See also
Unsettled or crying babies
Gastroenteritis
Key points
- Gastro-oesophageal reflux disease (GORD) should be differentiated from physiological gastro-oesophageal reflux, which is common in healthy, thriving babies and does not require specific investigations or management
- GORD is not a common cause of unexplained crying, irritability or distressed behaviour in otherwise healthy infants
- Empiric use of acid suppression for unsettled infants is not effective and may cause harm
- The natural history of GORD is of resolution with time; any therapy commenced should be reviewed regularly
Background
Gastro-oesophageal reflux (GOR) is the passage of gastric contents into the oesophagus, often with effortless vomiting, or 'possets'. It is a physiological process that occurs several times a day in healthy infants.
Gastro-oesophageal reflux:
- is common, affecting at least 40% of infants
- usually begins before 8 weeks of age, peaks at 4 months and resolves by 1 year of age in majority of cases
- does not cause crying and irritability in healthy infants. Infant crying peaks at 6-8 weeks, and hence some babies with simple GOR may also be unsettled
- rarely require investigations
- can usually be managed with parental education, support and anticipatory guidance
There is insufficient evidence to support the diagnosis or management of "silent reflux"
Gastro-oesophageal reflux disease is when GOR causes vomiting with:
- refusal to feed
- pronounced irritability with feeding
- aspiration
- chronic cough, wheeze
- slow weight gain
- haematemesis
Cow
milk protein allergy (CMPA) can present with similar symptoms to GORD
- Blood and/or mucous in stool, chronic diarrhoea or atopic risk factors make this diagnosis more likely.
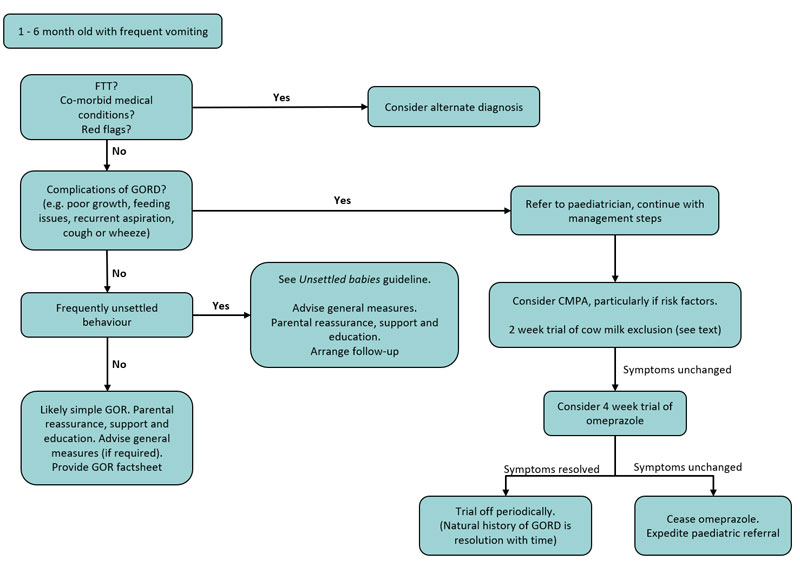
See Flow Chart below.
Assessment
- Both GOR and GORD can be diagnosed on detailed history and examination
- Direct observation of a feed by an experienced clinician can be particularly useful to identify exacerbating factors
Reconsider diagnosis if any
of the following red flag features are present:
Symptoms
- Vomiting that is bilious; has onset >6 months of age; or is consistent and forceful
- Significant diarrhoea or constipation
- Fever or lethargy
Signs
- Abdominal rigidity
- Hepatosplenomegaly
- Bulging fontanelle and/or increasing head circumference
Management
Investigations
Investigations for GORD (such as barium contrast radiography, pH probe, endoscopy) are rarely necessary, and are not diagnostic. Investigations should only be considered on an individual basis after the patient has been assessed by a paediatrician.
Treatment
Simple GOR can cause considerable parental distress, and requires reassurance, support and anticipatory guidance. General measures may minimize symptoms.
General measures
Positioning
- Holding the infant in a head elevated position for 20–30 minutes after feeding may reduce GOR
- Prone sleeping or inclining the sleep surface is not recommended in infants due to the risk of SIDS
Thickened feeds
- In bottle fed babies, thickened feeds may reduce frequency of vomiting
- "Anti-reflux" formulas are pre-thickened, or alternatively a thickening agent can be added to a standard formula or expressed breast milk
- Thickened feeds can contribute to constipation
- Ensure the infant is not being given sodium alginate (Gaviscon Infant®) as co-administration increases risk of bowel obstruction
Optimise feeds
- Observation and assessment of feeds by an experienced lactation consultant or Maternal Child Health Nurse (MCHN) can be helpful
- Assess feed volumes in formula fed infants to identify overfeeding. Reducing feed volumes can reduce regurgitation but should only be considered if excessive for infant's weight. Consider a trial of smaller, more frequent feeds in these infants if practical
- GOR alone is not an indication to change formula or stop breast feeding. One particular brand of standard cow milk formula does not confer benefit over another, nor do they vary in their content of dairy
Specific
measures for GORD
Consider
cow milk protein exclusion
- Up to 40% of infants presenting with symptoms of GORD will have non-IgE mediated Cow Milk Protein Allergy (CMPA)
- Symptoms usually occur within a few weeks of exposure to cow milk protein
- There are no specific distinguishing features that can predict response to dietary modification, nor are any investigations helpful in CMPA
- Where CMPA is suspected, the infant should have a 2 week trial of strict cow milk protein elimination from their diet and referral to a paediatrician arranged
- Breast fed infants require strict
maternal dairy avoidance
- Formula fed infants require extensively hydrolysed formula, obtained via prescription from a paediatrician. Over the counter formula options include Novalac Allergy® or Aptamil Allerpro®
Consider
acid suppressant therapy:
Acid suppressant therapy may be indicated in specific patients with GORD (see flow chart). When commenced, it should be instituted as a four week trial. Omeprazole, a proton pump inhibitor (PPI), is the recommended agent:
- omeprazole:
<10 kg: 5 mg once daily
- omeprazole takes 4 days to reach maximum effect
Studies have indicated that PPI therapy may lead to an increased risk of:
- increased risk of community acquired pneumonia
- increased risk of gastroenteritis
- increased future fracture risk
- micronutrient deficiencies
There is no evidence to support empiric use of acid-suppressant therapy as a diagnostic trial for irritable infants
It is important to review ongoing therapy and cease at 4 weeks if no benefit
Surface
agents
Surface agents such as sodium alginate (Gaviscon infant ®) increases viscosity of gastric contents and can reduce episodes of visible regurgitation. There is little information available on efficacy and long-term use in infants is not recommended
Management flowchart
Surgical treatment
Surgical approaches (eg fundoplication) are reserved for children who have intractable GORD symptoms unresponsive to medical therapy or with significant complications
Consider consultation with local paediatric
team when
- Red flag features present
- Infant clinically unwell
- GORD not responding to initial management, or commenced on acid suppressant therapy
Consider transfer when
Child requiring care beyond the comfort level of the hospital
For emergency advice and paediatric or
neonatal ICU transfers, see Retrieval
Services
Parent information
Additional notes
REducing MEDications in Infants (REMEDI)
Last updated October, 2019