Table of contents will be automatically generated here...
As the year progresses, we will keep building on this resource for managing diabetes on different special occasions!
Ramadan
Ramadan information
Passover
Passover is a Jewish festival that is observed and
celebrated over 8 days. It is a festival where food eaten is affected. During
Passover, all leaven, whether
in bread or other mixtures, is prohibited, and only
unleavened bread, called matzo, may be eaten.
A Sedar is held on the first
two nights of Passover.
The following tips can be viewed to manage your
diabetes within this time where different foods are eaten.
Planning
Remember, Passover is a time of celebration and coming
together with your family and friends. You may see more swings in your glucose
levels over the festival. Remember no-one is perfect and not everyone can keep
their levels within the target range at all times.
However, some planning
around the foods that you will eat (and likely eat at the same time each year)
can help keep your levels in range as much as possible.
Tips for planning and getting ready for Passover:
- Families often have their own
traditional recipes over the Passover period. Take some time to look at these
recipes to work out the carbohydrate content in these meals. Utilise apps in preparation,
such as Easy Diet Diary®. The Easy Diet Diary® app allows you to build a recipe
and will help with your carbohydrate counting. Save these calculations for the
years to come.
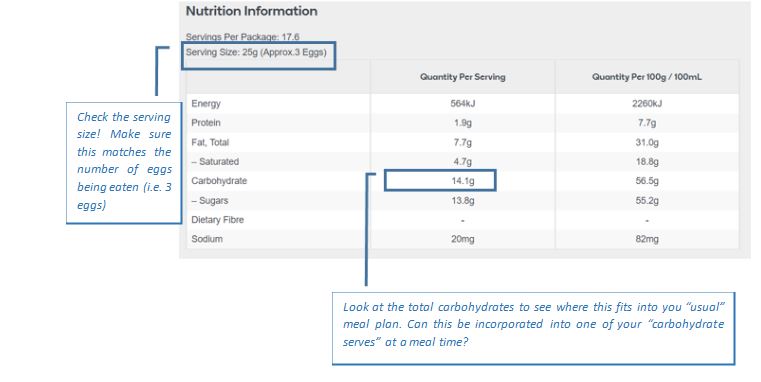
- For packaged products, read the
label.
For example, Sniders Matzah Meal – 1
serve is 25 grams and contains about 18 grams of carbohydrate or 1 serve.
Matzah: 1 piece of Matzah is about 25
grams of carbohydrate (about 2 serves of carbohydrates)
- Matzah is classified as a High
Glycaemic Index (GI) food. When eating matzah aim to always include nutritious
fats and proteins. This can help prevent rapid rises in your BGLs. For example,
toppings for your matzah may include avocado, cheese, eggs and meats. Try to
avoid sweet spread toppings.
- Passover packaged foods such cereals,
desserts and snacks may also have a higher GI due to the added sugar that is often
found in them. Make sure you take your insulin 15 minutes before starting to
eat and consider adding foods as discussed above (also included in this is adding milk to your ceral) to help prevent bigger rises
in your glucose levels.
.JPG)
Managing with different insulin regimens:
Remember,
however you get your insulin, and whatever the celebration, carbohydrate
counting is key, take the time to count correctly, speak with your team to get
extra help as needed and enjoy your celebrations!
You may need to make insulin dose changes over the holiday period. With having a different routine over the holidays and eating different foods for Passover, your insulin doses may need to change e.g. you may need more/less insulin to cover a meal. See dose adjustment guidelines on when and how to change your insulin doses. You may then need to change back to your original doses when Passover is over and your return to school.
Fixed dose insulin injections
If you have a fixed dose of insulin and eat a fixed amount of
carbohydrate with your meals make sure to:
- Incorporate your Passover treat carbohydrates into you mealtime
carbohydrate allowance. This might mean eating less savoury carbohydrates to
accommodate for a dessert
- Introduce an additional injection between meals to allow for
large, between meals snacks. Please discuss this with your diabetes educator if
you haven’t done this before.
Dosing cards or dosing app with insulin injections
Using an app or dosing cards help you adjust your insulin dose
based on the amount of carbohydrates you are eating and your current glucose
level. Some cards/settings in the app recommend different insulin doses for
different times of the day.
If you are eating extra food between meals, you can use your
dosing card or app to give an extra insulin injection.
Make sure to:
- Use the meal time recommendation on your card closest to that
time of day
- DO NOT include any correction dose with the extra
injection
- Make sure there is at least 3 hours between each of your meal
time injections
Insulin pump therapy
Remember to count
the carbohydrates and bolus for all of them.
For Control IQ® consider setting another insulin profile to support the algorithm working off adjusted settings for this time period where your routine is different
Temporary Basal Rate
(TBR) - If you can set a TBR (not using Control IQ® or SmartGuard®)
- Consider increasing your TBR
for the Sedar nights. Sitting sedentary for a long period could cause your
glucose levels to go up. You might try an increase of ~ 10-20%
Easter
Easter is all about having an egg-cellent time. It is a time of celebrations with family and food and your diabetes management shouldn’t get in the way of enjoying yourself. Indulging in some chocolate and hot cross buns is often part of the tradition. Not being able to eat chocolate if you have diabetes is a myth, but some moderation, awareness of what you are eating and carbohydrate counting is important.
Here are some tips to help you hop right into the holiday period:
No one is perfect: Don’t be too hard on yourself. This is an occasional not a daily occurrence and you might see more swings in your blood glucose levels (BGLs). Remember all information is good information, even if you notice that after a meal or Easter egg hunt your BGLs aren’t where you thought they would be. Think about the carbohydrates you’ve eaten and when and how much insulin you gave. If your glucose readings are high, use this as an opportunity to discuss with parents or your diabetes team what did and didn’t work and learn some tips for next time.
Plan ahead: Where possible plan your day. Make sure to still have regular meals, as this will help stop hunger taking over when the treats come out. Think about when the Easter Bunny or Bilby usually comes to visit, and when these treats might be eaten. Incorporating the additional carbohydrates into your meal can be helpful and avoiding the need for additional injections. Check out the dosing section at the end, to see how to manage extra carbohydrates eaten based on your insulin regimen.
Know your carbohydrates
Quality: Not all chocolate is the same. Dark chocolate is often praised as being a better choice, but Easter is about having a treat. You might see “Diet or “No Added Sugar” chocolates, but this usually means artificial sweetener has been used instead. Like standard chocolate, these products are generally still high in saturated fat, so why not pick something you will enjoy?
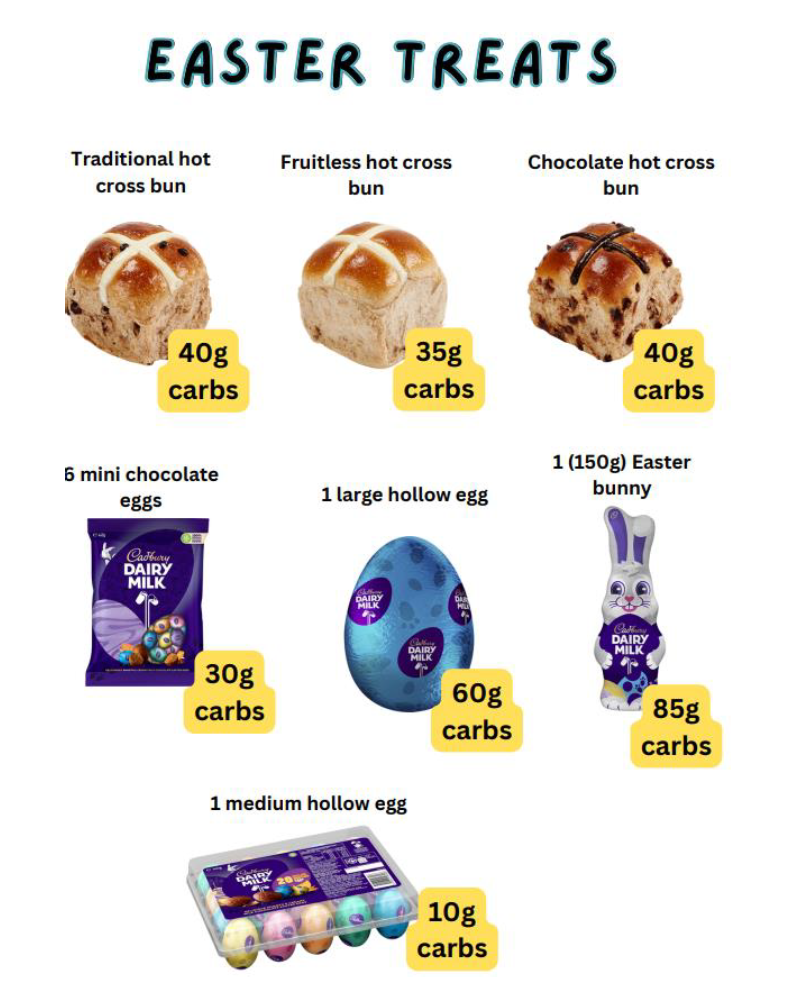
Quantity: Moderation will help prevent overindulging, particularly outside of meal times. When selecting your Easter eggs think about the portion size. Instead of going for the biggest egg on the shelf try selecting a couple of smaller ones. Smaller amounts of carbohydrate will ease ebbs and flows in glucose levels, help with the accuracy of your carbohydrate counting - you’ll also get to enjoy your Easter chocolate supply for longer!
When looking to count carbohydrates, the nutritional information panel will provide you with everything you need to know!
A guide to Easter treats!
Get creative: It doesn’t have to be all about chocolate. Try adding non-food gifts into the celebrations.
For example: fill some hollowed plastic eggs with arts and craft supply to make your own Easter hat! There are lots available to search online – try entering “Easter plastic egg” or “colourful plastic Easter eggs”

Incorporate activity: being active is beneficial for both mental and physical health. It is recommended for all children to have 60 minutes of activity most days of the week, and Easter is no expectation. With exercise, the body uses insulin more efficiently, so if you have diabetes, glucose levels generally lower with exercise. If needed, we suggest eating ~ 10 grams of low glycaemic index (GI) carbohydrate (activity food) before or during physical activity, and a few small Easter eggs could be used for this. Doing a bit more exercise during Easter celebrations will allow for some extra activity food to be eaten; maybe think about walking to the local park before starting the Easter egg hunt, or play a game of capture the egg (flag) with the extended family. Most importantly, like always with physical activity, make sure to monitor your BGLs, and carry hypo treatment on you. Please remember, chocolate is not first line hypo treatment, but could be used as a follow-up carbohydrate.
Working out your insulin dose
Insulin dose, the time it’s given and the types of carbohydrate eaten all play a role in what your BGLs is 3-4 hours later. Fast acting insulin takes around 15 minutes to start working, so aim to give it 10 -15 minutes before eating. The carbohydrate content you are eating ideally determines your insulin dose, so carbohydrate counting is key, but also, what comes with the meal is also important. Fats and proteins can slow down the glucose rise, which is why chocolate has a lower GI than standard sweets and lollies. Have a look at the nutritional information on the wrapping to work out matching insulin and carbs, and speak with your diabetes team if you are needing help with this.
Here are some suggestions about adjusting insulin for both insulin pump use and injection use:
Using an Insulin Pump (CSII)
Remember to count the carbs in the chocolate you are eating and bolus for it!
Temporary Basal Rate (TBR) - If you can set a TBR:
Consider increasing your TBR if the excitement of the day causes glucose to be above target range. You might try an increase of ~ 10-20%;
Consider decreasing your TBR if you will be more active than usual. You might try a reduction of ~ 10-20%
Extended Bolus
Your dietitian may have spoken to you about extended boluses. They can be used with meal boluses if eating low GI food or if the meal will be eaten over a long period of time to allow the delivery of insulin to match the release of glucose into the blood stream.
Using injections
Using Dosing Cards
These are usually provided by your diabetes team and help you adjust your insulin dose based on the amount of carbohydrates you are eating and your current blood glucose level. Some cards recommend different insulin doses for different times of the day.
If you are eating extra food between meals, you can use your dosing card to give an extra insulin injection.
Make sure to:
Use the meal time recommendation on your card closest to that time of day
DO NOT include any correction dose with the extra injection
Make sure there is at least 3 hours between each of your meal time injections
Giving fixed insulin doses
If you have a fixed dose of insulin and eat a fixed amount of carbohydrate with your meals make sure to:
Incorporate your Easter treat carbohydrates into you mealtime carbohydrate allowance. This might mean eating less savoury carbohydrates to accommodate for a hot cross bun or Easter egg at the end of the meal
Introduce an additional injection between meals to allow for large, between meals snacks. Please discuss this with your diabetes educator if you haven’t done this before.
Consider splitting your meal-time insulin dos
Meals eaten during times of celebrations can take longer and may be more mixed in type (i.e. protein, fat, carbohydrates). If your meal is of a long duration, you might find it helpful to split you meal time dose.
Try:
Eg: if you normally give 10 units of insulin with your meal, give 5 units 10 -15 minutes prior to eating and 5 units around 1 hour into the meal.
Please remember, however you get your insulin, and whatever the celebration, carbohydrate counting is key, so take the time to count correctly, speak with your team to get extra help as needed and enjoy your celebrations!
Halloween
Whether it is a trick or a treat that you are looking for this Halloween, it is important to know how to manage your diabetes care on the most Ghoulish night of the year!
Safety first
Whether it is a house, street, or neighbourhood event, it is important to keep safe this Hallows Eve.
- Stay in a group
- Watch for traffic
- Don’t take or eat lollies that aren’t in their original wrapping
Quick tips for diabetes care
Your blood glucose can really swing when you’re having fun! Here are a few quick tips to help make sure you are prepared:
- Make sure that your insulin pump, CGM or flash glucose monitor can be accessed under your fang-tastic outfit
- Have your diabetes supplies on you
- Tell a friend about your diabetes, and how what to do if you have a hypo
- Trick or treating is exercise! Your insulin needs could change if you are doing more walking than you normally do. Remember this if you are injecting or making adjustments on your pump.
The treats
- Remember to carb-count the sweets you’ve eaten!
- Have your diabetes supplies on you
- If there is an option opt for Chocolate, as it has a lower glycaemic index than other sweet treats like snakes, and skittles
- Spread you treats, do not eat all your goods at once. Keep them for the weeks to come as a lunch time snack, or for post dinner treat.
Below are some common treats that might end up in your pumpkin:

Credit: Adapts from Children and Young People’s Wales Diabetes Network Halloween Leaflet
Updated October 2022