* Approved by CPG Committee; PIC endorsement pending
See also
Gastrooesophageal reflux disease in infants
Non-IgE mediated food allergy
Slow weight gain
Child abuse
Recognition of the seriously unwell neonate and young infant
Key points
- Crying is a normal part of infant communication and reflects a range of physical, emotional and developmental needs, which can vary in frequency and intensity over time
- Assessment aims to exclude medical conditions, inflicted injury or parental mental health concerns
- Management focuses on education, reassurance and shared decision making to develop a supportive and individualised approach
- Avoid medications due to limited evidence of benefit and potential for harm
Background
- Crying typically peaks at 6-8 weeks of age, averaging 2-3 hours/day
- Families often receive diverse and conflicting advice, which can be challenging to navigate
- A range of settling approaches exist, from structured to flexible, which may complement one another, to suit the individual infant and family
- The term 'infant colic' has traditionally described excessive crying but is now considered unhelpful, as it inaccurately implies an abdominal cause
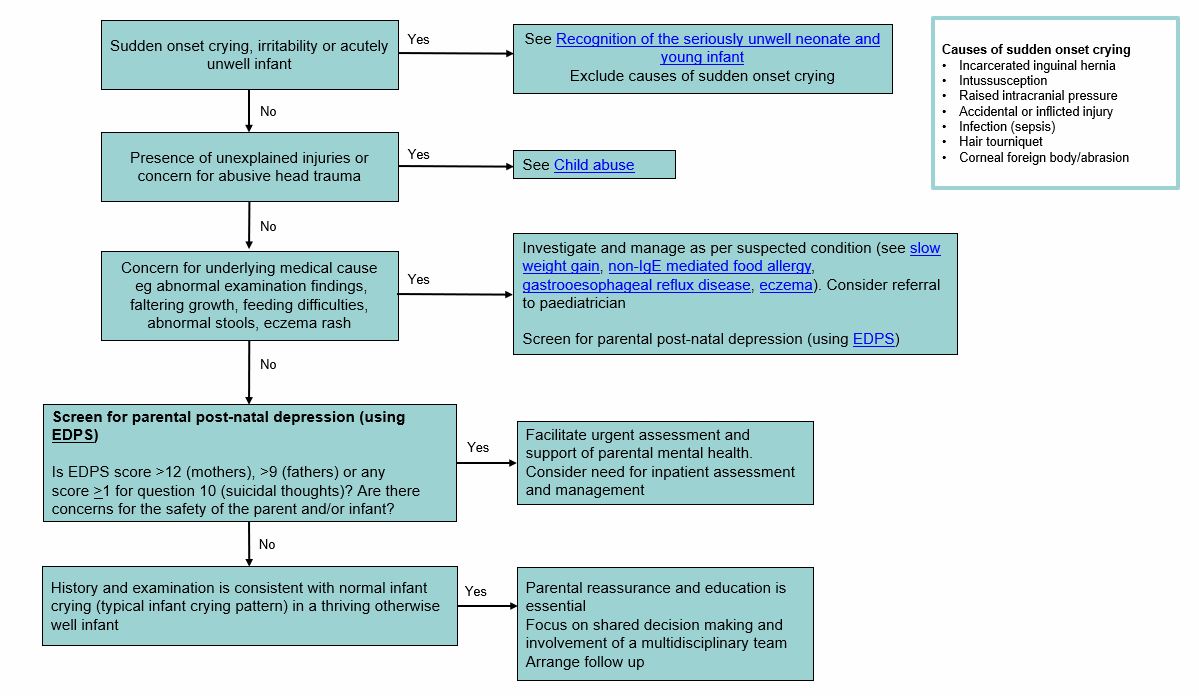
Assessment
The assessment of a crying or unsettled infant aims to
- Identify red flags and exclude medical/traumatic causes
- Evaluate parental mental health, support systems, and parent-infant interactions
- Determine if crying pattern is developmentally normal and/or related to communication of common infant needs eg hunger, discomfort, sensory input, or need for comfort
History
- Pregnancy and birth history
- Feeding patterns
- Sleep-wake patterns
- Growth and development
- Current strategies, treatments and support services
- Family and social context
- Parental/carer mental health
Examination
Assess for physical signs of illness, injury or pathology contributing to unsettled behaviour
Red flags
- Sudden onset irritability and persistent crying
- Features of an acutely unwell infant. See Recognition of the seriously unwell neonate and young infant
- Faltering growth, feeding difficulties, oral aversion
- Rapid head circumference growth crossing percentiles
- Unexplained injuries
- Excessive crying is a risk factor for abusive head trauma (previously known as shaken baby syndrome) See Child abuse
- Parental post-natal depression (PND) and social isolation
- Screen for PND using the Edinburgh Postnatal Depression Scale. See Additional Notes for other languages
- Concern if score >12 (mothers), >9 (fathers) or any score >1 on question 10 (suicidal thoughts)
Consider if sudden onset crying
Other causes to consider in assessment
Typical infant crying pattern
Babies cry to communicate a broad range of physical, emotional and developmental needs. It is best understood as proximity-seeking communication, the expression of a need for physical and emotional closeness with a caregiver
There is a wide range of unsettled or crying behaviour that is considered typical (in an otherwise well and thriving infant)
- Increases to a peak at 6-8 weeks and improves by 3-4 months (see graph below)
- Often worse in the late afternoon/evening, may last hours, can be resistant to soothing
- Night waking is normal for infants
<12 months of age
- Breastfed infants often engage in cluster feeding during growth spurts, particularly in the evening (helps regulate breastmilk supply to meet the infant's changing needs)
- Some babies strain, cry, grunt and go red in the face, before passing soft stools (also known as infant dyschezia). This is a common and self-resolving difficulty in coordinating increased intra-abdominal pressure with relaxation of the pelvic
floor required to pass stool
Curves of early infant crying

Management
Investigations
If history and examination is consistent with typical infant crying patterns, no investigations are required
Management approach
Once red flags and medical causes are excluded, parental reassurance and education are essential.
- If screening for postnatal depression raises significant concerns, or there are concerns for the safety of parent and/or infant, urgent mental health assessment and support should be facilitated
Focus is on shared decision making and involvement of a multidisciplinary team eg lactation consultant, child health nurse, GP, paediatrician, perinatal mental health or infant mental health service, and parenting support services
Where possible, allowing time for the following discussion points can be highly effective for the infant and family's care
- Acknowledge the challenges and validate caregiver concerns
- Explain that underlying causes have been considered and give reassurance regarding normal examination, growth and development
- Provide an explanation of typical infant crying patterns and variability. Share resources (eg PURPLE crying) that describe normal crying behaviours as an important form of infant communication
- Address parental mental health and stress levels, identify protective support systems, provide resources and early referral
- Offer practical strategies (see below), ongoing support and early follow-up. Encourage caregivers to flexibly explore settling strategies that align with family values and infant developmental stage and temperament
Treatment
Medication, supplements and interventions are often sought by families. Often these are not indicated, have no evidence and can cause harm
| Intervention |
Details |
| Feeding-related interventions |
Breastfeeding support (provided by lactation consultant) is useful for assessment and optimisation of latch, attachment, milk transfer and feeding effectiveness
Flexible, on-demand feeding is associated with improved infant regulation and reduced parental stress
Maternal dietary and/or formula changes rarely reduces infant distress, except when a non-IgE mediated food allergy is suspected. Introducing formula or solid foods does not improve infant sleep or crying
Bottle and teat changes are usually ineffective |
| Probiotics |
There is emerging evidence to support probiotic use for exclusively breastfed babies
<3 months
- Lactobacillus reuteri DSM 17938 (only strain shown to be effective): 5 drops/day PO for 21 days |
Acid suppression medications
eg proton pump inhibitors, H2 receptor antagonists |
Not effective for infants with physiological reflux, irritability or unsettled behaviours |
| Simethicone eg InfacolTM |
Not effective, possibly harmful |
| Herbal 'colic' mixtures eg gripe water |
Not effective, possibly harmful |
| Anticholinergic medications eg dicyclomine, cimetropium |
Risk of significant harm (drowsiness, apnoea, seizures) associated with belladonna toxicity |
| Spinal manipulation |
Not effective, risk of significant harm |
Lingual frenotomy
(tongue-tie release) |
Most infants with a short lingual frenulum (aka tongue tie) have no functional limitations and require no intervention
If feeding is ineffective, assessment by trained professional eg lactation consultant, midwife, speech pathologist is essential. First-line treatments include improving breastfeeding positioning, latch and feeding frequency
|
Consider consultation with local paediatric team when
- Medical cause of crying identified or suspected
- Infant clinically unwell
- Concerns for inflicted injury or significant parental mental health concerns
Consider transfer when
- Infant requiring care beyond the comfort level of the hospital
- Parent requiring care beyond the comfort level of the hospital (inpatient mental health support)
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
- Medical conditions, inflicted injury, and parental mental health concerns have been excluded or appropriately addressed
- Families have been provided reassurance, education, resources and referral for early ongoing support
Options for ongoing support include
- Maternal and child health nurse, including state based enhanced/extended programs
- General practitioner
- General paediatrician
- Lactation consultant
- Perinatal mental health clinician
- Infant mental health clinician
- Parent and family support services (state specific)
- Early parenting centre for sleep and settling support
- Parent-baby unit when close professional or inpatient mental health support is required
Parent information
Additional notes
Edinburgh Postnatal Depression Scale in other languages
Practical strategies
| Strategy |
Details |
| Self-care and support of parental mental health |
Encourage self-compassion, adjusting expectations, prioritising rest and nutrition and accessing support. Early referral to perinatal mental health services and supports if indicated |
| Prevention of abusive head trauma |
The peak period of infant crying is strongly linked to an increased risk of abusive head trauma (AHT). The Period of PURPLE Crying program offers evidence-based strategies
to help caregivers understand and manage this challenging stage safely and effectively |
| Prompt responsiveness to infant cues |
Responding sensitively to infant cues and crying has been shown to foster secure attachment, improve parental wellbeing, improve sleep and reduce infant crying |
Babywearing
(use of a carrier, sling or wrap that is worn on the caregiver's body) |
Convenient and allows caregivers to attend to tasks while soothing the infant. Use a carrier appropriate for the infant's age and development to ensure proper positioning for airway patency and hip health. Follow the TICKS safety rule
- Tight: carrier snugly supports the baby close to wearer's body
- In view: face is always visible
- Close enough to kiss: positioned high on the chest
- Keep chin off the chest: maintain a finger-width gap for airway safet
- Supported back: back is in a natural, supported position with tummy and chest against wearer
|
| Safe sleep |
Recommendations apply if using a cot/bassinet or if sharing a sleep surface with a caregiver
- Baby on their back
- On a firm, flat, level surface
- Head and face uncovered
- Clear space free of objects
A
risk minimisation approach can guide caregivers to make informed choices and reduce risks (see QH Safer Infant Sleep Guideline) |
| Varied sensory experiences |
Experimenting with a broad range of rich sensory experiences allows caregivers to find what may soothe and settle their individual baby
Examples include - Going outdoors eg lying on mat under trees, walk in pram or carrier
- Music, singing, white noise or alternative low level background noise
- Reading books, funny voices
- Wrapping, swaddling
- Bathing, water play
- Skin to skin contact with caregiver
- Rocking, patting, massage
|
*Last updated October 2025