Type 1 diabetes is a condition that occurs when the body loses its ability to produce a hormone called insulin. This life-long autoimmune condition affects over 120,000 people in Australia alone and is predominately diagnosed in childhood. Insulin is normally produced by the pancreas and allows glucose (sugar) to move from the blood to tissues such as muscle where it is required for energy.
A children's guide to type 1 diabetes
An adult's guide to type 1 diabetes
What are the symptoms of type 1 diabetes?
Type 1 diabetes may cause some of the following symptoms. If you think you or someone you know has these symptoms, seek medical help immediately, and drink sugar-free fluids to prevent dehydration.
- Extreme thirst
- Constant hunger
- Sudden weight loss
- Frequent Urination
- Blurred Vision
- Nausea
- Vomiting
- Lethargy
- Infections
When there is not enough insulin the blood glucose levels build up and eventually "spill over" into the urine. This results in excessive urine production and thirst. Thus, prior to treatment, affected children and adolescents have usually had the symptoms of thirst and increased urination for some time (usually 2-3 weeks). If this situation is allowed to progress unchecked, fat stores begin to break down, weight loss occurs and the blood becomes increasingly acidic. Eventually affected people become dehydrated, start vomiting and lose consciousness. This is called diabetic ketoacidosis (DKA).
The treatment of type 1 diabetes involves replacement of insulin. Insulin can be replaced in the body either via insulin injections (twice daily insulin or four injections per day) or with insulin pump therapy. Checking blood glucose levels provides information on how much glucose is currently in the bloodstream and is a crucial part of managing diabetes. It is the only way to know if the body is getting the correct amount of insulin that it needs. Managing diabetes involves balancing insulin, food, and exercise.
When people are first diagnosed with type 1 diabetes, they will be medically stabilised and start on insulin injections. They will usually be required to stay in hospital for a short period of time to commence diabetes education which can then be finished as an outpatient after discharge. These education sessions will be with a diabetes nurse educator (approx. three-four sessions), dietitian (approx. two sessions), and social worker (approx. one session).
The goal of diabetes education is to provide the needed support to young people and their families to feel comfortable and confident with diabetes management in their day to day life.
A young person with diabetes will have an appointment with an endocrinologist (diabetes doctor), diabetes educator and dietitian a few weeks after their diagnosis. Following this appointment, diabetes care involves an outpatient appointment every 3-4 months with the endocrinologist.
Diabetes nurse educators, diabetes dietitians and social workers are available to be contacted in between the young person’s doctor appointment for support with diabetes management.
Long term management and HbA1c targets
It’s important to note that despite our best efforts, blood glucose levels (BGLs) will not always be in our target of 4-7 mmol/l pre meals. Variations will happen on a daily basis, sometimes they will be low i.e. less than 4mmol/l and other times high i.e. greater than 7 mmol/l. Often we can account for blood glucose levels that are out of the target such as the impact of food which may raise BGLs or exercise that may lower BGLs.
Every 3 – 4 months, children with type 1 diabetes will have a blood test called an HbA1c. These blood tests measure the amount (as a percentage) of haemoglobin in red blood cells that has glucose attached to it. The higher the glucose levels in the blood (the more BGLs out of target per day/week) the more will become attached to the haemoglobin.
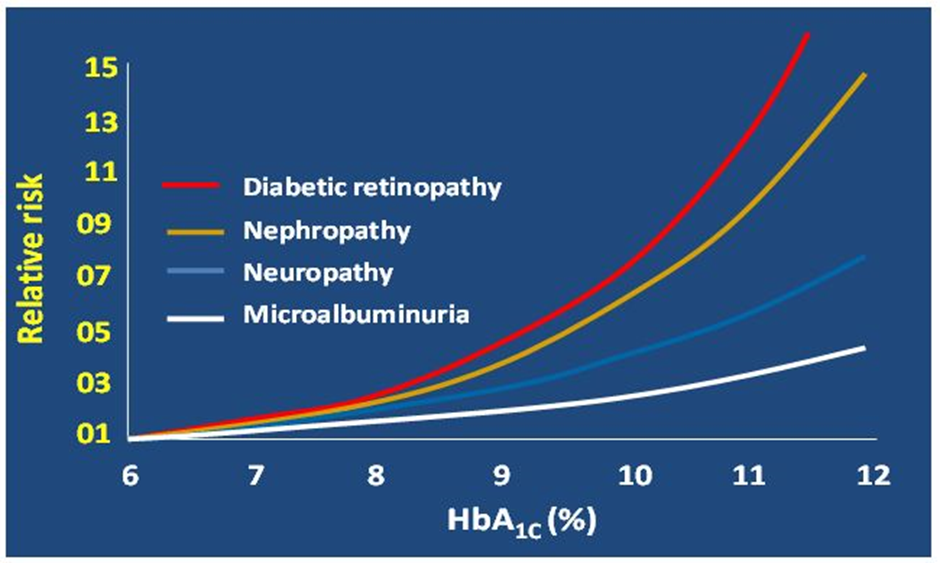
At the RCH we aim for any HbA1c 7% or less. If a child has any HbA1c higher than this on a regular basis, their risk of developing complications will increase dramatically.
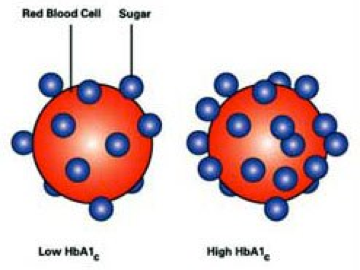
Remember: BGLs in target range = HbA1c in target range.
At the RCH we expect our children to enjoy long and healthy lives so the aim of our diabetes management during childhood and adolescence is to allow day to day activities and quality of life whilst minimising the risk of long-term diabetes related complications. We do this by encouraging regular reviews of your child’s BGL’s, adjusting insulin doses in response to patterns and performing the HbA1c test every three months in clinic.
Targets can be achieved by ongoing contact with a dedicated paediatric diabetes care team, education and motivation to maintain a healthy lifestyle with particular emphasis upon diet and exercise. The diabetes team can teach you how to adjust your child’s insulin and support you to become independent with this over time.
All children who have been diagnosed with type 1 diabetes at the RCH will have a fingerprick blood test done in clinic every three months to test their HbA1c. This test is the best measure for long-term blood glucose control. It can tell us about how much glucose has been circulating in the blood stream on average over the last three months which tells us about the relative risk of complications associated with chronically (long term) elevated blood glucose levels. (See graph below)
This can be achieved by ongoing contact with a dedicated paediatric diabetes care team, education and motivation to maintain a healthy lifestyle with particular emphasis upon diet and exercise. The diabetes team can teach you how to adjust your child’s insulin.
A blood glucose level (BGL) measures the concentration of glucose in the blood at the time of the test. Performing blood glucose test is the only way you will know how to determine the correct dose of insulin to give. You need to know how to adjust insulin doses.
BGL’s need to be checked a minimum of four times a day:
- Before breakfast
- Before lunch
- Before dinner
- Before supper
- Overnight 2-3 times a fortnight.
BGL’s may need to be tested at other times of the day:
- If hypo is suspected
- If you feel unwell
- Before commencing sport or exercise
- Before driving a car
The target range BGLs is 4.0mmol/L – 7.0mmol/L prior to main meals.
An assessment of blood glucose levels tell you if you are getting the correct dose of insulin. Growing children will require regular insulin dose adjustment.
- If the BGL’s are consistently less than 4.0mmol/L you are getting too much insulin
- If the BGL’s are consistently above 7.0mmol/L before meals you are not getting enough insulin
All BGL readings and insulin doses should be recorded in a record book. Keeping a detailed record of your BGL’s allows you to assess if you need to make changes to your insulin doses.
Always wash and dry hands before taking a BGL as food on your fingers can alter the BGL reading.
The ACCU-CHEK FastClix lancing device has been proven to be the least painful and overall easiest to use. This should have been provided for you to use at diagnosis. For video instructions on how to use the lancing device please
click here. NOTE: the RCH advices that lancets should only be changed once a day not at each BGL test as per the video
Printable version
What is hypoglycaemia?
Hypoglycaemia (“Hypo”) means a low level of glucose in the blood. For people with type 1 diabetes, this is a blood glucose value of less than 4.0 mmol/L. Mild to moderate hypoglycaemia is common and is an expected to occur in good diabetes care. True physiological hypoglycaemia does not occur until the BGL is less than 3.5mmol
Hypoglycaemia can be caused by:
- Too much insulin
- Vigorous exercise without extra carbohydrate
- Missing or delayed meals
- Not eating all serves of carbohydrate
- Alcohol intake
Or, there may be no obvious reason.
People affected by hypoglycaemia may start to experience symptoms when the blood glucose level is less than 4mmol/l, or more commonly when the BGL is less than 3.4mmol Sometimes the blood glucose level can be lower than this and no symptoms are experienced, this is referred to as "hypo unawareness".
Common signs and symptoms of hypoglycaemia are:
- paleness
- heart pounding
- shakiness
- irritability, change in mood
- headache
- lack of concentration
- sweating
- confusion, vagueness
- feeling hungry
- crying
- dizziness
- weakness
All BGLs less than 4mmol need to be treated, regardless of their signs and symptoms.
Mild hypoglycaemia is common and is an expected to occur in good diabetes care.
Note: The treatment must be taken to the person having the hypo. Never make them walk to get treatment as this may exacerbate the hypo.
Treatment
A blood glucose test should be done to confirm the hypoglycaemia before treating. Treat the hypo if the blood glucose level is 3.9mmol or lower. Do not delay treatment.
Step 1
Give 5-10grams of high GI (quick acting) carbohydrate to raise the blood glucose levels quickly
Treatment options are based on age
5 years old or younger, or less than 25kg give 5 grams
6 years old and older, or more than 25kg give 10 grams
e.g.
- 60-120mls Juice
- Glucose tablets (1.5-2 TRUEplus™ or 3-6 Glucodin™)
- Polyjoule/Sucrose Solution
- 50-100ml Lemonade
- 100-200ml Cordial
- 1-2 teaspoon Honey
- 2-4 jelly beans(Glucojel™)
Step 2
WAIT 15 minutes, perform another blood glucose test.
If BGL remains under 4mmol/L : REPEAT Step 1.
If BGL is above 4mmol/L : Proceed to Step 3
Step 3
Give 10-15 grams of a sustaining (low GI) carbohydrate to keep the blood glucose in the target range.
e.g.
- 4 - 6 Savoy biscuits/7-10 rice crackers
- 200-250mls of milk
- 1 apple or small banana
- ½ cup of fruit yoghurt
- I slice of bread
If a hypo occurs within 20 minutes of meal time, please use the meal as your STEP 3, low GI carbohydrates.
If hypoglycaemia occurs immediately before a meal when insulin is due:
- Give a sugar serve, wait a few minutes until feeling better
- Give the normal dose of insulin
- Serve the meal immediately
Remember that the less sticky the hypo treatment, the better it is for good dental hygiene. Regular flossing and brushing will also help this!
You can see in the picture below, hypo’s must be treated with high GI carbohydrates immediately to raise blood glucose levels quickly. Following on with low GI carbohydrates, will minimise the chance of repeated hypoglycaemia once the initial fast acting high GI food has worn off.

Over treating hypoglycaemia can be a problem for many families. If you are experiencing high BGLs after treating a hypo, please contact the diabetes allied health team to discuss hypo treatment.
Tips for assisting with hypoglycaemia
- Always carry fast acting high GI carbohydrates on you at all times
- Hypo treatment should be kept at school, in the car and other places that are easily accessible
- Check blood glucose levels whenever possible to confirm hypoglycaemia
- Do not ignore mild symptoms. Do not delay treatment
- Eat meals and snacks on time
- Supervise your child’s injections
- Never give rapid acting insulin unless food is available
- Give extra serve of low GI carbohydrates before any activity
- Teach family and friends how to recognise and treat low blood glucose levels
- If low blood glucose levels continue to happen without explanation, please contact the diabetes team.
- Wear a diabetes identification bracelet at all times.
Hypoglycaemia on an insulin pump
The treatment of a hypo changes on an insulin pump. There is less circulating insulin in the body, which means less carbohydrate needs to be consumed to treat the hypo.
- A BGL less than 4.0 mmol/L is hypo and needs immediate treatment
- BGL must be above 4.0 mmol/L to bolus for a meal or snack
- Common reasons for BGL going low on a pump:
Too much insulin (basal, carb ratio or sensitivity setting)
Exercise without reducing basal rate
Eating less carbohydrate than you bolus for
Alcohol
Mild Hypoglycaemia: BGL between 2-4 mmol/L
- Give QUICK ACTING carbohydrate only (5 grams if ≤5 years old, 10 grams 6 years old and over) e.g. glucose tablets or fruit juice. DO NOT BOLUS FOR THIS TREATMENT,
- Enter BGL in the pump after hypo treatment
- Rest until you feel better
- Recheck BGL in 15 mins. If your BGL is still under 4.0 mmol/L repeat the treatment.
- After 1st hypo BGL entry, do not put further BGL readings in the pump for 1 hour
- When BGL is above 4.0 mmol/L all carbs eaten must be bolused. (Do not enter BGs for one hour after initial hypo entry)
Moderate Hypoglycaemia: BGL below 2.0 mmol/L
- Give QUICK carbohydrate (5 grams if ≤5 years old, 10 grams 6 years old and over) e.g. glucose tablets or fruit juice.DO NOT BOLUS FOR THIS TREATMENT,
- Enter BGL in the pump after hypo treatment
- Then eat 15 grams LONG ACTING Carbohydrate e.g. Milk or crackers. DO NOT BOLUS FOR THIS TREATMENT
- Rest until you feel better
- Recheck BGL in 15 mins
* If BGL still Below 2.0 mmol/L repeat the above treatment
* If BGL between 2-4 mmol/L give QUICK ACTING serve of carbohydrate
When BGL is above 4.0 mmol/L all carbs eaten must be bolused. (Do not enter BGLs for one hour after initial hypo entry)
Severe hypoglycaemia
A severe hypo has occurred if your child’s BGL is less than 4mmol and is unconscious, is having a seizure (fitting), is too drowsy to eat or drink or is being uncooperative. If this occurs, please do not attempt to administer anything by mouth.
Call 000 for an ambulance
Glucagon is a hormone that raises the blood glucose level by making the liver release its store of glucose into the bloodstream. This medication can be used to treat your child if they are having a severe hypo.
Glucagon is a very safe medication to give and is injected into either the subcutaneous tissue or the muscle to raise blood glucose levels. If it is possible to do a blood glucose check before administering Glucagon, please do so.

Instructions for administering Glucagon:
- Place the child on their left side in the coma position to prevent anything from being breathed into the lungs.
- If you haven’t already called an ambulance, please do so. Call 000.
- If possible please do a blood glucose check
- Remove the orange plastic cap from the bottle of white powder (glucagon) and the needle guard from the syringe containing sterile water.
- Inject all the water into the bottle containing glucagon. Leave the needle in the bottle. The glucagon will dissolve into the fluid with gentle rotation of vial.
- Turn the bottle upside down. Pull ½ the needle out of the bottle to keep the end of the needle in the solution.
- Draw up the glucagon into the syringe.
- Inject all the glucagon into a muscle on the outside of your child’s thigh.
How much glucagon do I give my child?
- 0.5mls: Children who weigh less than 25kg or less than 6 years old
- 1ml: Children who weigh more than 25kg or who are older than 6 years old
How long will it take my child to recover after giving them glucagon?
Glucagon may take 5 to 15 minutes to work, therefore don't expect an immediate improvement.
What do I do after I have given my child glucagon?
Glucagon can cause nausea, vomiting and headache.
Once your child is rousable, encourage high GI carbohydrates fluids such as juice or lemonade. Because Glucagon depletes glycogen stores, you must be give your child sugary food or drink by mouth as soon as they have roused and are able to take it. This will prevent the occurrence of secondary hypoglycaemia.
Within the hour it is important to give a low GI carbohydrate, such as bread or milk in order to prevent recurrence of the hypoglycaemia and assist in return to normal eating. The liver needs to replenish its store of glycogen before glucagon can work again
Monitor blood glucose levels every 15 minutes for the first hour then every hour for 4 hours.
If you have had to use glucagon, please contact the Royal Children's Hospital to discuss further management over next 24 hours.
Blood glucose levels are often elevated following a severe hypo. Any high blood glucose levels after a severe hypo requiring glucagon should not be treated with extra insulin.
Expired Glucagon
Novo Nordisk provides a service with the ability to register to activate a reminder for when your hypoglycaemia medication is due to expire.
Please follow this link to register your glucagon.
Printable version
Ketones
Ketones are produced when the body breaks down fat for energy when there is insufficient insulin for cells to access glucose. Ketones occur most commonly when there is not enough insulin in the body. They are acidic and are dangerous if they build up in the blood as they cause a life threatening condition called Diabetic Ketoacidosis DKA.
Small amounts of ketones are normal ( 0.0 – 0.6mmol).
What is Diabetic Ketoacidosis (DKA)?
Diabetic Ketoacidosis (DKA) is a life threatening condition that occurs when there is insufficient insulin and blood ketones are abnormally high. High ketones are often associated with very high BGLs as well. The high ketones cause imbalances in body fluid and salt levels, leading to dehydration and build-up of acids in the blood. Vomiting and increasing drowsiness result. DKA requires urgent medical assistance.
What causes DKA?
- Missing insulin injections
- Illness
- Previously undiagnosed type 1 diabetes
What are the signs and symptoms of DKA?
DKA can develop rapidly and requires urgent medical assistance. Signs and symptoms may include
- High blood glucose levels with ketones present
- Tummy pain
- Vomiting
- Dehydration
- Rapid, shallow breathing
- Acetone smell on the breath
- Confusion
- Drowsiness which may lead to coma
How do I check for ketones?
- Ketones can detected in the blood and in the urine.
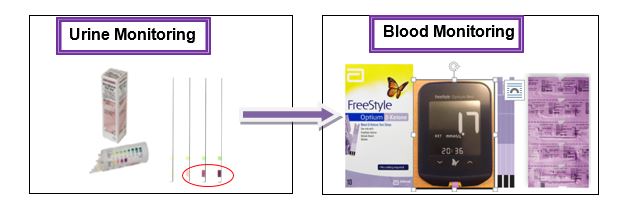
Urine ketones are positive if a colour change occurs (+, ++ or +++). If positive urine ketones check blood ketones.
When do I need to check for ketones?
- When the blood glucose level is greater than or equal to (>) 15 mmol/L
- Whenever your child is unwell, no matter what the blood glucose is.
Ketones do not need to be checked more frequently than every four hours if they are less than 1.0mmol/L
Action is required if keytones are greater than 1.0mmol/l
What should I do if my child’s ketones are greater than 1.0mmol/L and they are on injected insulin?
1. If BGL greater than (>)15mmol/L:
- Give 10% of total daily insulin dose using rapid acting insulin (Novorapid or Humalog) immediately
- Total daily dose is calculated by adding all insulin doses for a usual day and dividing by 10. This equals 10% of total daily insulin dose.
- If insulin is due, add 10% of total daily insulin dose to normal insulin dose
- If insulin is not due, give 10% of total daily insulin dose as an extra injection immediately
- Check ketones in 2 hours and seek medical advice if ketones remain > 1.0 mmol/L
- Extra insulin may be required if BGL remains >15mmol/L & ketones remain > 1.0 mmol/L after 2 hours
2. If BGL 8.0mmol/L - 15mmol/L:
- Consider giving 5 -10% of total daily insulin dose using rapid acting insulin.
- Encourage extra carbohydrate to maintain BGL
- Check ketones in 2 hours and seek medical advice if ketones remain > 1.0 mmol/L
3. If BGL 4.0mmol/L – 7.9mmol/L:
- Encourage extra carbohydrate to maintain BGL
- Give normal insulin dose
- Check ketones in 2 hours and seek medical advice if ketones remain > 1.0 mmol/L
4. If BGL < 4.0mmol/L:
- Treat hypo and encourage sweetened fluids
- Seek medical advice if insulin is due – reduction in insulin dose may be required
- Check ketones in 2 hours and seek medical advice if ketones remain > 1.0 mmol/L
Remember
- If vomiting and ketones present, call the RCH early for support with insulin doses
- If unsure of appropriate treatment, call the RCH and ask for the sick day diabetes service:
- The RCH switchboard 9345 5522
What do I do if my child is on a pump?
Positive ketones = 0.6 mmol/L or higher.
If you have ketones you have not been receiving adequate insulin.
Insulin pump therapy carries a much higher risk for developing ketones than injected insulin because if there is interruption to insulin delivery, there is no background or long acting insulin
Insulin pump users need to have access to injected insulin at all times.
A ketone reading of 0.6mmol/L and higher is positive and needs immediate treatment:
- Inject emergency dose of short acting insulin via pen or syringe
- Calculate emergency dose dividing your pump total daily dose of insulin by six (PTDD÷6)
- Do a full line and cannula change
- Check BGL’s and ketones 2 hourly (Do not enter a BG into the pump for at least 2 hours). Bolus for any carbs consumed.
Please update and record your PTDD regularly and keep it with your emergency pack.
How do I know what my child’s PTDD is?
Pump total daily dose (PTDD) can be found in the pump or on the download.
Medtronic Veo
In utilities menu, daily totals, daily average, 7 days to average, total insulin: Page 2 of download, right hand side – statistics box
Medtronic 640G
History menu, summary, 7 days, TDD: Page 2 of download, right hand side – statistics box
Medtronic 670G
Options, history, summary, 7 days, total daily dose.
Tandem T slim
Options, pump history, delivery summary, 7 day average, total insulin
With type 1 diabetes, the body does not produce insulin. This means that giving insulin injections is a vital part of managing type 1 diabetes in children and adolescents.
Insulin is usually made by the beta cells in the pancreas. In type 1 diabetes, the beta cells are destroyed and can no longer make enough insulin to meet the body’s requirements.
What is insulin and why do we need it?
Insulin is the hormone needed to move the glucose from the bloodstream into the cells. Insulin is the “key” which opens the door of the cell, allowing glucose to flow inside. Without insulin most of the organs cannot take up glucose.
When there is not enough insulin in the body the glucose stays in the bloodstream. The blood glucose level rises very high because it cannot move into the cells. The body tries to clear the glucose from the bloodstream by offloading glucose in the urine.
"When glucose cannot be used for energy the body uses fat instead. If fat is used for energy, some harmful substances called ketones begin to build up in the blood. The ketones that build up will make the person with diabetes very sick"
- Diabetes in Children and Adolescents, 3rd ed, 2010
When a person is diagnosed with type 1 diabetes, insulin needs to be replaced by an injection of manufactured insulin. This insulin is made in a laboratory and does not use any animal products.
Insulin is essential for survival. There is never a time when the body should be without insulin. There is no alternative treatment to insulin.
What are the different types of insulin?
There are a number of different types of manufactured insulin available: rapid-acting, short-acting, intermediate-acting and long-acting.
The types and combination of insulin will be advised by your treating Endocrinologist.
Rapid acting insulin
- Begins to work 5-15mins after injection
- Can last 3-5hrs
- Will be working at its peak action between 1-3hrs
- Is a clear solution
- Please give immediately before food
Short acting insulin
- Begins to work 20-30mins after injection
- Can last 5-8hrs
- Will be working at its peak action between 2-4hrs
- Is a clear solution
Intermediate acting insulin
- Begins to work 1-2hrs after injection
- Can last 16-24hrs
- Will be working at its peak action between 4-12hrs
- Is a cloudy solution
Long acting insulin
- Provides a steady level of insulin over 24hrs
- No peak
- Clear solution
- Please give at the same time each day
When you have a child with type 1 diabetes, it’s important you know how to change insulin doses in response to ‘patterns’ of hyperglycaemia (highs) and hypoglycaemia (lows), whether this be a dose adjustment for injections or setting changes on insulin pumps.
The Diabetes Allied Health Team understands that making changes to insulin doses can be daunting to begin with, but with support and guidance from the team we aim to build your confidence in making independent changes at home.
See > Management of T1D > Dose adjustment
How do I give the insulin injections?
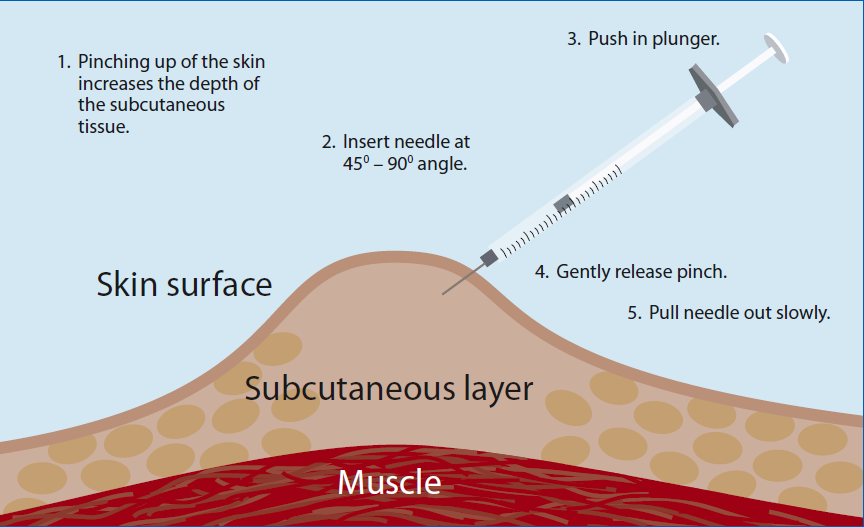
Insulin is injected into the subcutaneous layer (fat layer) just underneath the skin. This is done by pinching up the skin and injecting the syringe or pen on an angle. For pen insulin this should be a 90 degree angle and for syringes a 45 degree angle.
Where do I give my injections?
Insulin injection site rotation is extremely important in good diabetes management. It will help prevent lumps from forming under the skin and ensure good insulin absorption. If insulin is injected into the same spot repeatedly, fatty lumps will form. This is called Lipohypertrophy (or lipo).
Lipos don’t absorb insulin in the same way as healthy tissue and can lead to increased insulin doses and more glycaemic variation.
98% of people who have lipo, don’t rotate correctly!
People with lipo use on average 15 units more of insulin than people without lipo!
Sites that can be used for insulin injections include stomach, hips, arms and legs.
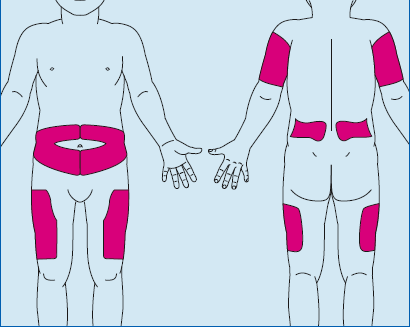
If your child has little or no fat tissue in the stomach area please do not use.
Exercise increases insulin absorption so the arms and legs may need to be avoided on days when young people are very active with sport.
If you are unsure where you should inject your child or if they have any changes to their skin, please contact your diabetes educator.
How do I care for my insulin?
Unopened insulin needs to be stored in the fridge.
Open insulin needs to be stored in a dry cool place and can be used for up to a month after opening.
Insulin can lose its effectiveness and should be discarded if exposed to direct sunlight, heat, frozen or shaken.
Dose Adjustment
Throughout life your insulin requirements will change and doses need to be adjusted accordingly in order to keep BGLs in target. Growth, sport, activity, lifestyle and food all play a part in affecting blood glucose levels.
To maintain diabetes control it is important to adjust insulin doses when BGL’s start to drift outside the target range.
Your target BGL is 4.0 mmol/L - 7.0mmol/L before main meals
Some tips
- Do not adjust insulin because of a single high or low BGL
- Look for patterns in your BGL over a minimum of 3 days
- A BGL out of target range 3 days in a row or 4 times in one week at the same time of day is a good indicator that the insulin doses should change.
- Wait 3 days to assess the effect before making a second change
BD Insulin Regimen (2 injections/day)
Hyperglycaemia (high blood glucose) at:
- Breakfast or over night - Increase your dinner dose of Protaphane/Levemir by 1-2 units
- Lunch or morning tea - Increase your breakfast dose of Actrapid/Novorapid by 1-2 units
- Dinner or afternoon tea - Increase your breakfast dose of Protaphane/Levemir by 1-2 units
- After dinner or before bed - Increase your dinner dose of Actrapid/Novorapid by 1-2 units
Hypoglycaemia (low blood glucose) at:
- Breakfast or over night - Decrease your dinner dose of Protaphane/Levemir by 1-2 units
- Lunch or morning tea - Decrease your breakfast dose of Actrapid/Novorapid by 1-2 units
- Dinner or afternoon tea - Decrease your breakfast dose Protaphane/Levemir by 1-2 units
- After dinner or before bed - Decrease your dinner dose of Actrapid/Novorapid by 1-2 units
Basal Bolus Regimen (4 injections/day)
Hyperglycaemia (high blood glucose) at:
- Breakfast or over night - Increase your Lantus/ Levemir by 1-2 units
- Lunch or morning tea - Increase your breakfast dose of Novorapid / Humalog by 1-2 units
- Dinner or afternoon tea - Increase your lunch dose of Novorapid / Humalog by 1-2 units
- After dinner or before bed - Increase your dinner dose of Novorapid / Humalog by 1-2 units
Hypoglycaemia (low blood glucose) at:
- Breakfast or over night - Decrease your Lantus/ Levemir by 1-2 units
- Lunch or morning tea - Decrease your breakfast dose of Novorapid / Humalog by 1-2 units
- Dinner or afternoon tea - Decrease your lunch dose of Novorapid / Humalog by 1-2 units
- After dinner or before bed - Decrease your dinner dose of Novorapid / Humalog by 1-2 units
This advice does not apply if your child is on sick day management
Diabetes nurse educators
9345 6661 8.30am – 4pm for non-urgent advice (routine dose adjustment)
9345 5522 out of hours for all urgent/sick day advice
CSII dose adjustment
Printable version
Your goal is to be able to make rate and ratio adjustments independently.
Throughout life insulin requirements will change. Growth, sport, activity, lifestyle and food all play a part in affecting blood glucose levels. To achieve a target HbA1c (measure of complications risk) it is important to change pump settings when BGL’s start to drift outside the target range. If you have tried making changes but are still having problems you can call or email the diabetes nurse educators during office hours for advice.
Your BGL target is 4.0 mmol/L- 7.0mmol/L. before main meals
Your HbA1c target is
< 58 mmol/mol (<7%)
Some guides
- Do not adjust settings because of a single high or low BGL Look on the download for patterns in your BGL over a minimum of 3 days (except on sick days)
- BGLs out of target range 3 days in a row or 4 times in one week at the same time of day is a good indicator that a change could be made.
- Wait 3 days to assess the effect before making a second change
- Try not to have more than 5 basal rates
- Try not to have more than 3 Insulin to Carbohydrate Ratios (ICR) or Insulin Sensitivity Factor ratios (ISF).
Hyperglycaemia
Is it basal rate or bolus ratio?
- If BGLs elevated overnight or more than 4 hours after food it is likely to be a basal rate. Consider increasing the basal rate by 0.1 - 0.2 units/hr 2 hours before the rise. If your child is under 4yrs old then only increase by 0.05-0.1 units/hr
- If BGLs high 2- 3 hours after a meal bolus it is likely to be the insulin to carbohydrate ratio (ICR). Consider lowering the carbohydrate ratio by 5%-10%.
- If BGLs high 2-3 hrs after correction it is likely to be the sensitivity factor. Consider lowering the ISF by 5%-10%.
Hypoglycaemia
Is it basal rate or bolus ratio?
- If BGLs low overnight or more than 4 hours after food it is likely to be a basal rate. Consider decreasing the basal rate by 0.1-0.2 unit/hr 2 hours before the lows . If your child is under 4yrs old then only decrease by 0.05-0.1 units/hr
- If BGLs low 2- 3 hours after a meal bolus it is likely to be the insulin to carbohydrate ratio (ICR). Consider raising the carbohydrate ratio by 5%-10%.
- If BGLs low 2-3 hrs after correction it is likely to be the sensitivity factor. Consider raising the ISF by 5%-10%.
Refer to initial pump education documents for more detailed information.
This advice does not apply if your child is on sick day management
Diabetes nurse educators
9345 6661 8.30am – 4pm for non-urgent advice (routine dose adjustment)
9345 5522 out of hours for all urgent/sick day advice
Printable version
Sick days
Children with well controlled diabetes have no greater risk of contracting infections than anybody else. Having diabetes introduces the need for closer monitoring during sick days. Good management during illness can prevent diabetic ketoacidosis and hospital admissions
Sick day management falls into two different categories:
- Illness causing hyperglycaemia
- Illness causing hypoglycaemia
Both situations will require the child to stay home from school with adult supervision.
Regardless of the situation NEVER stop insulin even if you are unable to eat.
- Insulin doses may need to be changed
- Monitoring of glucose and ketones will increase
For illness causing high BGL’s:
Viral and bacterial infections can cause stress hormones to raise BGL’s and cause insulin resistance.
- Insulin doses may need to be increased
- Check BGL’s every 2 hours
- Check blood ketones every 4 hours.
- Visit GP to treat underlying illness and or infection
- Give medicine to relieve discomfort e.g. headaches or sore throat.
- Encourage sugar free fluids to maintain hydration.
For illness causing low BGL’s:
Vomiting, diarrhoea, nausea and decreased appetite can all lead to hypoglycaemia.
- Insulin doses may need to be decreased
- Insulin can never be stopped but doses can be reduced to minimise the risk of hypo with decreased appetite.
- Check BGL’s every hour
- Check blood ketones every 4 hours.
- Ketones can be produced during illness even with normal or low BGL's
- Sip on sugar containing fluids
- Aim for ½ cup per hour of lemonade or juice
- Mini doses of glucagon may be used to treat hypoglycaemia when unable to tolerate food or fluids
Call the hospital for advice when:
- Unsure about insulin dose adjustment
- Child is drowsy or lethargic
- Child has 3 vomits, 3 diarrhoeas or abdominal pain
- Blood ketones at 1.0 mmol/L or more
Minidose Glucagon Guideline
If you have not used this protocol please call the RCH for advice.
This is used for:
- Children who are hypoglycaemic (BGL
< 4.0 mmol/LO) with inter current illness (vomiting) and cannot tolerate food or fluids (food refusal or feeling sick)
How to use:
- Inject all the water into the glucagon vial and remove the needle.
- Discard needle into the sharps container
- Use an insulin syringe to draw up and administer the glucagon solution
- Use the following table for a dose
| Age (years) |
units on an insulin syringe |
|
< 2 |
2 |
| 2-15 |
1 per year of age |
| >15 |
15 |
- When drawing up the Glucagon, remove all the air bubbles from the syringe and administer as you would an insulin injection
- BGL rechecked in 30 min. If BGL
< 5.5 mmol/L but unable to drink fluids, give double the dose of glucagon previously given, e.g. if 2 units given then give 4 units.
- Re check the BGL in another 30 min.
- Glucagon rescue can be given a 3rd time if the BGL remains below 5.5mmol/L. 3rd dose is the same amount as the 2nd dose.
- Continue to offer child small amounts of fluid and food, refer to sick day management in manual.
- BGL hourly if maintained BGL > 5.5mmol/L
- After glucagon has been reconstituted keep in refrigerator for 24 hours then discard (replace supply immediately with script from your GP)
Please call the RCH if:
Diet
The diet used in the treatment of diabetes is a healthy, well-balanced diet, that allows all the necessary foods to meet your nutritional requirements. Young people with diabetes do not need to follow a special diet or use any special foods or products. The healthy food pyramid can be used as a
good guide for healthy food choices (see pyramid below).
It is important to eat three regular meals throughout the day i.e. breakfast, lunch and dinner. Snacks are optional for children on multiple daily injections (MDI) and pumps, but may be necessary for children on twice daily insulin (i.e. Novorapid and Levemir, OR Novomix, injected at
breakfast and dinner). If children on MDI or pumps choose to eat snacks, they should be small (
<8g carbohydrates for young children, or <15g for older children). Children on pumps should bolus insulin for their snacks. All meals and snacks should include some carbohydrates, because children require
carbohydrate foods for growth and energy. Foods containing carbohydrate include bread, breakfast cereals, potato, rice, pasta, crackers, fruit, milk and yoghurt.
A good understanding of carbohydrates is essential for families of children with diabetes. Regular contact with Dietitian experienced in Diabetes care is highly recommended for children with diabetes. Your Dietitian can help with all aspects of nutrition and food including issues with
food patterns and carbohydrate spread, growth and development, appetite, physical activity, or just further education and advice on food and diabetes.

Carbohydrate counting
People living with diabetes should have a good knowledge of how to count or measure the carbohydrates in the foods they eat, regardless of what type of insulin regimen they are on. This is because the amount of carbohydrates you eat will have a direct impact on the amount of insulin you
need to inject or deliver. Carbohydrates can be counted using several different methods, none being more superior to the rest. For example, many people count carbs in ‘serves’: one serve being about 15 grams of carbohydrate (e.g. 1 slice of bread, 1 medium piece of fruit, 250mL plain milk etc). People using insulin
pumps tends to count carbs in grams. Your dietitian can help you with your carb counting skills.
Low GI and diabetes
It is important to try and include at least one low-glycaemic index (low GI) food at every meal and snack. Low GI foods let the blood sugars rise more slowly and steadily and are more sustaining than foods with a higher GI. Check out the low GI food checklist below. Sugar and foods
containing added sugars can be included in moderation in a healthy low-GI based diet without upsetting diabetes control.
Does that mean I
should only eat low GI foods?
No. There are some foods that have a high glycaemic index value that provide other important nutrients (vitamins and minerals) and are found in the base of the healthy food pyramid (the "eat most" section). These foods (e.g. watermelon and other tropical fruits) should not be
excluded and can be eaten in conjunction with other low glycaemic index foods. Combining low and high GI foods together results in a moderate GI effect.
There are also many foods that have a low glycaemic index but are high in fat or have poor nutritional value and are therefore found in the top section of the healthy food pyramid (the "eat least" section). These foods are not recommended to be eaten on a regular basis.
So remember, glycaemic index value alone does not determine the suitability of a food - the guidelines of a healthy diet (as illustrated by the healthy food pyramid) are the most important considerations. Stick to the guidelines of the healthy food pyramid and select low glycaemic index food
choices where practical.
For up to date information on glycaemic index go to
https://www.glycemicindex.com/
Making the changes from high GI to low GI choices
| High GI food |
Low GI alternative |
| Bread (white or wholemeal) |
Bread containing lots of 'grainy bits' such as Burgen™, Helga's™ Soy and Linseed, Multigrain, pita bread or sourdough breads |
| Processed breakfast cereals |
Unrefined cereal such as rolled oats, muesli or a low GI processed cereal such as Guardian™, Special K™, or All Bran™
|
| Plain biscuits and crackers |
Biscuits made with dried fruit and whole grains such as oats |
| Cakes and muffins |
Make them with fruit, oats and wholegrains |
| Tropical fruits e.g. watermelon, ripe bananas |
Temperate fruits e.g. Apples, stone fruit and citrus fruit
|
| Potato |
Sweet potatoes, corn, pasta and legumes |
| Most rices |
Basmati rice, Doongara rice (Clever rice) or Mahatma brand long grain rice |
Useful apps
Some apps that might be useful when on the go and trying to count/ estimate carbohydrate content of mixed meals include;
Calorie King
This app generates a nutrition panel similar to that seen on product packaging. The beauty of the app is the ability to manipulate the portion size consumed while the app calculates the amount of each nutrient (carbohydrate in this case) for you! If the specific brand is unknown the app
can generate an average for all brands. If the specific brand is known, you can scroll down the list to find it for more accurate information. Available on both Apple & Android.
.png)
Carb & Cals: Diet and Diabetes
This app is great for people who like a visual reference for their portion sizes. You choose a food and then get to look at different serving sizes labelled with how many carbs are in each. Available on both Apple & Android.
Easy Diet Diary
This app is useful for a number of its functions, most relevant to diabetes is the ability to input your own recipes to assist with carbohydrate counting. Once the recipe ingredients and quantities have been entered, along with the number of serves produced by the recipe, the app
automatically generates a nutrition panel similar to those seen in apps mentioned above. Only available on Apple.


The diabetes social work service is available to support children and families in dealing with the impact of diabetes on their lives. The support is available while the child is a patient at RCH, from diagnosis through to the time when a young person transitions to adult services.
Social workers provide a range of support and assistance that may be needed when a child is admitted into hospital or managing a chronic condition as an outpatient.
This is done through:
- Counselling
- Supporting families through times of crisis and distress
- Providing education and information
- Advocacy
- Assisting patients and families during periods of hospitalisation
- Planning for discharge from hospital
- Referral to community agencies and supports
- Liaising with interstate, regional and other metropolitan hospitals
- Delivering group and support programs
- Facilitating access to the hospital
- Accessing practical and material assistance
Initial diagnosis
When your child is diagnosed with type 1 diabetes it affects the whole family as this is a period of adjustment. There is significant grief and loss around the diagnosis and this takes time to process. While your child is an inpatient at the RCH you may feel tired and overwhelmed processing all the information you are given to support your child at home. The Diabetes Allied Health Team are here to support you during this stressful adjustment period.
A new diagnosis of diabetes may create difficult emotional issues for young people. Children look to their parents for support and cues about how to manage their own reactive emotions. This can be difficult for parents as they are also struggling with their own feelings and it is important that parents get support from family members, friends, support groups and the Diabetes Allied Health Team.
Each child is individual and may experience different emotional responses at different times: Some examples can be:
- Difficulty coping with the emotional reaction of family members
- Anxiety about the condition.
- Fear of needles and multiple injections.
- Frustration over the daily tasks of managing diabetes.
- Embarrassment about their diabetes and their friends' possible negative reactions.
- Difficulty coping with the emotional reaction of family members.
- Worry about school.
It is important that once children and young people go home from hospital they return to school/kinder, sports, afterschool care, having playdates etc. as soon as possible. Returning to familiar activities that were enjoyed before the diagnosis brings a sense of relief to children and young people and highlights that they are ‘well’. It can also distract them from being excessively preoccupied with thoughts and feelings about their condition. It allows them to access informal support through friends and family which will be highly beneficial at this time.
Tips for helping your child
- Be honest with the child or young person.
- Be patient.
- Create a space that is calm at home and at school to carry out tasks.
- Be prepared.
- Allow the child or young person time to talk.
- Encourage them to write down any thoughts, questions he/she is having in a note book and these can be discussed with doctor, Diabetes Allied Health or family.
- Use age appropriate distraction eg. Bubbles, TV, IPAD, song, game.
- Try big deep breaths to relax during the injection/finger prick.
- Reward charts can be helpful for younger children
Siblings
Siblings often worry a lot and should be spoken to about the diagnosis of diabetes and what the treatment entails in basic age-appropriate language, so they are prepared and understand as much as possible.
Siblings of children with diabetes often feel that they get less attention, care and support than their sibling with diabetes. Where possible try and find time to spend with siblings away from ‘diabetes’!! Young children may like to help so give them a task e.g. “can you get a tissue for your sister?” or “can you get the iPad for them?”
Juno Health is an initiative set up by doctors to explain medical information to children and have developed a comic book discussing what type 1 diabetes is to siblings.
Click here to be taken to this resource.
Parental support
Parents go through a wide range of emotions when their children have a chronic condition and these feelings often come in waves, e.g. denial, anger, frustration, sadness, guilt, fear and depressed mood. How parents learn to cope with their own emotions and their own needs will determine how they can best support their child. To care for your child you must first care for yourself!
Some self-care tips
- Continue to do things that you loved prior to diabetes diagnosis.
- Educate others in your family about diabetes management so you can have a break!
- Talk to family and friends regularly.
- Adult colouring, yoga, deep breathing, gym, music, reading etc can assist parental wellbeing
Diabetes and parenting
As if parenting wasn’t hard enough! When your child has diabetes parenting can be even more difficult and require more planning, routine and involvement in your child’s life. Children and young people can often rebel against this and it is important to have all carers on the same page to support the child and for them to feel safe. Parental anxiety is often transferred to the young person so it is important that you have a space to talk away from your child as not every conversation is developmentally appropriate for a child to hear.
Your child is still the young person they were before their diagnosis and can achieve goals, play sports, get a job etc. It is important that there are times at home and while out and about that there is no (or limited) ‘Diabetes talk’. Diabetes does not define who they are and this is important to remember. For instance, it is not helpful to say to your child when they first arrive home from school “what is your BGL?”A better question might be ‘how was your day at school?”
Support for young people
Sometimes it is helpful to talk to other people who understand what it is like to live with diabetes or be a parent of a child with type 1 diabetes. Group support often makes people feel less isolated and alone.
Diabetes Camp
Read information about Diabetes Camp.
See the section on camp on the type 1 diabetes page for more information.
Other online support for young people
eHeadspace provides free online and telephone support and counselling to young people 12 – 25 and their families and friends.
MindShift (App)
Free app designed to help adolescences and young adults cope with anxiety and shift their thinking. Offers a range of strategies to manage excessive worries, stress, anxiety and panic. Also offers mindfulness and relaxation techniques.
SmilingMind (App)
Free app that offers mindfulness and meditation exercises for young people 7 years and older. Australian designed app to help de-stress and stay calm, a range of different programs for different age groups.
Free app that offers meditation exercises to help people de-stress and switch off from current stressors and anxieties. There is also a Headspace for Kids app, that is more appropriate for young people under 12 years of age.
Juvenile Diabetes Research Foundation (JDRF)
JDRF has developed a support program that
provides practical advice and help for people who have been affected by a diagnosis of type 1 diabetes.
Diabetes Victoria
Diabetes Victoria has
information for people affected by type 1 diabetes.
Chronic illness peer support program at The Royal Children’s Hospital (ChIPS)
This program is run for young people age from 12-25. The focus is to connect with other young people who get what it’s like to live with a chronic illness.
Please see the website for further information and if you would like to be part of this program please talk to the diabetes allied health team.
Other useful websites
http://www.diabeteskidsandteens.com.au - It has learn and play games and additional child and teenage friendly ways of discussing type 1.
http://www.diabetes.co.uk/
Famous people living with diabetes
Joe Eldridge, Professional Cyclist - Member of Team Type 1 Check out
Team Novo Nordisk for some inspiration and tips about diabetes and sports. Team Novo Nordisk is a global all-diabetes sports team of cyclists, triathletes and runners, spearheaded by the world’s first all-diabetes professional cycling team. The team’s mission is to inspire, educate and empower people affected by diabetes
Dale Weightman, AFL Player – Dale runs yearly presentations at the Richmond football in June each year.
Ben Cocker- Soccer player.
Jeremy Irvine, Actor- starred in War Horse movie.
Sonia Sotomayor- Supreme court judge.
Jack Fitzpatrick- AFL player.
Sam Reid- AFL Player.
Brandon Jack- AFL Player.
Paddy McCartin- AFL Player.
Centrelink
Carers Allowance and Health Care Card for people under 16 years of age.
The Carers Allowance is an additional benefit to the Health Care Card provided by the Commonwealth Government. A submission may be made to obtain the Carers Allowance from Centrelink. It is means tested and families who meet residency requirements are eligible if the family household income in lesser
then $250, 000. It is only available for children up to age 16 year of age.
Applications for the Carers Allowance are made through Centrelink. Eligibility for the Carers Allowance is determined on criteria based on the medical report that can be signed by the Treating Doctor, Credentialed Diabetes Nurse Educator or your local GP.
To apply for the carers allowance
- Please call Centrelink on 13 27 17 and request an application for carers allowance and a health care card. These forms are not available online.
- Centrelink will then post out the appropriate forms including a medical form.
- Please sign the front of the medical form before sending this into you Diabetes Nurse Educator or giving it to your doctor.
Please send forms to :
[Your diabetes nurse educator]
Department of Endocrinology and Diabetes
The Royal Children’s Hospital
Level 5
50 Flemington Road
Parkville, 3052
Once completed it can be returned to you to submit with all the forms or if all forms are sent in we can submit it on your behalf to Centrelink. The process to claim takes about 4-6 weeks.
Centrelink reviews all payments when your child turns 16 years old. Carers allowance is ceased at this point. If you are a previous recipient of carers allowance and cared for child with type 1 diabetes before they turned 16 years of age you will be eligible to apply for a ‘health care card for
former recipient of carers allowance health care card’. Centrelink will sometimes advise you that you need to complete documentation, otherwise you will need to contact Centrelink regarding applying for ‘health care card for former recipient of carers allowance health care card.’
Further
information about the Health Care Card can be obtained from any Centrelink
office, by accessing www.centrelink.gov.au or
by calling 13 27 17.
Identification
It is beneficial for the young person to wear some form of identification that says they have diabetes, like a necklace, bracelet or diabetes ID card.
www.medicalert.org.au
Young people also can put medical details in the health app on their phone and paramedics can access these details without a pin number. This is important just in case someone doesn't know they have diabetes and they have a hypo or get sick.
Parking
If you have a Health Care Card (HCC), this entitles you to discount parking. Present your HCC to security on lower ground near emergency department before returning to your car.
Victorian Patient Transport Assistance (VPTAS)
If you live more than 100 Km away from the hospital, you may be eligible for travel and accommodation assistance from the
VPTAS
Sport and activity
Keeping active is an important part of your diabetes management. Having diabetes shouldn’t stop you from performing sports at your best! National guidelines encourage children to participate in physical activity for at least 60 minutes on most days of the week. This can be smaller sessions added together e.g. 30mins of walking plus a 30min tennis lesson.
Limiting your time in front of a screen (e.g. TV, computer, iPad, mobile) to less than two hours a day and walking to school are easy ways to increase your daily activity levels.
Regular activity can help you to:
- Feel good
- Have a healthy heart
- Give you more energy
- Keep your body in good shape
- Improve the action of insulin
Exercise can affect blood glucose levels and insulin requirements. Everyone is individual and the response to exercise can vary from person to person.
How does exercise affect blood glucose levels?
In general, exercise lowers your blood glucose levels (BGLs). This is because your body uses glucose as an energy fuel. Sometimes BGLs can rise just before or during an activity due to the release of a hormone called adrenaline. This is usually short lived, with BGLs returning to target range without requiring extra insulin. If your BGLs are above 15mmol/L and you have ketones then activity should be postponed. Exercising when your BGLs are this high could further raise your levels and increase your ketone production.
Management of your diabetes during exercise will depend on the type, duration and intensity of exercise.
To get a better understanding of your blood glucose response during exercise, it is important to keep a record of your blood glucose levels and types of exercise performed. This includes testing before, during and after exercise. It is important to aim for target blood glucose levels (4-8 mmol/L) to maximise performance during exercise. Hyperglycaemia before exercise can impact on your performance during exercise.
Recommendations
Additional carbohydrate “activity food” should be used for sport/exercise.
Insulin doses may also need to be adjusted because of increased insulin sensitivity from the muscles used during exercise. Your diabetes nurse educator and dietitian will help you work out carbohydrate intake and/or insulin dose adjustment when planning exercise.
Injecting in the lower tummy/abdomen or hips is preferable prior to exercise.
A general guide for managing exercise
As a general rule for every 30-45mins of moderate to intensive physical activity you need to consume one extra serve of carbohydrate (approximately 15-20grams), preferably low GI. This is just a starting point, the amount of carbohydrate you require may differ depending on your level of fitness and the type/length of activity you are doing.
Examples of 1 carb serve activity snacks;
- 1 piece of fruit
- 200g tub of yoghurt
- Glass of milk
- 2 plain sweet biscuits
- 1 slice of bread with spread
- 4-6 crackers
- 125mls of Juice
- 1 Muesli bar
It is usually best to have the extra carbohydrate 30mins before exercising. This is in addition to the carbohydrate you usually have.
You do not need extra carbohydrate during recess and lunch breaks at school (even if you are very active). Your daily insulin doses and carbohydrate serves are based on your usual activity levels.
If you are doing long periods of high intensity activity then you might need to have extra fast acting (high GI) carbohydrate during the activity e.g. sports drink or juice. Your diabetes team can advise you on this.
When swimming, have one extra serve of ‘fast acting’ carbohydrate just before starting (e.g. 5 jelly beans or 125ml glass of lemonade or juice) and for every 30mins you are in the water. This is to ensure BGLs stay above 4mmol/L as hypoglycaemia can be harder to detect in the water.
Delayed hypoglycaemia
Delayed hypo’s can occur, often up to 12-16hours after being active. This is because your muscles continue to use glucose during recovery and your body is more sensitive to insulin after exercise.
Testing BGL’s prior to bed and overnight is necessary after prolonged exercise. If you are experiencing regular hypoglycaemia during or after activity then a reduction in insulin might be necessary.
Importance of monitoring!
Exercise affects everyone differently. Monitor your BGLs carefully to look for patterns and learn how your body responds to different sports. Testing your BGLs before activity is important and can give you an idea as to which direction your BGLs are heading and how much extra carbohydrate you require.
Guide to extra carbohydrate before and during exercise
| Exercise |
Blood glucose level before |
Extra carbohydrate (1serve = approx 15g carbohydrate) |
| All activities |
Less than 4mmol/L |
Treat hypo and delay exercise until feeling better or BGLs >4mmol/L |
| Short duration (less than 30 minutes) or Low intensity exercise (e.g. walking, general play) |
Less than 7mmol/L, More than 7mmol/L |
1 serve before. No extra necessary |
| Moderate to High intensity exercises (e.g. basketball, netball, running) |
If BGL is less than 12mmol/L
Above 12mmol/l |
1 serve before, followed by 1 serve every 30-45 minutes of exercise
May not need a carbohydrate serve prior to exercise however may require 1 serve after 30-45 minutes during exercise to maintain normal BGL’s |
Exercise should be avoided if ketones are above 1mmol/L on injections or 0.6mmol/L on insulin pump therapy. Less carbohydrate may be needed if insulin has been reduced before the activity.
Printable version
Driving with diabetes
Before getting your learners or probationary license your Diabetes specialist will need to declare you ready to drive.
It is your responsibility to undertake certain measures prior to every trip you drive in order to ensure you are
safe before getting behind the wheel – this is for your own well being
and that of others on the road.
As with everyone with Type 1 or insulin treated diabetes, obtaining and ongoing renewal of your drivers’ license will be conditional on achieving and maintaining certain standards of self-care and wellbeing. Certification of being medically fit to drive must therefore be provided by your treating diabetes doctor at the time of your first licence application and 2-yearly thereafter. It is your responsibility to ensure that this is done in a timely manner.
Necessary requirements before obtaining license
- You must notify VicRoads that you have type 1 diabetes – they will provide you with a medical form that your doctor must complete.
Vic Roads reporting a medical condition or driver
- Notify your motor vehicle insurance company that you have Type 1 diabetes
- You must not have had a severe hypoglycaemic episode in the preceding 6 weeks
- You must show evidence to your doctor through your glucometer that you’re already regularly checking your BGL as is the requirement before and during a drive.
Necessary precautions that you must undertake before every drive
- Check blood glucose before each trip
- Do not drive if BGL is less than 5mmol
- Take your meter, hypo treatment and long acting carbohydrate with you, even on short or learner drives
- Check your blood glucose level at least every 2 hours. At the RCH we recommend hourly BGL testing. On longer trips plan regular stops for BGL testing and snacks
- If your BGL is between 4-5mmol/L, have a sustaining carbohydrate serve
- If you have a hypo while driving pull over the car and turn engine off. Do not drive until your BGL returns to 4mmol/L or above
- Do not delay or miss any main meals
- We also recommend that you wear a medic alert or similar identification bracelet or that states your name and your condition.
Non-driving period after a ‘severe hypoglycaemic event’
If a severe hypoglycaemic event occurs the person should not drive for a significant period of time and will need to be urgently assessed. The minimum period of time before returning to drive is generally six weeks because it often takes many weeks for patterns of glucose control and behaviour to be re-established and for any temporary ‘reduced awareness of hypoglycaemia’ to resolve. The non-driving period will depend on factors such as identifying the reason for the episode, the specialist’s opinion and the type of motor vehicle licence. The specialist’s recommendation for return to driving should be based on patient behaviour and objective measures of glycaemic control (documented blood glucose) over a reasonable time interval.
Reduced awareness of hypoglycaemia
Reduced awareness of hypoglycaemia exists when a person does not regularly sense the usual early warning symptoms of mild hypoglycaemia such as sweating, tremulousness, hunger, tingling around the mouth, palpitations and headache. It markedly increases the risk of a severe hypoglycaemic event occurring and is therefore a risk for road safety. A person with persistent reduced hypoglycaemia should speak with their treating endocrinologist for assessing if they are fit to drive.
This information has been adapted from Assessing Fitness to Drive, a joint publication of Austroads and the National Transport Commission (NTC), which details the medical standards for driver licensing for use by health professionals and driver licensing authorities. For more information or to download the full document please visit
Austroads
Below are links to the Vic Roads website for more information on driving with diabetes and reporting your medical condition to Vic Roads
For more information on driving with diabetes
School camps
Every child who attends school will attend a school camp at some point. A camp plan is required to provide diabetes information to the child’s care givers whilst they are on camp. Most children will also require a reduction in insulin for camp.
If the camp is more than 30 minutes from an emergency service we recommend that an adult attending knows how, and is willing, to give Glucagon. We also recommend overnight BGL testing at 2am.
We require two weeks notice to put together a camp plan. We need the following information:
- Child’s name and date of birth
- Dates of the camp
- Type of insulin regimen
- Current insulin doses
Please email
diabetes@rch.org.au with the above information
Diabetes camps
Diabetes Camp are a separate camp for children/adolescents with Type 1 Diabetes. They are coordinated by the consortium of the RCH, Monash Children’s and Diabetes Victoria. For more information please use the following link
Diabetes Victoria Camps
Travelling and holidays should not be restricted because your child has diabetes. However, you will need to make sure that you have planned ahead to ensure your time away is safe and enjoyable.
Domestic travel
- A domestic travel letter for the airlines is required – please contact
diabetes@rch.org.au to request this letter
- Take twice as many supplies as you would normally use in the same time frame
- Carry insulin, syringes/needles and other diabetes supplies (including hypo food/drink) on board with you, divided in two separate bags in case one is lost. Don’t pack any supplies in your checked in luggage in the cargo hold as they may be exposed to extreme temperatures or get lost at the airport
- Consider comprehensive travel insurance
International travel
- An international travel letter for the airlines is required – please contact
diabetes@rch.org.au to request this letter
- A timing of insulin injection plan is required when the time difference at your destination is more than 3 hours. We require 4 weeks notice to put together a flight plan and require the following information:
- Child’s name and date of birth
- Flight itinerary (including time and length of flights)
- Type of insulin
- Current insulin doses
This is a guide for creating your own flight plan if you are on multiple daily injections. Use this guide to develop your plan and you can send it to diabetes@rch.org.au for a diabetes nurse educator to review once you have completed your plan.
- For those on an insulin pump, change the pump time once you reach your destination. Carry back-up injectable insulin and consider taking either long-acting insulin or a replacement pump. Replacement pumps can be obtained by contacting your pump company, not through the RCH.
- Take twice as many supplies as you would normally use in the same time frame
- Carry insulin, syringes/needles and other diabetes supplies (including hypo food/drink) on board with you, divided in two separate bags in case one is lost. Don’t pack any supplies in your checked in luggage in the cargo hold as they may be exposed to extreme temperatures or get lost at the airport
- Consider comprehensive travel insurance
- Useful websites:
Diabetes Australia travel advice
International Association for medical assistance to travellers
International society of travel medicine
Medicare (Australians overseas)
National Diabetes Services Scheme travel fact sheet and checklist
Smart Traveller(Department of Foreign Affairs and Trade)
-
Abbott Diabetes Care Travel Guide
Flying with an Insulin Pump
- Date/Time in pump: Keep your pump on local time until you reach your final destination. When you arrive, change the pump time to match local time.
- Pump settings and reports: Ensure you have a current download report from either system i.e Medtronic Carelink Settings report (page 5) or Diasend Settings report (under Insulin tab). If using a Medtronic 640/670G and sensing, it will need to be put into ‘flight mode’.
- Check for air bubbles in pump line when ascending and descending during the flight. If there are air bubbles disconnect and prime them out before reconnecting. Alternatively, you can disconnect and suspend the pump while the plane is ascending and descending, and check the
- Pump Failure: In the event of pump failure, you will need revert to injected insulin.
Inject Novorapid / Humalog via pen or syringe every 4 hours until you can resite or reconnect the pump.
Give Total Daily Dose (TDD) divided by 6 (TDD÷6) every 4 hours + 2-3 serves of carbs.
If you need further clinical advice please refer to the Sick Day Management section of this website
Contact your pump company regarding a replacement pump. - Line/site failure with blood ketones: Hyperglycaemia, blood glucose levels persisting ≥15.0mmol/L despite 2 corrections or blood ketones ≥ 0.6 mmol/L requires pen insulin and a cannula resite.
Inject TDD ÷ 6 as Novorapid / Humalog via pen/syringe, and resite.
Until you cann resite the pump you will have to continue to give these injections every 4 hours - Pump Supplies: Take your usual blood glucose and ketone testing strips and equipment, hypo food and pump supplies. Other equipment will include extra Novorapid / Humalog in case of pump failure. Medical equipment and supplies are taken as carry-on luggage, as you may require during in flight. Take double the amount
Please call the RCH Diabetes Service (urgent only):0061 3 9345 5522 if you need further advice
Insulin pump flight tips
Printable version
What is insulin pump therapy?
An insulin pump is a small computerised device powered by batteries. It delivers rapid-acting insulin continuously in small amounts into the subcutaneous tissue. The pump is about the size of a deck of cards and is worn by clipping it onto a piece of clothing or worn in a pocket. Insulin is delivered through a thin plastic tubing attached to a syringe in the pump. At the end of the tubing there is a small needle which is used to insert the infusion set under the skin into the fatty tissue and is secured by a waterproof dressing. The needle is then removed leaving a small, hollow, flexible plastic tube, called a cannula. These infusion sets are changed every 2-3 days. The pump can be removed for up to 1.5 hours, to enable you to have a shower, go swimming or participate in contact sport. Insulin pumps are not automatic and not an ‘artificial pancreas’. It must be interacted with to give insulin when needed. Blood glucose levels must be checked 6-8 times a day for pump therapy to be safe and effective. The pump does not monitor blood glucose levels! You can purchase continuous glucose monitoring (CGM) separately to work with your insulin pump.
How does pump therapy work?
An insulin pump tries to replicate what normally happens in the body. It can deliver insulin in exact amounts as small as 0.025units per hour. Insulin is delivered in two ways:
Basal: insulin that is delivered continuously 24 hours a day in the background. The job of the basal insulin is to keep blood glucose levels stable when you aren’t eating food. Basal rates can be programmed to change over the day based on individual needs.
Bolus: Insulin needs to be given in a larger amount when you are eating or when your BGL is above target. These boluses cannot be pre-programmed into the pump. A pre-meal bolus is given based on the amount of carbohydrates about to be consumed. A correction bolus is given when blood glucose levels are above target to try and bring them back down. The pump is able to calculate the amount of insulin required based on BGL and/or carbohydrate grams being entered by the user. It cannot work independently. It requires the user to enter BGLs and amount of carbohydrate to be consumed.
All rates and ratios are set by the diabetes team at the commencement of pump therapy based on individual needs. With assistance, families are then taught to adjust their own pump settings when required.
What are the advantages to pump therapy?
- Insulin delivery is precise and calculated according to each person’s individual needs. Because of the accuracy of insulin administration, it may be possible to keep blood glucose levels in target range, most of the time.
- There is a greater flexibility in timing and the type of meals and snacks that can be eaten
- With accurate settings, quality of life can be improved with greater flexibility in being able to accommodate unpredictable events/activity
- Allows for more frequent adjustments in insulin dose, enabling a rapid response to changing BGL
- Diminishes variable absorption rates that occurs with long acting insulin
- May reduce incidence of hypoglycaemia during the night, post exercise and severe recurrent hypoglycaemia
- When used properly, pump therapy can be responsible for better diabetes control
What are the disadvantages to pump therapy?
- There is a higher risk for DKA as the pump only uses rapid acting insulin. If there is an interruption to insulin delivery, blood sugars will immediately begin to rise and ketones will start developing within a few hours without insulin. Rapid acting insulin pens must be available at all times to inject insulin if required and ketones must be checked if BGLs are higher than 15mmol.
- Potential for skin infection and irritation around the insertion site is much higher. Infusion sets must be changed every 2-3 days and site rotation is just as important and when you are injecting.
- Intensive BGL testing is required. Pump users need to do 6-8 BGLs per day to ensure basal and bolus doses are accurate
- The device needs to be attached all the time with only certain exceptions for showers, swimming and contact sport.
- Learning how to manage pump therapy successfully can be a steep learning curve. Commencing on a pump requires several education sessions and is a lengthy process to learn all the features to the pump.
Who would be considered for pump therapy?
Pump therapy is not for everyone. Discuss your options with your Endocrinologist at your next appointment and clarify with them if insulin pump therapy is suitable for you.
The following need to be considered before commencing on a pump:
- The young person needs to be able to show evidence of more than 4 BGLs per day
- Ability to self adjust insulin appropriately
- Ability to self administer injections
- No injection bother
- Family members must be supportive and motivated to help with management, and must be included in the all education sessions
- The young person needs to be motivated to improve control and maintain it
- An interest in learning about carbohydrate counting
What are the financial cost involved?
The pump devices are approx $9,025. Private health insurance should cover this cost and should be confirmed with your health fund before considering insulin pump therapy. Confirmation in writing is preferred.
For the private health insurance company to cover the cost of an insulin pump, the membership is required for a minimum of 1 year.
The other costs involved in pump therapy are the consumables; the line, cannula and insulin reservoir/cartridge. Most consumables are covered by NDSS. The costs of consumables are approximately $30-40 per month.
Insulin pumps supported at the Royal Children's Hospital:
In order to have a thorough knowledge and expertise of the devices, at RCH we have limited the pumps we support to the following:
Medtronic 640G and 670G
AMSL Tandem t:slim
For more information refer to the
Medtronic and
AMSL Diabetes web sites.


We would like our child to commence on pump therapy, what is the next step?
The first step is to speak with your Endocrinologist at your next appointment. If you meet the criteria for pump therapy, your doctor will write you a referral to the Diabetes Allied Health team for a pump information session. This appointment will take place with a diabetes nurse educator and one other family.
If you decide that pump therapy will suit your family you will be allocated a series of appointments for your ‘pump start’. The current waitlist from the time of your information session is 6-9 months. The appointments following your information session include:
- Choosing your pump (approx. 3hrs)
- Receiving your pump and learning how it works (approx. 3hrs)
- Pump start (two full days)
- Pump start review (approx. 2hrs)
- Pump start follow up (6 weeks from pump start)
These clinics are run on set days and may be with one or two other families
We are interested in pump therapy for my child however we can't afford private health insurance. Is there another option?
JDRF provide funding for families who meet certain criteria. For further information visit the
JDRF website.
My child's diabetes specialist have referred us for 'consideration for insulin pump therapy' and we have been offered an appointment for a 'pump information' session. What do we need to do before attending this session?
- Confirm your attendance to the appointment via phone or email
- Whilst we are reducing face to face encounters with COVID-19 these appointments will be via Telehealth. Ensure the appropriate platform has been set up on your home computer and you have access to the invitation details
- Watch the videos on how to insert a pump infusion set:
AMSL Tandem t:slim
Medtronic Sure T infusion Set - How to Guide
This information can also be found on your appointment letter.
Where should I direct any additional questions?
If you have any further questions please speak with your Endocrinologist at your next appointment or contact the Diabetes office on 9345 6661
Printable version
Continuous Glucose Monitoring (CGM) and Flash Glucose Monitoring (FGM)
There are currently two CGM systems available in Australia- the Medtronic and the Dexcom.
The FreeStyle Libre system is not a continuous glucose monitor but a flash glucose monitor (FGM). This means that it will only give you a reading when you scan the sensor with a reader or smart device. FGM has some similar benefits to the CGM.
NDSS fact sheet on CGM and FGM
What is CGM?
CGM is a small button like device that sits against the skin and records subcutaneous tissue (not blood!) glucose. Tissue glucose levels and blood glucose levels are not always the same. When you use the current CGM devices under optimal conditions the CGM glucose is usually within a 10-13%
Both the Dexcom and the Medtronic systems require calibrating. This is done by fingerpricks and testing blood glucose on a meter as you have always done. The amount of times that this needs to be done can vary between 2-4 BGLs per day depending on the system that you are using.
Tissue glucose readings are taken by the CGM every 10 seconds and averaged out over 5 minutes. It is the 5 minutely average reading that is recorded and displayed
CGM sensors vary in terms of how long they last. Under ideal conditions they will last between 5-13 days depending on the brand. Some people find that electrodes can last longer than this, though the accuracy of the sensors is not guaranteed by the manufacturers once the sensor is used beyond
Tissue glucose levels that have been measured by the CGM can be seen in ‘real-time’ either on a purchased receiver, a mobile phone or on an insulin pump depending upon the specific device. Displays include the current glucose level and a graph of previous glucose levels over several hours
For more information:
Medtronic and the Dexcom CGM systems, please refer to the
Medtronic and
AMSL Diabetes (Animas) web sites.
For more information on
Abbott Freestyle Libre (FGM)
Will CGM improve my diabetes control?
The short answer is yes, no and maybe.
CGM devices have become much more accurate over recent years and they measure tissue glucose extremely well. But does this translate to better diabetes control?
Studies performed on CGMs have shown a variety of results. These range from no benefit to only a small benefit in reducing a patients HbA1c, reducing hypoglycaemia and improving quality of life. Individuals anecdotally report a variety of responses in relation to wearability, comfort
One of the reasons behind these conflicting results is because people use CGMs for a variety of situations. Some patients use CGM with injections, some use it with insulin pumps and others use it linked to the pump where it has limited control over the delivery of insulin in certain
Studies show that the amount of time the CGM is in use is critical. To gain any benefit in reducing HbA1c, CGM devices need to be used more than 70-80% of the time (i.e. > 5 days per week). Research suggests that for a variety of reasons most adolescents are unwilling to wear CGM more
The motivation of the user has shown to also significantly affect the benefits of wearing a CGM. If the aim is simply to avoid hypoglycaemia and not to improve metabolic control then HbA1c levels may worsen.
Finally, for some, CGM provides too much information. Adolescents in particular and some parents find the constant feedback from CGM overwhelming, causing them to switch off and ignore readouts and alarms, particularly if the CGM readings give false-alarms.
Research is currently underway into CGM as part of a “closed loop” systems. This will predict where a blood glucose level is heading and inform a pump ahead of time about how much insulin to deliver. Being able to change insulin delivery ahead of time rather than in real time is what most clinicians think
Which CGM devices are available on the NDSS subsidy?
Dexcom G5
Dexcom G6
Medtronic Guardian Connect or Guardian Link 3
See this
information sheet to learn more about using the Hybrid Closed Loop insulin pump that connects with the Medtronic 670G
Abbott Freestyle Libre (FGM)
How to apply for CGM or FGM
Complete the following NDSS form and email it to diabetes@rch.org.au -
Continuous and Flash Glucose Monitoring Eligibility Assessment form
Device options for CGM and FGM
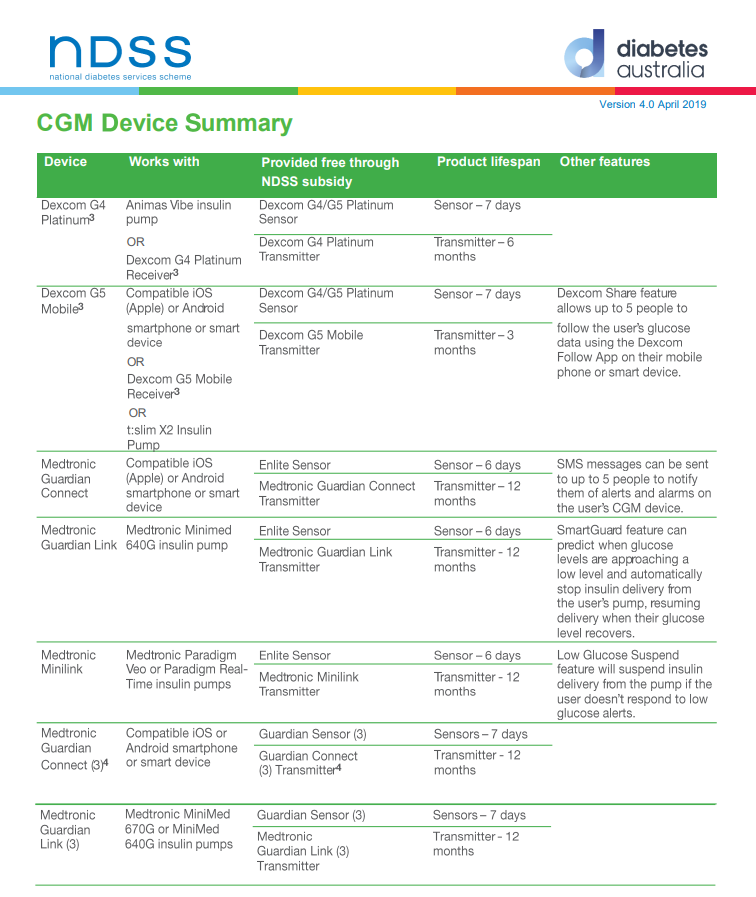
.PNG)
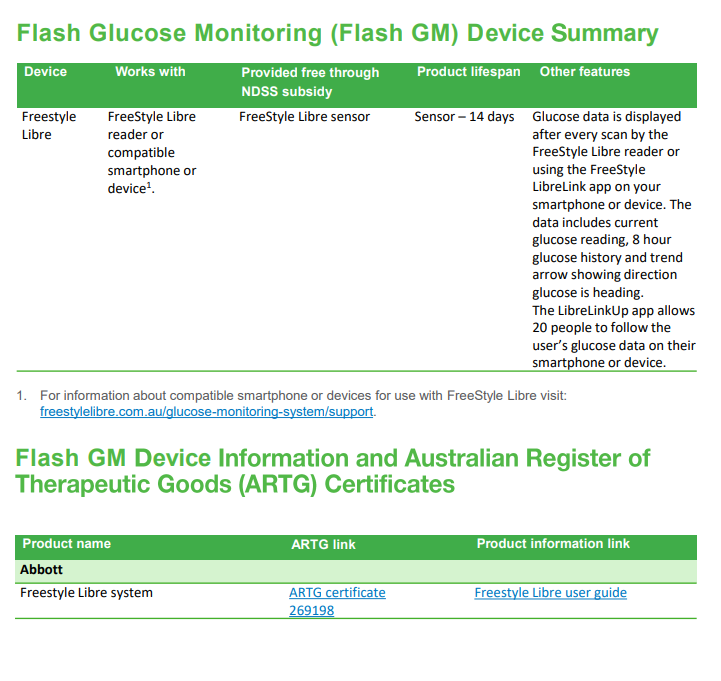
NB- YOU MUST be registered with the NDSS to access the CGM program.
Video resources
Continuous Glucose Monitoring. presented by Professor Fergus Cameron and Rebecca Gebert
Webinar recorded 10th May and was presented by Professor Fergus Cameron (Endocrinologist) and Rebecca Gebert (Diabetes Nurse Educator)
In this webinar we will introduce you to the world Continuous Blood Glucose monitoring. What is CGM? Will it improve diabetes management? Is it all it's cracked up to be?
Why Sensor Glucose (SG) and Blood Glucose (BG) wont always Match
Blood Glucose (BG) and Sensor Glucose (SG) - What is The Difference
Diabetes Complications Clinic at the Royal
Children’s Hospital
Diabetes Complication Screening is offered to children and adolescents with diabetes as a routine screening tool. Screening allows for the detection of very early signs of complications, where changes can be put in place to stop or reverse that complication.
The Diabetes Complication Screening Clinic assessments includes a photo of the back of the eye, to check for nerve damage to the eyes, blood tests to screen lipids, coeliac, thyroid and thyroxine levels and a urine test to check kidney function, a postural blood pressure and an assessment of
peripheral neuropathy.
Your doctor has to refer you child to the Diabetes Complication Screening Clinic. Usually the screening appointment will be booked in alongside your next endocrinology appointment. At times, there can be waiting list, if this is the case it will be booked in alongside your
appointment in 6 months’ time.
When should my child be getting Diabetes Complication
Screening at RCH?
If diagnosed with diabetes under the age of 10 years old first diabetes complication screening at approximately 5 years after diagnosis. And then every 2 years until 15 years old and then annually.
If diagnosed over 10 years of age, first comps screen approximately 3 years after diagnosis, every two years until 15 and then annually.
Who organises when my child needs a complication
screening?
Your Endocrinologist will refer your child to the Diabetes Complication Screening Clinic. It will be booked in alongside your next diabetes appointment, on either a Tuesday or a Wednesday afternoon.
How will I get notified of my appointment?
An appointment letter with instructions will be sent to your home address. As part of the screening, your child will need to get a sample of the first urine of the day. The reason for this is that an early morning sample gives a much more accurate result than one done during the day. If you
forget to do the morning sample a midday sample can still be used. You can collect a yellow collection container from your local pharmacy or pathology. You can keep it in the fridge at home until the appointment.
What happens when my child gets their Diabetes
Complication Screening?
Your blood tests will be ordered and waiting for you at pathology (A6) where you usually get your HbA1c. Please do not use a kiosk to check in. Remember to tell the check in personal that your child is having a Complication Screening which requires a blood test.
What tests are done as part of the Diabetes Complication
Screening?
· Urine test to check the amount of protein being passed via the kidneys into the urine
· Blood test to check blood lipids, thyroid function and coeliac antibodies
· Blood pressure both lying and standing
· Vision testing including retinal photo and a visual acuity assessment
· Nerve testing of the foot
My child has been asked to do 3 early morning urine
samples- what does this mean?
It is very common to have mildly increased levels in your urine if the test is done from a midday sample. If this happens we need to check the levels more closely and we will mail out a request for your child to get three early morning samples to check
if it is a consistent result. On your appointment letter there is instructions about getting a sample from the first urine of the day.
When do I get the results?
Your endocrinologist will go through the results with you at your next appointment.
This page is still being updated, please check back at a later date