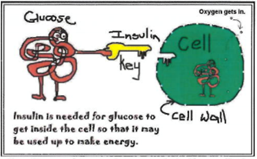
Insulin is the hormone needed to move the glucose from the bloodstream into the cells. It is the “key” which opens the door of the cell, allowing glucose to flow inside. Almost every cell in our body needs insulin to let the glucose in. We must have insulin in our body all the times.
Insulin is a protein. If it was taken as a tablet it would be destroyed by the stomach acids, so it must be injected. There are different insulins and they work for different lengths of time. The insulin regimen you use will determine the insulin prescribed, and your doctor will
discuss the choice of insulin regimen with you. Your diabetes nurse educator and dietitian will provide you with the information needed to understand the insulin, how long it works and how food, exercise and insulin work together to affect your blood glucose levels. They will also teach you about “target” blood
glucose levels (4mmol/L – 7 mmol/L) and how best to achieve these.
The insulin regimen best suited for most children newly diagnosed with type 1 diabetes at the Royal Children’s Hospital (RCH) is multiple daily injections (MDI). At RCH your diabetes doctor will always prescribe injected insulin at diagnosis. Down the track, if you and your
family are interested in learning about insulin pump use, please discuss this with your doctor at diabetes clinic. They can arrange an appointment with a diabetes educator to further explore how the pump works and if it will suit you and your family.
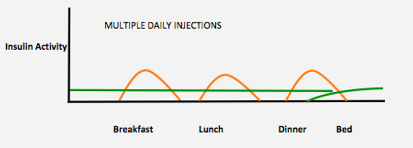
Multiple daily injections (MDI)
MDI is also known as ‘Basal Bolus’ insulin regimen. This regimen aims to mimic the body’s normal production of insulin. It requires you to give a dose of long-acting background (basal) insulin once a day (at the same time each day) and a dose of rapid-acting (bolus) insulin
before every main meal. This usually means you give 4 injections a day. The MDI regimen providesflexibility with timing of meals and
routine. Snacking between meals is generally not needed when using this insulin regimen and if large snacks are eaten, sometimes more insulin is needed.
Basal insulin (brand includes Optisulin® glargine) lasts for 24 hours. It is injected once per day, at the same time of day, and ensures there is insulin in the body all the time.
Bolus insulin (brands include NovoRapid®/Humalog®) lasts for about 3-5 hours. It is rapid acting and given before each main meal. This dose is matched to the amount of carbohydrate that is eaten. Rapid-acting insulin can be injected 3 or more times per day.
NovoRapid®/Humalog® take 15 minutes to start to work. Best practice means that rapid acting insulin needs be injected15 minutes before starting to eat.
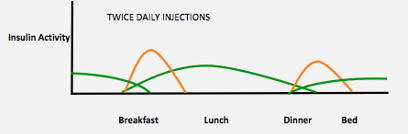
Twice daily insulin
Twice daily insulin requires an injection of both rapid and an intermediate / long acting insulin before breakfast and before dinner. This type of insulin regimen is less flexible compared to multiple daily injections because it requires insulin injections and meals to be at the same time each
day. It also means the quantity as well as timing of meals needs to be a consistent routine each day.
Twice daily insulin uses a rapid acting insulin e.g. Novorapid®/Humalog® with an intermediate/long acting insulin e.g. Levemir®/Humulin® NPH.
NovoRapid®/Humalog® takes 15 minutes to start to work. Best practice means that injections are given 15 minutes before starting to eat.
Sometimes, the doctor may prescribe an already premixed insulin. This is also injected before breakfast and dinner. The rapid and long acting insulin mix is pre-determined so meal timing and quantity must be strictly adhered to and is only used if the above insulin regimens aren’t
working for you.
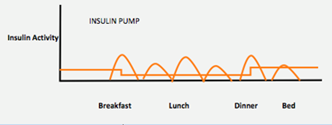
Insulin pump therapy
The insulin pump is a small battery device filled with a cartridge of rapid acting insulin. As the body must always have insulin in the body, it is worn 24 hours a day. Before eating, the user needs to enter the total grams of carbohydrate to be eaten and
the pump will deliver an insulin dose. The user also needs to enter at least 6 BGLs into the pump so enough insulin is delivered to keep the blood glucose level in target range.
The delivery of insulin is via small plastic tubing (line) which is connected to a fine metal or plastic needle (cannula) which is injected through the skin and is kept in place by a sticker. The line, cannula and insulin is changed every 2–3 days. There are
benefits and challenges to using an insulin pump and they are not right for everyone.
For further explanation about insulin pumps, the process for appointments and the required education to start on a pump at RCH see the
diabetes technology section on our website
.