See also
Intravenous immunoglobulin
Febrile child
Sepsis – assessment and management
NB Cases of PIMS-TS – a novel post infectious systemic hyperinflammatory syndrome – have been reported in children in Victoria.
See alert
Key points
- Kawasaki disease (KD) is a clinical diagnosis that requires prompt recognition and management
- Consider incomplete KD where there is prolonged fever and no alternative cause found
- Infants and adolescents may present with incomplete KD and are at particularly high risk of developing coronary artery aneurysms
- Early treatment with intravenous immunoglobulin (IVIg) has been shown to reduce morbidity and mortality
Background
KD is the second most common vasculitis in childhood after Henoch Schönlein purpura, and is the most common cause of acquired heart disease in children in high-income countries. Lack of appropriate treatment leads to coronary artery aneurysms (CAA) in approximately 25% of cases.
- Worldwide distribution, although more common in Asian children
- Approximately 75% of cases occur under 5 years of age
- Less common in children
<6 months and >5 years; however these children are more likely to develop CAA
- Can present without all diagnostic criteria (see flowchart below) which can present a significant diagnostic challenge
Assessment
History
Physical findings can present sequentially over a number of days, thus history should include asking about diagnostic features that may have resolved by the time of presentation
Examination
Kawasaki disease: Diagnostic criteria
Fever persisting for 5 days, PLUS 4 of the 5 following criteria:
- A diagnosis earlier than 5 days can be made with a typical presentation in consultation with an experienced clinician
- KD can be diagnosed with less than four of the following features if coronary artery abnormalities are present
|
|
Criterion |
Features |
|
Conjunctival injection
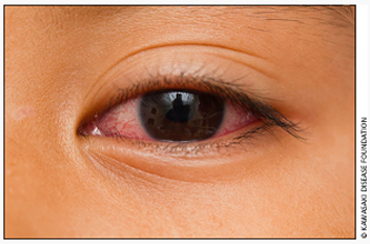 |
Bilateral, non-exudative, painless. Often with limbic sparing (zone around the iris is clear) |
|
Rash
 |
Erythematous polymorphous rash occurs in the first few days, involving trunk and extremities
Variable presentations, most commonly maculopapular, erythema multiforme-like or scarlatiniform
Bullous, vesicular, or petechial rashes are not typical in KD |
|
Oral Changes

 |
Strawberry tongue
Erythema, dryness, cracking and bleeding of the lips
Diffuse oropharyngeal erythema
Exudates are not typical of KD |
|
Extremity changes
 |
Hyperaemia and painful oedema of hands and feet that progresses to desquamation from the second week of illness |
|
Lymphadenopathy
 |
Cervical, most commonly unilateral, tender. At least one node >1.5cm. Less common feature and seen in older children |
|
Photographs used with permission from the Kawasaki disease Foundation, Inc |
Common findings in addition to the diagnostic criteria include:
- neurological: irritability, aseptic meningitis
- GIT symptoms: abdominal pain, vomiting, diarrhoea, gallbladder hydrops
- arthralgia / arthritis
- dysuria
- inflammation at recent (within 6 months) BCG vaccination site
KD is a medium vessel vasculopathy; any organ system can be affected
Incomplete Kawasaki disease
Consider in a child with a clinical presentation suggestive of KD but not meeting the full diagnostic criteria
- Requires abnormal investigation results to support the diagnosis (see flowchart)
- Infants and adolescents often present with an incomplete picture and are at a higher risk for cardiac complications
Consider incomplete KD in:
- A child with fever for at least 5 days combined with 2 or 3 of the principal clinical features OR
- An infant with one/more of the following features:
- fever ≥7 days +/- irritability without other explanation
- prolonged fever and unexplained aseptic meningitis
- A child or infant with prolonged fever and:
- shock
- cervical adenitis not responsive to oral antibiotics
- Incomplete KD can present a significant diagnostic dilemma, however once the diagnosis is made, the treatment for KD and incomplete KD is identical
Incomplete Kawasaki disease
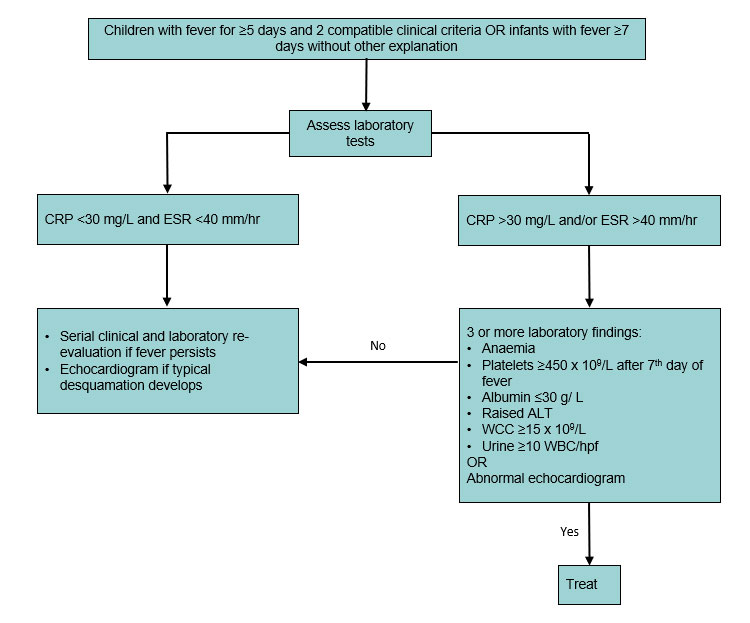
Adapted from the American Heart Association (2017).
Differential diagnosis
- Group A streptococcal infections: tonsillitis, scarlet fever, acute rheumatic fever
- Viral infections including EBV, CMV, Adenovirus, HHV-6, SARS-CoV-2
- Systemic juvenile idiopathic arthritis (JIA)
- Sepsis
- Toxic shock syndrome (staphylococcal or streptococcal)
- Stevens-Johnson syndrome
- Drug reaction
- Malignancy
Management
Investigations
There is no diagnostic test for KD. Laboratory tests provide support for diagnosis, assessment of severity, and monitoring of disease and treatment
- Echocardiogram: discuss with cardiology specific timing of initial and follow-up studies. Suggested schedule:
- At presentation (this should not delay initiation of treatment)
- 2 weeks
- 6 weeks
Coronary artery lesions should be managed in consultation with paediatric cardiology and haematology services
- In all patients consider:
- FBE, CRP, ESR, UEC, LFT (note ESR result unreliable after IVIg administration)
- Blood culture
- ASOT
- Serum to store (prior to IVIg administration)
- Urinalysis and culture (sterile pyuria)
-
COVID-19 swab
- ECG
Common abnormalities include elevation of ESR, CRP and neutrophils. Thrombocytosis is common in the second week of illness.
Treatment
- INTRAVENOUS IMMUNOGLOBULIN (IVIg): 2 g/kg as a single IV infusion on diagnosis
- IVIg should be given within the first 10 days of illness but should also be given to children diagnosed after 10 days if there is evidence of ongoing fever and/or inflammation
- A second dose of 2 g/kg IVIg should be given to children who do not respond to the first dose, as demonstrated by persistent or recurrent fevers 36 hours after the end of the first IVIg infusion. Seek specialist advice
- The National Blood Authority and BloodSTAR coordinate and authorise the use of blood products. IVIg is a product that must be ordered via their
website
- Haemolytic anaemia is an uncommon but recognised adverse effect of IVIg infusion, particularly for children receiving multiple doses. It typically occurs up to a week after IVIg administration
- Post IVIg vaccination: live vaccines (eg measles and varicella) should be deferred after IVIg administration, see the
National Immunisation Handbook. If the child is at high risk of measles, vaccinate and re-vaccinate after the appropriate period
-
ASPIRIN : 3-5 mg/kg orally as a daily dose until normal echo on follow up (minimum 6 weeks)
- There is minimal risk of Reye syndrome with low-dose aspirin
- Avoid non-steroid anti-inflammatory medications whilst on aspirin
- CORTICOSTEROIDS:
- Evidence for indication and optimal dose/duration of adjunctive steroids in the primary treatment of KD is limited
- Corticosteroid use in KD should be considered in consultation with specialist advice
- Consider use in high-risk groups which include
- Demographics: age
<12 months of age, Asian ethnicity
- Investigation abnormalities: ALT >100 IU/L, albumin ≤30 g/L, sodium ≤133 mmol/L, platelets ≤30 x 109/L, CRP >100 mg/L, anaemia for age
- Cardiac or coronary artery involvement on echo at presentation
- ADDITIONAL TREATMENTS: A number of therapies are available for consideration in patients who are not responsive to initial IVIg. These options should only be used in consultation with local paediatric specialists and include biological medicines such as infliximab
Consider consultation with local paediatric team when
- Kawasaki disease is suspected
- Child does not respond to initial treatment
Consider transfer when
- Child has cardiac involvement or timely echocardiography is unavailable locally (in consultation with the paediatric cardiology team)
- Children requiring care above the level of comfort of the local hospital
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Consider discharge when
- Afebrile and well at least 36 hours after treatment
- Children are on a daily dose of aspirin (see treatment point 2 above)
- A follow-up plan is in place including general paediatric review and repeat echocardiograms planned with cardiology
Parent information
RCH Kid’s Health Info:
Kawasaki disease
Sydney Children’s Hospital network fact sheets:
Kawasaki disease
Last Updated January 2021