Pre-Oxygenate:
- Pre-oxygenate with T-piece and high flow oxygen
- Deliver positive airway pressure breaths and positive end-expiratory pressure
- Apply nasal cannulae (in the absence of suspected base of skull fracture)
- Aspirate air from the stomach via a small bore orogastric tube.
Endotracheal tube:
Where possible use a pre-printed resource to assist with drug doses and sizes of equipment such as the endotracheal tube (at RCH the standard resource is the Monash Drug Book). If this is not available, calculate the endotracheal tube (ETT) size using the below formula.
Size of cuffed ETT (internal diameter in mm) = Age/4 + 3.5
Tubes of the size calculated above, plus tube 0.5 mm ID smaller and 0.5 mm ID larger, should all be available on the child's bed.
At RCH the availability of micro-cuffed ETT, and the advantage of more completely protecting the airway with the use of these ETT's makes them the first choice when intubating children who have been severely injured.
e.g.: 6 year old child: 6/4 + 3.5 = 5.0mm in diameter.
As such on the child's bed should be 4.5, 5.0 and 5.5 mm in diameter tubes.
Endotracheal tubes
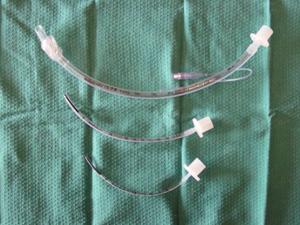
Introducer: For ET tubes 4.5 mm ID and smaller, a lightly lubricated Stiletto (PICTURE) inserted almost to the tip of the tube makes intubation easier. Oral: Always use oral, never nasal, intubation in a child with a head injury (because of the
risk of meningitis, or of entering the cranial cavity if an undiagnosed fracture of the skull base is present.
Laryngoscope: Have 2 available; check they are working
Suction:
- Check it is working
- Ensure it is a Yankauer
- Check it is next to the child's head
Drugs: Drawn up and labeled:
- Ketamine
- 0.25-2mg/kg depending on the degree of physiologic unwellness (lower dose in acute circulatory failure)
- Rocuronium
- 1.2-1.6mg/kg depending on the degree of physiologic unwellness (higher dose in acute circulatory failure)
- Saline flush 10 ml IV cannula + 3-way tap on extension tubing: all patent and visible.
Induction of anaesthesia
1. Pre-oxygenate the child:
- T-piece, high flow O2
- Positive airway pressure and positive end expiratory pressure
- 5 minutes if possible.
2. Drugs: - Always used unless the child is in cardiac arrest
- 1st hypnotic: ketamine
- 2nd muscle relaxant: rocuronium
There may be a delay between administration of the anaesthetic agent and muscle relaxant at the discretion of the team lead (for example to optimise oxygenation through titrated dose of anaesthetic agent). Prioritise avoidance of hypoxia at all times. Continue gentle positive pressure ventilation with positive end- expiratory pressure during the apnoeic period. During laryngoscopy turn the flow up on nasal cannulae to 2L/kg/minute (max 15L/min).
3. Laryngoscopy.
- Hold laryngoscope in your left hand.
- Be gentle.
- Don't lever on the teeth.
- Don't jam the lip between blade and teeth.
Up to 1year: Straight blade (Miller or
Robertshaw)
- Pass the tip over the tongue, past the tip of the epiglottis
- Lift the epiglottis to see the vocal cords.
- If you are more comfortable using a curved blade, this can also be used in this age group

More than 1 year: Curved blade (MacIntosh 2 or
3)
- Pass the tip over the tongue into the vallecula (space between tongue and epiglottis)
- Lift the handle towards the ceiling at the far end of the room to bring the vocal cords into view.

4. Insert the endotracheal tube
- Length [(Age/2) + 12] cm at the teeth - as with calculating the ETT size, the use of a cognitive aid may minimise the chance of making an error in calculating this.
- Immobilise the tube at the lips.
- Auscultate both axillae and the epigastrium to confirm tube position.
- Secure with cotton tape around neck or Elastoplast on the face
5. Insert an orogastric tube on free
drainage.
Never use a nasogastric tube or a nasotracheal tube in a child with a head injury (because of the risk of meningitis or of entering the cranial cavity where there is undiagnosed fracture of skull base).
6. Check on an AP chest X-ray: The ET tube tip should lie at the level of the medial end of the clavicles. If not, re-position the tube and re-tape.
7. Suction the ET tube carefully each hour, and more often if needed.
8. Humidify the inspired gases using a condenser humidifier (Swedish nose) between the ETT (PICTURE) tube and the self-inflating bag.
9. Splint the child's arms if necessary. (Child should be sedated)
Side effects of drugs
- Anaesthetic agents (ketamine, thiopentone, midazolam, propofol) all cause:
- Hypotension - may occur with all anaesthetic agents - including ketamine - especially in the presence of hypovolaemia. However, the hypotensive effect is likely to be more pronounced in agents such as propofol and thiopentone
- Respiratory depression - Beware of using IV hypnotics in severe airway obstruction; ensure that you can inflate the chest with bag/mask first.
- Muscle relaxants:
- Prevent breathing - Beware of using them in severe airway obstruction; ensure that you can inflate the chest with bag/mask first.
- Suxamethonium may cause severe hyperkalaemia in crush injury and burns patients (can occur up to 24 hours after burn) this causes fasciculation and severe muscle pain.
- Rocuronium at a dose of 1.2-1.6mg/kg is the preferred muscle relaxant at RCH for emergent intubation in the emergency department.
Can't intubate, can't oxygenate (CICO)
If the event of a CICO event you will need to progress to either a:
- Surgical cricothyroidotomy (> 12 years)
- Needle cricothyroidotomy (any age; may be used to gain time during surgical cricothyroidotomy)
Needle cricothyroidotomy
(see airway procedures section)
Useful for obstruction in the larynx or above, but not if there is obstruction in the trachea or bronchi. It improves oxygenation slightly, and buys 10-15 minutes' time for help to arrive, and for the establishment of a definitive airway.
- Continue bag/mask ventilation with O2
- Prepare equipment: -IV cannula: largest available (10 - 16 SWG), with 5 ml syringe
- Oxygen tubing + 3-way tap (if no 3-way tap available, cut a 3 mm hole in the side of the O2 tubing, cutting the O2 tubing if necessary, to fit over the hub of the cannula.
- Rolled towel under the child's shoulders;
- Feel your own cricothyroid membrane: this is the horizontal gap between the thyroid cartilage (Adam's apple) above, and the horizontal cricoid cartilage below.
- Stand on the child's left and locate the same structures.
- Immobilise the trachea between your left finger and thumb in the child .
- Insert the cannula through the cricothyroid membrane, then 45o downwards towards the feet. STAY IN THE MIDLINE
- Aspirate continuously as soon as the needle is through the skin.
- When you can aspirate air, the needle is in the trachea; immobilise the syringe (don't pull it back) and slide the cannula down the needle into the trachea.
- Tape the cannula in place.
- Attach the O2 tubing to the cannula.
- Run O2 at 1 litre/min per year of age.
- Occlude the side hole of the 3-way tap, or the hole in the O2tubing, for 1 second. Then release for 4 sec to allow expiration.
Surgical cricothyroidotomy
(see airway procedures section)
- Continue bag/mask ventilation with O2.
- Prepare equipment: -3.5 - 4.5 ET tube -Scalpel blade on a handle - Curved mosquito forceps -Cotton tape or 2/0 silk ties -Self-inflating resuscitation bag attached to O2 outlet.
- Rolled towel under the child's shoulders;
- Feel your own cricothyroid membrane: this is the horizontal gap between the thyroid cartilage (Adam's apple) above and the horizontal cricoid cartilage below;
- Stand on the child's left and locate the same structures;
- Immobilise the trachea between your left finger and thumb;
- Make a 1.5 cm vertical incision down to the trachea over the cricothyroid membrane;
- Spread the skin edges with your finger and thumb;
Stay in
the midline
- Carefully stab through the cricothyroid membrane with the scalpel blade oriented transversely;
- Rotate the blade through 90o to open the hole and keep it in place;
- Insert the endotracheal tube straight backwards beside the scalpel; When you feel it enter the trachea, push it downwards into the lower trachea;
- Immobilise the tube and tape it in place;
- Ventilate with the self-inflating bag +O2
- Auscultate both axillae and epigastrium to confirm tube position;
- CXR to check tube length;
- Orogastric tube on free drainage.
If the lungs do not inflate easily, possible reasons are:
- The ET tube is not in the trachea. Most likely cause. Start again!
- Bilateral tension pneumothoraces. Less likely: consider
needle or
finger thoracostomies
- Foreign body completely obstructing the lower trachea. Unlikely: try passing the ET tube further down the trachea.
The main problems of needle and surgical cricothyroidotomy are:
- Failure to enter the trachea: hold the trachea firmly and stay in the midline.
- Bleeding: Apply pressure with a swab. Tie off large bleeders.
- Damage to local structures (oesophagus, pleura causing pneumothorax, arteries, veins, nerves).
- Tracheal transection, if too wide an incision is made during surgical cricothyroidotomy.
- Damage to the trachea or larynx.
- Infection.
Specific airway problems in trauma
Airway injury
Be suspicious in the following injuries:
- Fall onto sharp object;
- Running/riding into hidden wire;
- Motor vehicle accident: A blow from dashboard / front seat;
- Penetrating injury to the neck.
In each case consider ruptured larynx or trachea: Look for subcutaneous emphysema
Burn
For definitive burns management
see burns / management of burn wounds clinical practice guideline
Airway management is a
priority.
Airway obstruction occurs secondary to:
- Thermal injury
- Inhalation of flames/steam
- Aspiration of hot liquids
Upper airway obstruction can occur due
to inhaled smoke even in the absence of burn to the face.
If the child is exposed to fire or smoke in an enclosed space e.g.
a building or car, consider inhalation injury until proven
otherwise.
Signs of a respiratory burn injury:
- Tachyapnoea or rising respiratory rate
- Dysphagia or drooling
- Stridor
- Mouth/neck/facial burn
- Oedema of neck and face
- Respiratory distress e.g. intercostal or subcostal recession. This is a very late sign and requires immediate tracheal intubation and mechanical ventilation.
- Signs of airway obstruction
Primary survey for burn
- Airway - protect C-spine if there is any suspicion of airway compromise. Immediately consider tracheal intubation and expert review.
- Breathing -give high-flow oxygen. Assess. If there is any sign of respiratory distress, immediately consider tracheal intubation and expert review.
Suggested reading list
- Advanced Paediatric Life Support. 3rd ed. London: BMJ Books 2001. Chapters 4 (Basic life support); 5 (Advanced support of the airway and ventilation); 22 (Practical procedures: airway and breathing).
- Taussig L, Landau L, Le Souëf P; Martinez F; Morgan W; Sly P (eds) (2nd edition) Pediatric Respiratory Medicine. St Louis: Mosby 2007. Chapters 1 (Assisted ventilatory support and oxygen treatment) and 27 (Lung trauma: toxin inhalation and ARDS).
- Fleisher G, Ludwig S (eds): Textbook of Pediatric Emergency Medicine (4th ed). Philadelphia: Lippincott 2000. Chapters 1 (Resuscitation: pediatric basic and advanced life support); 5 (Emergency airway management: rapid sequence induction); 104 (Major
trauma); 106 (Neck trauma); 107 (Thoracic trauma); 112 (Otolaryngologic trauma); 114 (Burns).
- Bersten A, Soni N (eds): Oh's Intensive Care Manual (5th ed) London: Butterworth Heinemann 2003. Chapters a (The critically ill child); b Upper airway obstruction in children; c (Acute respiratory failure in children; d (Paediatric trauma).
- Macnab a, Macrae D, Henning R (eds): Care of the critically ill child. London: Churchill Livingstone 1999. Chapters 2.6 (Trauma: cranial, spinal and multiple); 4.2 (Smoke inhalation); 4.4 (Trauma of individual systems); 6.2 (Intubation); 6.3 (Securing the
airway); 6.4 (Assisted ventilation).